Abstract
Aim: To compare the effectiveness of three different anchoring methods for percutaneous drainage catheter (PDC) in preventing accidental dislodgement, occurrence of medical adhesive-related skin injury (MARSI), ease of application, and additional anchorage changes.
Methodology: Patients undergoing PDC were randomly allocated into intervention groups: medical silk tape (DP), micropore tape (MP), or securement dressing (GL). The anchoring dressing was changed once a week or when it was soiled. Weekly follow-up via a phone call was conducted for 4 weeks.
Results: Fifty-four participants were recruited. There was a significant difference in MARSI for DP compared to MP (z: -2.45, p=0.014) and GL (Z-score [z]: -2.51, p=0.012). DP (median: 1) was significantly easier to apply when compared to MP (median: 3, H-score [H]: 13.30, p=0.015). There was a significant difference in additional changes required for MP (n=5, z: -2.44, p=0.015) and DP (n=4, z: -2.21, p=0.027) as compared to GL. There were no PDC dislodgements.
Conclusion: This pilot study suggests that securement dressing has the lowest association with MARSI and does not require frequent changes. However, further research with a larger patient population is necessary to validate these findings, as definitive conclusions cannot be drawn from a small sample size.
Key Points
1. There are no gold standards on percutaneous drainage catheter anchorage methods despite seemingly high rates of dislodgement.2. A quasi-experimental study was conducted to compare the effectiveness of three different line anchoring methods in preventing accidental dislodgement, occurrence of medical adhesive-related skin injury, ease of application, and additional anchorage changes.
3. Using a securement dressing may be an ideal method for percutaneous catheter anchorage while maintaining skin integrity with good yet comfortable adhesion.
INTRODUCTION
Percutaneous drainage catheter (PDC) insertion is an effective, safe, and well-tolerated method of relieving obstructions and drainage, especially in the renal or biliary system. It plays a significant role especially when biliary and renal systems are not inaccessible due to obstructions.1 PDC insertion is a minimally invasive procedure requiring radiology imaging guidance during the insertion of the catheter through the skin to drain the infected fluid or relieve it.2,3 While PDC is effective for up to 6–12 months, some patients may require long-term placement.4
One of the most common complications related to PDC is accidental dislodgement.5-8 Dislodgement can be defined as the displacement of the PDC followed by possible leakage, insufficient drainage, or protruding catheter.1 An unpublished retrospective data review conducted among patients with PDC reported an average of two to three accidental dislodgements per month within the authors’ institution. Each re-insertion procedure alone can cost from 900 to 3,200 SGD. With dislodgment, the patient can wait at least 3–5 days for a reinsertion appointment, leading to frequent readmissions, longer hospitalisation stays, complications from reinsertion, increased use of resources, significant delay in treatment, and hospitalisation cost.5,9 This compromises patient satisfaction and quality of care.10 A rapid improvement project was carried out to investigate the root cause of the dislodgment. The tubing anchoring method and dressing material used were identified as the root causes of accidental dislodgement.
The standard of care for external catheter anchorage is to suture the catheter to the skin at the insertion site.11 Within our institution, external catheter anchorage is usually accomplished in two steps: to suture the catheter to the skin at the insertion site and to use an adhesive medical tape in a crisscross technique to anchor the tubing onto the patient’s skin. Common reasons for accidental dislodgement apart from suture techniques are patient movement on the bed, accidental line tugging, bed transfers, skin integrity, patient ambulation, catching onto things in their environment, and loosening of tapes.12
Peripherally inserted catheters, which include short peripheral intravenous catheters, peripherally inserted central catheters, and central venous catheters, are the most inserted catheters worldwide.13 As such, the anchoring of these catheters has been extensively studied.4,7,8,13 The gold standard of anchoring the central venous catheters is the usage of transparent occlusive dressing, preferably impregnated with chlorhexidine gluconate, to firstly lower catheter failure and lower central line-associated bloodstream infection.13 In short, intravenous catheters and peripherally inserted central catheters; however, there is no established gold standard for anchoring.14 Literature strongly recommends using two options concurrently: a transparent dressing and securing the catheter to provide anchorage, as the usage of an additional form of securement was found to keep the catheter in place and reduce potential complications.14
In comparison, however, there is limited data on anchoring methods pertaining specifically to PDC, although high rates of dislodgment are also reported in the literature.
A review of the clinical evidence and guidelines on PDC care showed a variety of dressing methods.2 It involved multiple tube fixation devices to anchor the catheter with different dressing methods. As PDC can remain on patients from a few days to months, applying multiple dressings can be challenging for both the patients and caregivers. PDC is often longer in length as compared to many other catheters. This, in addition to the forces encountered on a day-to-day basis over an extended duration, can render current anchorage guidelines as inadequate.11
For a potentially long-term PDC that is at a fixed position, there is a need for repeated removal and application of the anchoring dressing. Such repeated action compromises the skin barrier function and can lead to skin injury, also known as medical adhesive-related skin injury (MARSI). MARSI is commonly associated with drainage catheters.15 It is a preventable skin injury; it is defined as an occurrence of erythema, vesicle, erosion, or tears persisting for more than 30 minutes after adhesive removal.16 Even when there is no visible trauma, the adhesive can lead to detachment of superficial epidermal cell layers. MARSI can be classified into skin tears, skin stripping, tension injury or blister, maceration, folliculitis, allergic contact dermatitis, and irritant contact dermatitis.16,17 MARSI are painful and can cause deep tissue injuries that can take more than 6 weeks to re-epithelialise.18
The ideal PDC line anchoring method should provide excellent anchorage to prevent accidental dislodgment and be comfortable, non-irritating, cost-effective, and easy to use. Decreasing PDC dislodgment can significantly impact patient morbidity and treatment costs. To date, however, there is no consensus on the optimal anchoring method for PDC. There is now a large variety of securement methods available specifically designed to anchor catheter tubing. While it has been extensively studied on central venous catheters to show an overall reduction in complications, there is minimal data on its use on PDC.19,20
A stabilisation and securement dressing for medical lines, catheters, and tubings recently became available at the authors’ institution. It offers a secure attachment without sutures and hypoallergenic adhesives.21 The meta-analysis by Xu et al.22 suggested that there is low evidence for the usage of sutureless securement devices in minimising movement and improving anchorage when compared to other dressings.22 There is currently limited research comparing securement dressings with established medical tapes often used for anchorage. Hence, it was of interest to not only evaluate the securement dressing, but also to compare the medical tapes against the securement dressing regarding important patient outcomes.
METHODS
Study Design
A quasi-experimental study was conducted in Singapore General Hospital, an acute tertiary hospital in Singapore, and National Cancer Centre, Singapore, a tertiary specialist cancer centre.
Study Aims
This study aimed to compare the effectiveness of three different line anchoring methods for PDCs in:
- preventing accidental dislodgement;
- occurrence of MARSI;
- ease of application; and
- additional anchorage changes and applications, if any.
Participants
Patients were recruited according to the following criteria from February 2019 – July 2021:
Inclusion criteria
- All patients with scheduled PDCs to be inserted.
- At least 21 years old for consent purposes.
Exclusion criteria
- Critically ill patients.
- Patients with complication(s) such as post-insertion bleeding, sepsis, and injury to an adjacent organ.
Ethical Consideration
This study conformed to the ethical guidelines of the Declaration of Helsinki. This study was approved by the SingHealth Institutional Review Board (CIRB reference number: CIRB 2018/2912), where informed consent with a witness was obtained from the participants. REDCap, a Singhealth secure web application complying with CIRB data security requirements for managing databases, was used to enter and store the collected data.
Study Procedure
Patients were recruited from four inpatient surgical units and outpatient clinics. Potential participants were identified from the listing provided by the Interventional Radiology department or by speciality nurses. Potential participants were then approached for recruitment. Post PDC creation, IV advance dressing was applied at the PDC exit site for all participants, which is the standard dressing applied for all PDC exit sites. Recruited participants were allocated using computer–generated randomisation to one of the three intervention groups with different anchoring methods: (1) IV advance with medical silk tape (DP) (n=17), (2) IV advance with micropore tape (MP) (n=18), or (3) IV advance with securement dressing (GL) (n=21). DP and MP were applied in a crisscross technique to anchor the tubing onto the patient’s skin. Patient education on the anchoring method was done prior to discharge. The anchoring dressing was changed by the patient or caregiver once a week, or when it was soiled. Weekly follow-up via a phone call was conducted for 4 weeks to check on any accidental dislodgement, ease of application of anchoring method, and presence of MARSI (dichotomous questions with a yes or no option). Ease of application was assessed on a Likert scale rating, ranging from 1 (easy) to 5 (challenging).
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (IBM, Version 26). Descriptive statistics were applied to analyse the frequency of MARSI, ease of change, and number of additional changes and applications. Nonparametric tests were used given the sample size and categorical data that was collected. The Mann-Whitney U test was conducted to analyse pairwise differences for ease of application and presence of MARSI. The Kruskal-Wallis test was conducted to analyse pairwise differences between ease of application.
RESULTS
A total of 60 patients were recruited (Figure 1). Six patients were lost to follow-up and were excluded. A total of 54 patients completed the study.
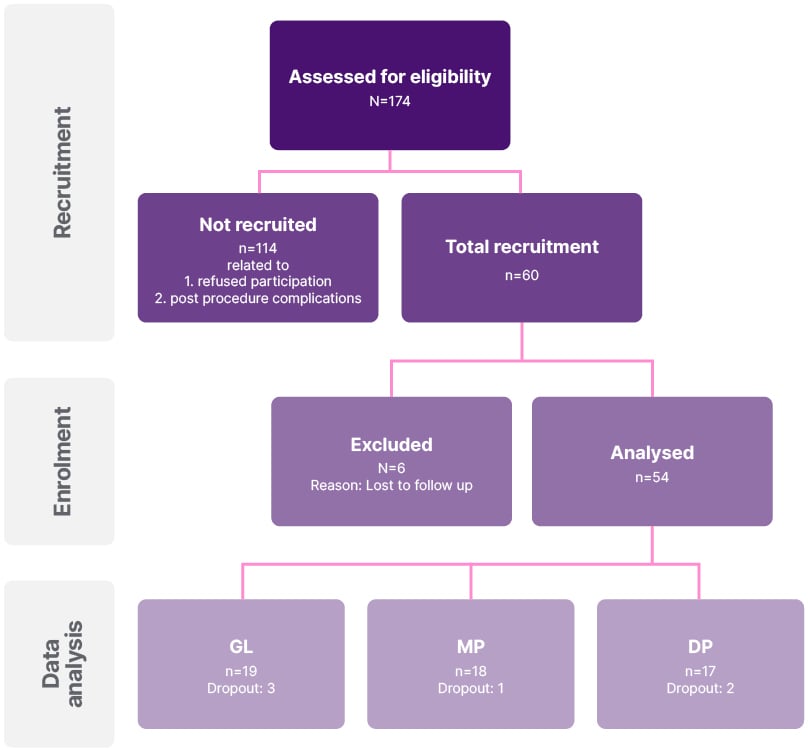
Figure 1: Study Algorithm.
DP: silk tape; GL: Grip-Lok; MP: micropore.
Most patients were between 61–80 years of age (Table 1). The most common site for PDC insertion was the biliary system (n=22, 40.7%), and the abdomen or peritoneum (n=20, 37.0%). Caregivers were available for 52 patients (96.3%). Up to 44 patients (81.5%) had their first PDC insertion in this study. There were no PDC dislodgments seen during this study.
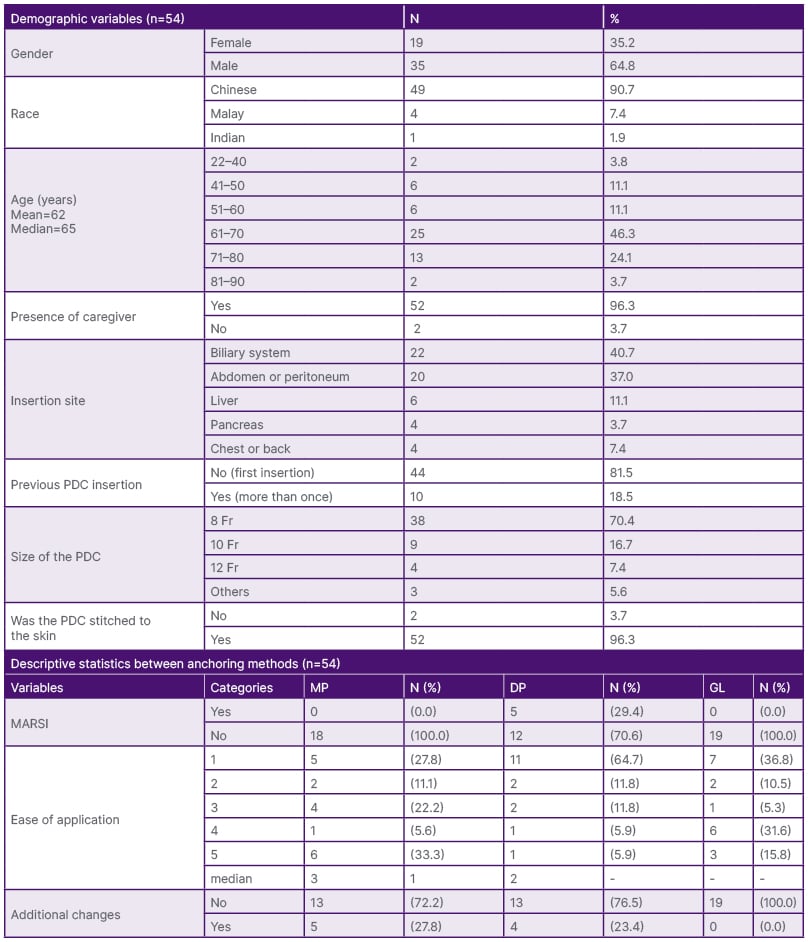
Table 1: Descriptive statistics.
DP: silk tape; GL: Grip-Lok; MP: micropore.
DP was the only anchoring method involved in MARSI in 5 patients (Tables 1 and 2). As such, there was a significant difference in MARSI occurrence for DP as compared to MP (Z-score [z]: -2.45, p=0.014) and GL (z: -2.51, p=0.012). DP (median=1) was significantly easier to apply when compared to MP (median: 3, H-score [H]: 13.30, p=0.015) (Tables 1 and 2). MP was reported to be not sticking well (n=5) and requiring multiple strips for adherence (n=2) (Tables 1 and 2). GL was associated with no additional changes as compared to DP and MP. As such, there was a significant difference in additional changes required for MP (n=5, z: -2.44, p=0.015) and DP (n=4, z: -2.21, p=0.027) as compared to GL.
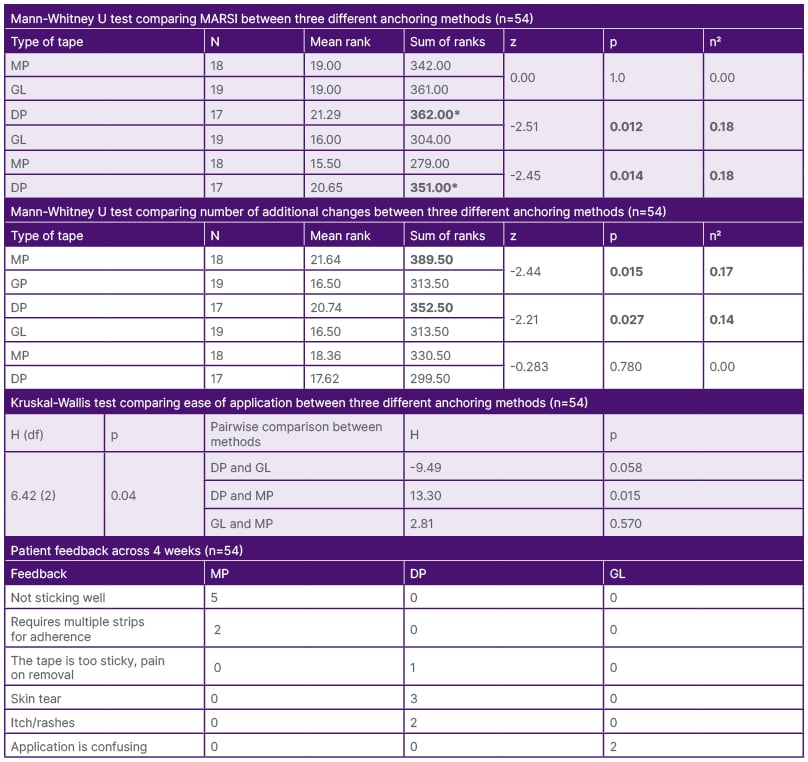
Table 2: Comparison and patient feedback on the anchoring techniques on medical adhesive-related skin injury, additional changes and ease of application (n=54).
DP: silk tape; GL: Grip-Lok; MARSI: medical adhesive-related skin injury; MP: micropore.
*Significant when p<0.05 n2 ≥0.14: large effect where outcome was affected by the anchorage method (Cohen 199223).
DISCUSSION
Accidental dislodgement of PDC is crucial to prevent delayed treatment, complications from reinsertion, increased morbidity, and treatment costs. While there are expert and literature recommendations to secure catheters for anchorage,14 studies often use different primary dressings with different securement methods.12,22,24 Given that transparent occlusive dressing is the recommended dressing for catheters,14 this study evaluated the effectiveness of three different line anchoring methods in preventing PDC dislodgement.
There was no accidental dislodgement seen across the three different anchoring dressings during the study period. Given the institution’s retrospective data and literature,14 accidental dislodgments were expected when only tape was used for anchorage. Given that both tapes were changed more frequently as compared to DP, it is plausible that the frequent changes ensured anchorage and prevented dislodgement.
Apart from DP, neither MP nor GL was significantly associated with MARSI. Five patients experienced DP-associated MARSI, ranging from itch and skin rashes to skin tears. Silk tape, an acrylate adhesive tape with woven polyester backing, has been previously reported to possibly cause greater skin trauma as compared to silicone tape.25 The skin is the body’s natural defence system against pathogens from the external environment.26 Patients with impaired skin integrity are subjected to more pain and discomfort,27 and are at greater risk of localised and systemic infections.16 Impaired skin integrity also creates a burden of sickness, including anxiety, depression, reduced quality of life, and impaired social well-being of both patients and carers.28 While MARSI can appear to be a minor injury, it is a specific and challenging wound, especially when there are skin tears involved.29 PDC can remain on patients for long periods, requiring repeated application and removal of anchoring dressing. As such, skin integrity related to the effects of anchoring dressing is an important outcome that must be considered.14 In addition, patients can experience PDC-related complications such as pain, infection, and leakage.5 It is crucial that the anchoring dressing does not contribute to or aggravate such possible developments.
DP was the only dressing associated with MARSI, despite being the easiest to apply. MP was reported as being the least easy anchoring method, which can be related to the tape not sticking well, requiring multiple strips. Two of the participants had reported GL application to be confusing. This can be attributed to its four-step application. Despite that, there were no additional changes required with GL, suggesting that the patient or caregiver was able to apply it correctly. The frequency of change may not be the most frequently assessed outcome in similar studies.24 As frequency of change reflects durability and thus contributes to potential displacement or dislodgment, it was one of the primary outcomes of this study. GL was the only method requiring no additional changes as well. With the duration of PDC ranging from days to months, caregivers and patients can be expected to care for the PDC for a longer time frame. Patients and caregivers may need to make lifestyle modifications when living with a catheter,30 and the need for frequent changing of anchoring dressing can have a negative impact on their daily lifestyle.31
LIMITATIONS
One limitation of this study is the use of convenient sampling, which may not have the same methodological rigour when evaluating the effectiveness of an intervention.32 There is the risk of sample selection bias as only selected units were included for data collection, outlying patients were not included.33 As this was a pilot study, the target sample size for each group was set at 30 participants.34 Given that the patient numbers in both inpatients and outpatients were affected due to the pandemic, the target sample size could not be met within the study timeline. The ease of application was based on a Likert scale rating and it is not a validated tool. While there are validated tools such as the USE Questionnaire,35,36 certain questions may not be applicable to dressing application or pertaining to patients’ or caregivers’ perspectives, and thus were not utilised for this study.
IMPLICATION FOR PRACTICE
The nursing quality team conducted a further evaluation and decided to implement the securement device as an improvement to the inpatient work process. Instead of medical tapes, the use of the securement device for anchorage has been expanded for all catheters and drains, where appropriate. The securement device has currently been made available within all inpatient wards.
FUTURE RESEARCH
While this pilot study did show a significant difference between the three different anchoring methods, further high-quality evidence is required, especially since there was no incidence of slippage among the study participants. Hence, evaluation of the securement device is necessary, especially for inpatients, through follow-up care from both the caregivers and patients for continuous improvement. As PDC can remain for extended periods, a more rigorous efficacy trial over a longer follow-up period, including cost-effectiveness analyses and time spent on anchorage dressing by nurses or caregivers should be considered.
CONCLUSION
This study compared three anchoring methods specifically with regards to PDC. There was no dislodgement seen across the three different anchoring methods. Although DP may be the easiest dressing to apply, it was the only dressing associated with MARSI. MP was associated with additional changes and applications. There were no additional changes or MARSI with GL. While there are four steps for GL application, only two patients had reported difficult application. As such, GL might be an ideal dressing for PDC anchorage while maintaining skin integrity with good yet comfortable adhesion.
AVAILABILITY OF DATA AND MATERIALS
Due to ethical concerns, study data cannot be made openly available. Data may be made available upon request from the corresponding author.







