BACKGROUND AND AIMS
The University of Illinois Hospital and Health Sciences Center (UIH), Chicago, USA, multidisciplinary telemedicine clinic provides HIV care to justice-involved individuals in the Illinois Department of Corrections (IDOC).1 Post-release HIV care remains challenging, with virologic suppression (VS) dropping from 73% at release to 49.7% at reincarceration into IDOC, based on previous data.2 To improve continuity of care, wrap-around services were expanded from follow-up care at UIH to medical insurance assistance, case management, employment/housing support, and statewide follow-up care.3
MATERIALS AND METHODS
This Institutional Review Board (IRB)-approved, retrospective cohort study occurred from January 1, 2021–August 31, 2024 and analyzed demographic, clinical, and social determinants of health in people with HIV aged 18 years or older, who were in custody in IDOC, released, and reincarcerated during the study period. The primary outcome was a change in the number of patients with complete VS at the time of release as compared to reincarceration in those who were virologically suppressed at release.4 Secondary outcomes included change in immunologic function and identification of factors influencing loss of VS upon reincarceration.
RESULTS
Of 393 patients released during the study period, 95 were reincarcerated, 82 were included, and 75 had VS at the time of release. Of the 75 who achieved VS at release, 62 maintained VS (Group 1) at reincarceration, while 13 experienced loss of VS (Group 2; p=0.0001). Median cluster of differentiation (CD)4 count of those who met inclusion criteria declined significantly from release to reincarceration (p=0.0032), but the change in CD4% was not significant (p=0.0973; Table 1).
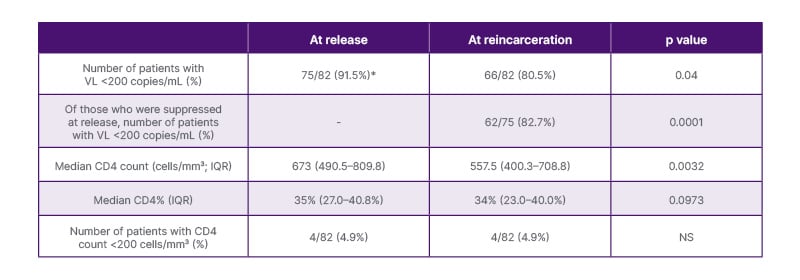
Table 1: Viral Load, CD4 count, and CD4% data at release and upon reincarceration.
*Patients who were not suppressed at release: four patients were released before the lab results could be updated, two patients preferred no pharmacotherapy, and one patient was not started on medication because the team decided it would be more effective to initiate treatment after release to ensure better follow-up and continuity of care.
CD: cluster of differentiation; IQR: interquartile range; NS: not significant; VL: viral load.
No difference was found between Group 1 and 2 in scheduling a statewide follow-up visit (p=0.0813), following up at UIH clinic at least once (p=1.00), or having AIDS Drug Assistance Program (ADAP) coverage (p=0.7552). Loss of VS was significantly associated with patient-reported housing instability (p=0.0046), lack of access to care (p=0.0056), living outside of Chicago (p=0.0318), and transferring from a jail in a rural setting (p=0.0054).
CONCLUSION
As the role of the IDOC telemedicine team expanded, the proportion of individuals who maintained VS upon reincarceration increased from 49.7% in 2014 to 82.7% in 2024. While interventions show progress, more targeted efforts are needed to address housing, care access, and non-Chicago residency.







