BACKGROUND AND AIMS
Strongyloides stercoralis is an intestinal parasitic nematode with a 2–7% prevalence in the USA. Immunosuppression can predispose to disseminated infection, concurrent bacterial sepsis, and significant morbidity and mortality. The authors sought to review positive Strongyloides serology (PSS) results across three academic medical centers.1,2
METHODS
Electronic medical records of patients with PSS were reviewed between 2012–2023. Extracted data included demographics, country of origin, travel history, testing indication, clinical presentation, treatment regimen, and duration (Table 1). Patients were classified into chronic infection (PSS without additional clinical manifestations), hyperinfection syndrome (cutaneous, gastrointestinal tract, or lung involvement), and disseminated infection (evidence of involvement of distant sites beyond hyperinfection, such as the brain, liver, kidneys, or bloodstream).
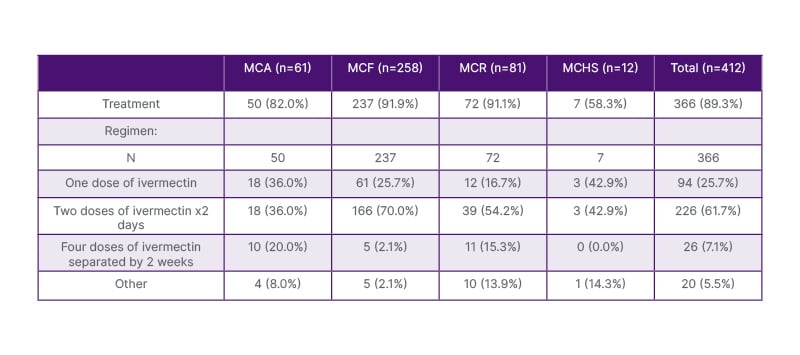
Table 1: Treatment regimens received.
MCA: Mayo Clinic Arizona; MCF: Mayo Clinic Florida; MCHS: Mayo Clinic Health System; MCR: Mayo Clinic Rochester.
RESULTS
Overall PSS rate across the three sites was 5.5%. A total of 412 patients with PSS were identified, with a mean age of 56.7 years (SD±14.2), of whom 272 (66%) were male. The primary indication for testing was transplant evaluation in 230 (56%), eosinophilia workup in 84 (20%), suspicion of active infection in 74 (18%), travel history in 27 (7%), and pre-immunosuppression screening in 27 (7%). Four hundred and one (97.3%) were categorized as chronic infection, 10 (2%) as hyperinfection, and one (0.2%) as disseminated infection. Treatment was administered to 366 (89.3%) patients: 226 (61.7%) received two doses of ivermectin on consecutive days, 94 (25.7%) received a single dose, 26 (7.1%) received two doses repeated 2 weeks later, and 20 (5.5%) received alternative regimens. The patient with disseminated infection received 2 weeks of ivermectin followed by monthly dosing.
CONCLUSION
The majority of patients with PSS were asymptomatic, and treatment regimens were not uniform. Screening should be considered for patients currently receiving or initiating long-term immunosuppression that can potentiate Strongyloides dissemination. Developing a targeted testing algorithm based on epidemiologic factors, clinical suspicion, laboratory parameters, and the nature of immunosuppression can help identify at-risk patients who can receive pre-emptive therapy if infected.3,4