BACKGROUND AND AIMS
Pregnant women with dilated cardiomyopathy (DCM) face high risks of complications and maternal death due to haemodynamic overload, withdrawal of teratogenic but essential therapies, and limited treatment options during pregnancy.1,2
The purpose of this study was to evaluate maternal and fetal outcomes in women with DCM during pregnancy and up to 12 months postpartum across different aetiologies, and identify predictors of maternal death.3
METHODS
The prospective cohort of women with confirmed DCM were enrolled in the InCor Pregnancy and Heart Disease Registry for over 10 years. All received standardised cardio-obstetric care. Left ventricular ejection fraction (LVEF) was assessed using echocardiography, and brain natriuretic peptide was evaluated when available. Treatment during pregnancy included β-blockers, hydralazine, diuretics, nitrates, enoxaparin, and hospitalisation when needed. Guideline-directed therapy was resumed postpartum. Outcomes included maternal (heart failure, arrhythmias, thromboembolism, death) and obstetric/fetal complications. Logistic regression identified predictors of maternal mortality.
RESULTS
Among 983 registry patients (2013–2023), 90 had DCM. Cardiomyopathy aetiologies were peripartum (32), idiopathic (21), myocarditis (15), Chagas disease (11), and others (11). Maternal complications occurred in 51.1% during pregnancy, 36.0% in the early postpartum period (up to 6 weeks after delivery), and 38.6% in the late postpartum period (from 6 weeks–12 months after delivery; Table 1). All nine maternal deaths (10%) occurred postpartum, mostly due to heart failure, at a mean of 8.8±3.1 months (Figure 1). Caesarean section was performed in 75% of patients, with 10.0% fetal loss and 33.8% prematurity. Mean birth weight was 2,606 g. LVEF improved from 32% at diagnosis to 39% during pregnancy and 42% at 12 months postpartum. Lower LVEF (odds ratio: 0.87; p=0.006) and prior thromboembolism (odds ratio: 15.5; p=0.017) were independent predictors of death.
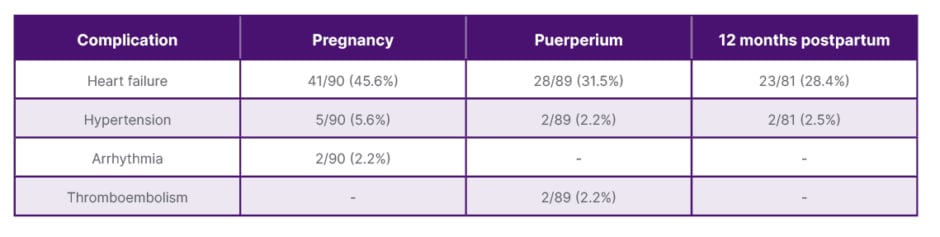
Table 1: Main clinical complications by follow-up period.
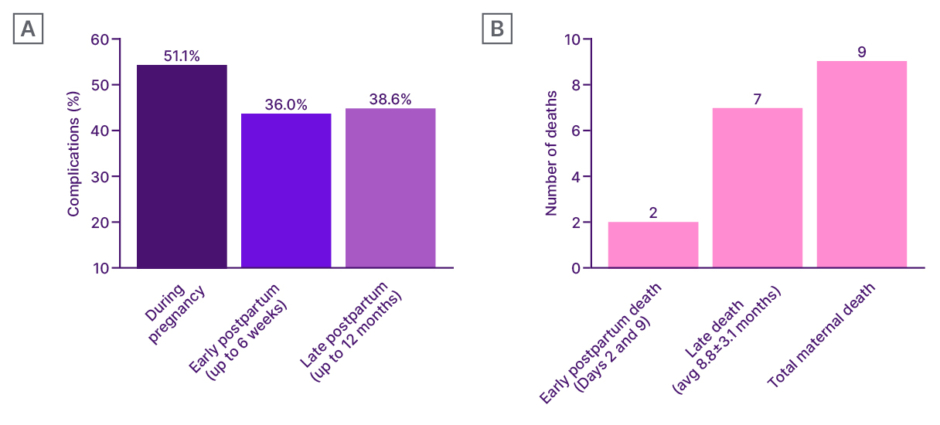
Figure 1: Incidence of maternal outcomes: complications and mortality.
A) Maternal complications. B) Maternal mortality.
avg: average.
CONCLUSION
Pregnancy in women with DCM was associated with high morbidity and late mortality. Reduced LVEF and a history of thromboembolism were independent predictors of maternal death.







