INTRODUCTION AND AIMS
Traditionally, the lifetime risk of developing diverticulitis, the most common clinical complication in diverticular disease, is cited as 10–25%; this high rate of progression, however, has been contradicted by a recent colonoscopy-based retrospective study reporting that only approximately 4% of patients with diverticulosis develop acute diverticulitis.1 At present, a small number of studies, mainly retrospective, have evaluated the natural history of diverticulosis and diverticular disease.1-3
The aim of this study was to assess the incidence of new cases of symptomatic uncomplicated diverticular disease (SUDD) and diverticulitis, and recurrence of diverticulitis after 1-year of follow-up, in a cohort of patients with colonic diverticula.
METHODS
The Italian Study Group on Diverticular Disease (GRIMAD) scientific association promoted the creation of the Registry of Diverticular Disease (REMAD),4 an ongoing 5-year prospective, observational, multicentre, cohort study, involving 47 centres, both academic and non-academic. Each centre was required to recruit at least 20 consecutive patients over 2 months. A total of 1,255 consecutive patients with colonic diverticula were initially considered, but five centres recruited <20 patients, and, therefore, those centres and corresponding recruited patients were excluded from the study (n=38). The median rate of non-adherence of patients to the registry was 22% (range: 5.0–36.4%). Inclusion criteria were informed consent, age ≥18 years, and endoscopic or radiological-confirmed colonic diverticula. Outpatient visits or telephone appointments were scheduled every 6 months.
At entry, patients were categorised into three subgroups according to the following criteria:
- Diverticulosis: presence of colonic diverticula in the absence of abdominal symptoms.
- SUDD: recurrent abdominal symptoms as abdominal pain and/or changes in bowel habit, attributed to diverticula in the absence of overt inflammation.5-7
- Previous diverticulitis (PD): patients who have experienced at least one episode of acute diverticulitis in the past.
The number of new cases of SUDD, diverticulitis, and recurrence of diverticulitis after 1 year of follow-up was evaluated. Patients were allowed to continue their therapy, if any. Logistic regression (adjusted for age <60 years, sex, BMI ≥25 kg/m2, Charlson Comorbidity Index ≥3, gastrointestinal comorbidities, family history for diverticular disease, use of non-steroidal anti-inflammatory drugs, antiplatelet, anticoagulants, proton pumps inhibitors, and statins) was performed to identify patient features associated with new occurrence of SUDD and diverticulitis.
RESULTS
A total of 1,217 patients (556 [45.7%] female, mean age: 66.1±9.9 years, BMI: 26.1±3.9 kg/m2) with a baseline diagnosis of diverticulosis (57.9%), SUDD (24.7%), and PD (17.4%) were included in the study. At 12 months, 922 patients (53.1%, 29.8%, and 17.1% with diverticulosis, SUDD, and PD, respectively) were followed; 11.9% of patients were lost at follow-up and data of 15.5% were not up to date.
During follow-up, 33 (6.3%) baseline diverticulosis patients developed SUDD and 4 (0.7%) developed diverticulitis (1 perforation), 4 (1.6%) baseline SUDD patients developed diverticulitis (no complications), and 14 (9.4%) patients who entered with PD developed a recurrence of diverticulitis (including 3 patients with complications such as perforation, abscess, and stenosis). The median time from the first episode of diverticulitis to recurrence was 4.5 years (0.003–15.04); no patients required surgery. The main characteristics of patients who developed diverticulitis are reported in Table 1. Logistic regression showed that the female sex was associated with subjects who changed subgroup from diverticulosis to SUDD (odds ratio: 2.26; 95% confidence interval: 0.97-5.22; p=0.05, barely missed). No features associated with recurrence of diverticulitis could be identified.
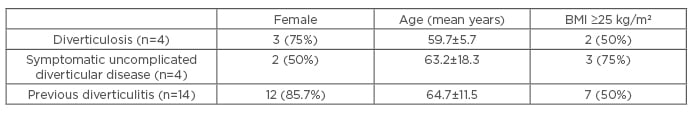
Table 1: Main characteristics of patients who developed diverticulitis.
CONCLUSION
These preliminary data show that, during an observation period of 1 year, progression from diverticulosis to SUDD occurred in <10% patients, and was associated with female sex. The overall incidence of diverticulitis was very low (2.3%), whereas recurrent diverticulitis was not uncommon. This observational study showed that, although the vast majority of patients did not show progression of disease, diverticulitis recurrence represents an important clinical challenge.








