BACKGROUND AND AIMS
Do automated insulin delivery systems outperform systems requiring manual upload and adjustment?1 Automated insulin delivery (AID) systems are now widely used in paediatric diabetes care, with multiple systems recommended by international guidelines. Evidence consistently shows that AID improves HbA1c and time in range (3.9–10.0 mmol/L or 70–180 mg/dL), with systematic reviews confirming gains of 10–15% in children and young people, across both outpatient and real-world settings.2-4
METHODS
The authors compared the two categories of AID systems used in their centre: AutoAID (cloud-integrated, automated algorithm updates, e.g., MiniMed 780G [Medtronic, Dublin, Ireland], CamAPS FX [CamDiab Ltd, London, UK], Omnipod 5 [Insulet, Acton, Massachusetts, USA]) and ManualAID (static algorithms requiring user uploads and adjustments, e.g., Tandem Control-IQ [Tandem Diabetes Care, San Diego, California, USA]).
RESULTS
Users in both categories achieved clinically meaningful outcomes, with HbA1c reduced by approximately 6 mmol/mol and time in range increased by 12–15% at 12 months, despite two-thirds of the cohort falling into the most severe category of socioeconomic deprivation. This underlines a fundamental point: AID systems work well.
However, additional benefits for AutoAID users emerged regarding higher time in tight range (TITR; 3.9–7.8 mmol/L or 70–140 mg/dL) and onboarding efficiency. TITR is a strong predictor of long-term complications, with even a 5% gain linked to reduced retinopathy risk.5 The authors’ AutoAID users demonstrated an additional TITR improvement of approximately 4%, confirmed in mixed-effects modelling (Figure 1). This suggests that automatic algorithm updates and adjustable targets may offer additional advantages.
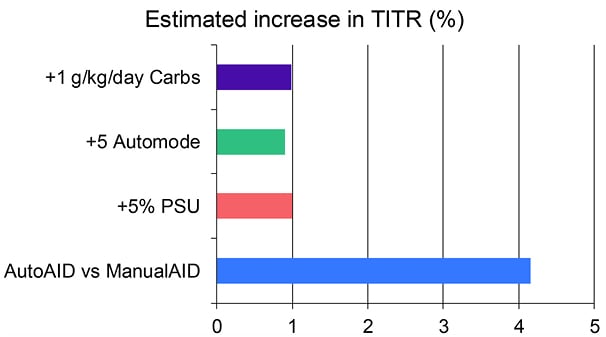
Figure 1: Independent predictors of time in tight range identified in mixed-effects modelling.
AutoAID use was associated with a 4.2% increase in TITR, while a 5% increase in sensor wear, 5% increase in automode use, and 1 g/kg/day higher carbohydrate intake were each associated with smaller, but significant gains. TITR was defined as 3.9–7.8 mmol/L (70–140 mg/dL).
PSU: percentage sensor usage; TITR: time in tight range; vs: versus.
Onboarding efficiency was another clear differentiation. AutoAID enabled 93% of families to onboard remotely compared to 52% of ManualAID, translating into a six-fold saving in both educator and family time. Automatic data uploads remove barriers such as lack of computer access, and enable remote support provision between clinic appointments, while ManualAID requires an active uploading process for this, potentially disadvantaging users like the authors’ deprived cohort. To achieve equity in diabetes care, this distinction matters: access and efficiency must not depend on socioeconomic status. Further studies will show whether auto-updating algorithms are inherently superior to manual ones. AutoAID recalibrates automatically based on total daily insulin, reducing user burden but limiting fine-tuned control. In contrast, ManualAID allows clinicians and families to adjust basal rates and correction factors directly. In highly skilled hands, this flexibility may be advantageous, particularly in paediatrics, where insulin needs shift rapidly with growth, hormones, and circadian variability. Yet, as seen in the authors’ socioeconomically deprived cohort, the need for manual upload and adjustment might prove disadvantageous.
CONCLUSION
What does this mean for clinical practice? A diabetes team confident in adjusting settings with patients able to engage regularly may achieve superior outcomes with ManualAID than automation alone, while less experienced users or those less resourced may fare worse. The power to adjust algorithms offers the potential for better control, but only if users have the required intellectual and digital capacity to upload and engage in systems. Looking ahead, the launch of TandemSource (Tandem Diabetes Care) offers automatic uploads for Control-IQ, addressing one major limitation. Whether this equalises outcomes, or whether algorithm update methods (automated by total daily dose versus manually tuned settings) remain a differentiator, will depend on skill, frequency of review, and the support structures surrounding families.







