A new multimodal neuroimaging study has revealed that people with systemic lupus erythematosus (SLE) may sustain silent but clinically meaningful brain changes even when they show no outward signs of neuropsychiatric involvement. The research indicates that structural alterations in both grey and white matter occur early and correlate with disease duration, organ damage and subtle cognitive decline.
Structural Brain Changes Detected Without Overt Symptoms
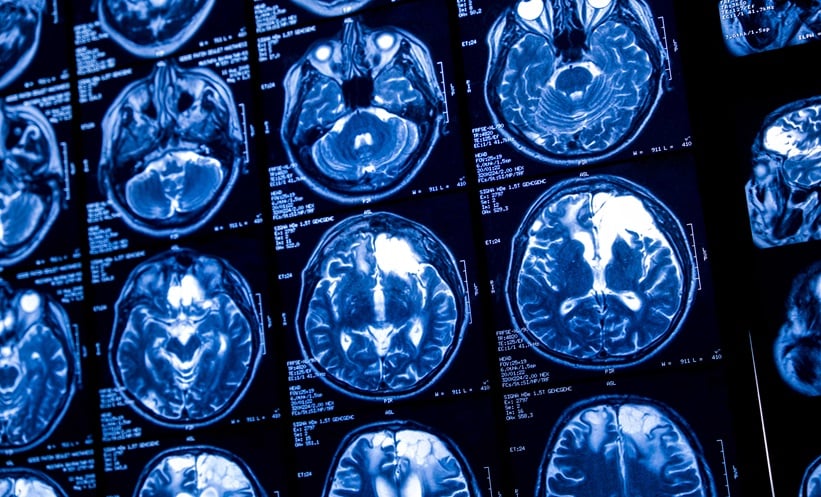
The study evaluated 30 patients with SLE who had no clinically apparent neuropsychiatric manifestations, alongside 34 healthy controls. Using high-resolution structural MRI, investigators found significantly reduced volumes in the right occipital lobe and left thalamus in the SLE group. These regions are important for processing visual information and regulating sensory pathways, suggesting that even symptom-free patients may already exhibit measurable neurological involvement.
Resting-state fMRI showed that global interhemispheric functional connectivity remained largely preserved. However, patients with moderate disease activity demonstrated reductions in connectivity within the frontal operculum and insula, areas linked to emotional regulation, attention and interoception.
White Matter Pathways Show Signs of Early Damage
Advanced diffusion tensor imaging (DTI) revealed widespread white matter disruption. Patients exhibited reduced fractional anisotropy (FA) in key pathways including the corpus callosum, right cingulum and brainstem. FA values declined progressively with increasing disease duration, particularly in the inferior fronto-occipital fasciculi and left cingulum.
Those with established organ damage showed even greater white matter impairment, indicating a cumulative effect of chronic inflammation on neural pathways. These findings provide new evidence that microstructural changes may precede overt neuropsychiatric lupus and could serve as early imaging biomarkers.
Cognitive Performance Linked to Disease Duration and MRI Findings
Neurocognitive assessments revealed that reduced white matter integrity correlated with poorer performance on tasks involving working memory, psychomotor speed and executive function. While participants did not report obvious neuropsychiatric symptoms, objective testing suggested a subtle decline that aligned with MRI abnormalities.
The authors conclude that structural and microstructural changes occur earlier and more frequently than previously recognised, even in patients categorized as having no neuropsychiatric lupus. They emphasise the importance of early monitoring, as these silent brain alterations appear to worsen with disease duration and may serve as early indicators of more significant neurological involvement.
Reference
Lee J et al. Multimodal brain structural and functional analysis in systemic lupus erythematosus patients without overt neuropsychiatric manifestations: associations with disease duration, organ damage, and neurocognitive function. Arthritis Res Ther. 2025;DOI: 10.1186/s13075-025-03640-6.