INTRODUCTION
Incidences of both Type 1 diabetes mellitus (T1DM) and Type 2 diabetes mellitus (T2DM) are increasing among young people.1 The diabetes-associated excess risk of cardiovascular diseases is known to be higher in women than in men, mostly at peri and post-menopausal ages;2 however, the risk in a younger population still remains uncertain.3,4 To answer this question, we carried out a retrospective observational study over a 6-year follow-up period (1st January 2007–31st December 2012) in Tuscany, Italy, to compare by sex the effect of diabetes on the risk of first hospitalisations for atherosclerotic cardiovascular diseases (ASCVD).
METHODS
Baseline diabetes was identified by a regional diabetes dataset in 2006 and confirmed in the following years over the entire study period. Continuous insulin therapy from the onset was considered as a proxy for T1DM and all other treatments were considered proxies for T2DM. From the regional hospitalisation dataset, outcomes of interest were first hospitalisations for ASCVD, primary or secondary diagnosis of acute myocardial infarction (diagnosis code ICD-9-CM), ischaemic stroke, congestive heart failure, and lower extremity amputation. Patients with at least two prescriptions for angiotensin converting enzyme inhibitors or angiotensin receptor blockers, aspirin, or statins over the study period were traced for further information about primary or secondary prevention therapy. Analysis of proportional incident risk of first hospitalisations for ASCVD, after adjusting for age and comorbidities (Charlson Comorbidity Index), was carried out by the Cox regression analysis model.
RESULTS
The population without diabetes comprised 514,732 males and 515,799 females, and there were 2,052 males and 2,598 females with diabetes who had a mean age of 32±7 years (934 T1DM/1,664 T2DM among females and 1,256 T1DM/796 T2DM among males). Hospitalisation rates for ASCVD (per year per 100,000) were much higher in those with diabetes in both sexes (32 per year in people without diabetes versus 209 per year for T1DM and versus 510 per year in T2DM among males, and 14 per year versus 194 per year in T1DM and versus 48 per year for T2DM among females). In the T1DM group the hazard ratio of hospitalisations for ASCVD, adjusted for age and comorbidities, as compared with those without diabetes, was 6-times higher in women, although the ASCVD incidence rate in diabetic people was similar in both sexes. On the contrary, in T2DM patients the excess risk was 6-fold higher in men but not in women (Figure 1).
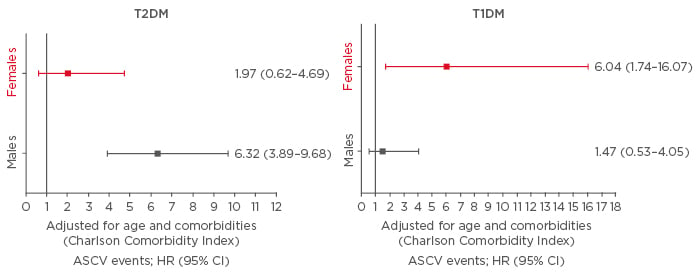
Figure 1: Risk of ASCVD events in subjects with T2DM or T1DM compared to those without diabetes, stratified by sex.
ASCVD: atherosclerotic cardiovascular diseases; CI: confidence interval; HR: hazard ratio; T1DM: Type 1 diabetes mellitus; T2DM: Type 2 diabetes mellitus.
Furthermore, within the diabetic populations, the risk of hospitalisation for ASCVD was higher in men with T2DM and similar between sexes in the T1DM group. ASCVD risk was higher in T1DM than in T2DM for males, while no significant difference between diabetes type was observed in females. Prescription of angiotensin converting enzyme inhibitors or angiotensin receptor blockers, aspirin, or statins was similar between sexes in T1DM patients and much greater among males with T2DM. No sex difference in all-cause mortality was observed, comparing people with or without diabetes.
CONCLUSION
In conclusion, whether these differences are due to a real sex-linked dimorphism, different characteristics of T1DM or T2DM in the youth, or a difference in the the presence of other modifiable ASCVD risk factors, as suggested by the sex inequality in drug prescription among people with T2DM, needs further investigation.








