BACKGROUND AND AIMS
Europe’s Beating Cancer Plan calls for the development of a gastric cancer screening strategy in Europe. The TOwards GAstric cancer Screening (TOGAS) consortium was established to explore the feasibility of gastric cancer screening approaches within Europe. One key method involves the detection and eradication of Helicobacter pylori, the leading causative agent of gastric cancer. However, not all regions are affected in the same way.1 In Western Europe, infection and cancer rates are higher among males, smokers, and individuals of lower socioeconomic status, which are groups that tend to engage less with preventive health services.2,3
This pilot study aimed to determine whether targeted screening in high-risk occupational settings improves participation and outcomes compared to population-based screening via general practice invitations. Key outcome measures included response rate, prevalence of the infection, and treatment effectiveness.4
MATERIALS AND METHODS
This prospective pilot study recruited individuals aged 30–34 years from January 2024–March 2025. Participants were invited either through general practices (general population group [GPG]) or through two occupational screening programmes (targeted group [TG]) representing higher-risk, male-dominated workforces: the Irish Defence Forces and the Construction Workers Health Trust, Dublin, Ireland. Exclusion criteria included prior H. pylori treatment or gastrectomy. All participants underwent serologic screening (H. pylori IgG antibody). The TG was offered initial on-site screening at their workplace, while the GPG attended a local hospital. All seropositive individuals were offered confirmatory 13-C urea breath testing (UBT) in a local hospital. Confirmed cases were offered a 10-day regimen of bismuth subcitrate/metronidazole/tetracycline with esomeprazole 40 mg twice a day. Eradication was assessed ≥6 weeks post-treatment. Response rates, demographics, infection prevalence, and treatment outcomes were analysed using Mann–Whitney U and Chi-squared tests (significance: p<0.05).
RESULTS
A total of 3,030 individuals were invited for screening: 2,824 in the GPG, and 206 in the TG. Key demographics and risk factors of each group are shown in Table 1. The invitation response and participation rates were significantly higher in the TG versus the GPG (invitation response: 31% versus 14%; p<0.001; participation rate: 30% versus 14%; p <0.00). H. pylori seroprevalence rates were similar between groups: 18% (11/60) in the TG and 19% (64/333) in the GPG (p<0.70). Confirmatory 13-C UBT was completed in 91% (10/11) of those who tested positive in the TG and 98% (63/64) of those who tested positive in the GPG. Overall, ‘true’ prevalence rates based on serology and confirmatory 13-C UBT results were 10% (6/59) in the TG versus 14% (44/325) in the GPG (p=0.47). Treatment adherence exceeded 90% in both groups, with 100% adherence in the TG and 90% in the GPG. Among those who completed post-treatment testing (n=37), eradication was achieved in 100% of the TG (2/2) and 89% of the GPG (31/35).
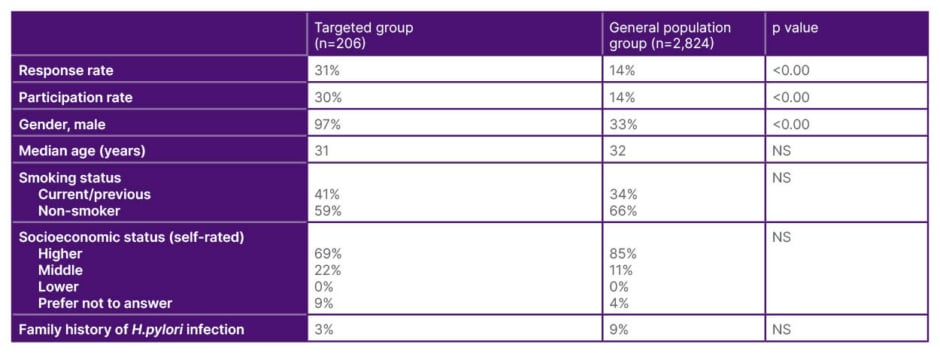
Table 1: Demographics, risk factors, and participation rate broken down by group.
H.pylori: Helicobacter pylori; NS: non-significant.
CONCLUSION
Targeted occupational screening in high-risk populations demonstrated superior response and engagement rates compared to general practice-based screening. These early results suggest that this approach may be a more effective and resource-conscious strategy in low-to-intermediate risk countries, and merit further evaluation in broader implementation efforts.