BACKGROUND AND AIMS
Personalised care in conservative kidney management (CKM) provides person-centred care for patients who have opted for non-dialytic therapy. However, the illness trajectory of patients with chronic kidney disease (CKD) G5 on CKM can be unpredictable. A previous study suggested a sharp increase in symptom distress and health-related concerns in the 2 months before death.1 The aims of this study were to identify clinical tools associated with mortality in patients on CKM, and to evaluate the concordance between preferred and actual place of death.2
METHOD
This was a single-centre cohort study including 109 patients with CKD G5 who opted for CKM from April 2021–September 2024. Baseline demographic, clinical data, laboratory data, Clinical Frailty Score (CFS), Edmonton Symptom Assessment System Revised: Renal (ESAS-r: Renal) score,3 Resources Utilisation Group-Activities of Daily Living (RUG-ADL) score,4 Palliative Performance Score (PPS),5 and Karnofsky Performance Score (KPS) were collected. Logistic regression and survival analysis were performed.
RESULTS
The mean±SD age of the patients was 79.8±7.3 years, 64.2% were female, and 82.6% were Chinese. The primary cause of CKD G5 was diabetes (69.7%). Baseline mean estimated glomerular filtration rate CKD-epidemiology collaboration (eGFRCKD-EPI) was 10.3 mL/min, with a Charlson comorbidity index of 8.5, a CFS of 4.6, and a KPS of 67.3. The median total ESASr-Renal score was 1, the RUG-ADL score was 4, PPS was 60, serum albumin was 38 g/L, and haemoglobin was 9.6 g/dL. Sixty-two patients (56.9%) became deceased during follow-up, with a median survival of 11.9 months. After adjusting for variables, baseline eGFRCKD-EPI remained the only significant predictor of mortality (Figure 1A). Patients with eGFRCKD-EPI ≤5 mL/min had a median survival of 4 months. A PPS of <50 showed a clear correlation with poorer survival estimates (Figure 1B). The advance care planning completion rate in this cohort was 60.5%. There was a moderate concordance between preferred and actual place of death, with 35.5% of the deceased patients passing away at home.
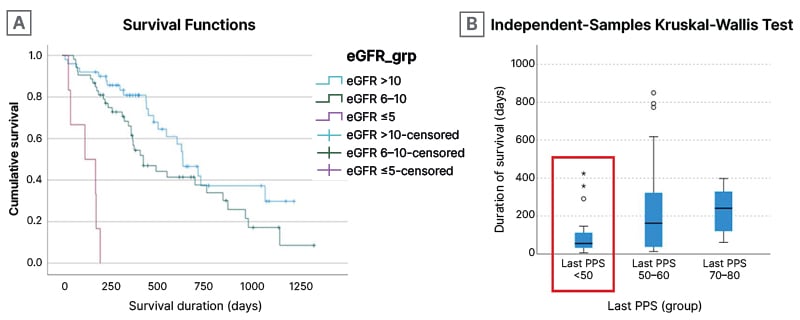
Figure 1: Duration of survival for patients who opted for conservative kidney management.
A) Duration of survival for patients on CKM of varying eGFR. B) Duration of survival based on PPS.
CKM: conservative kidney management; eGFR: estimated glomerular filtration rate; grp: group;
PPS: Palliative Performance Score.
CONCLUSION
Baseline eGFRCKD-EPI is a significant predictor of mortality in patients on CKM. PPS demonstrated utility in estimating survival and may aid in timely transitions to hospice care. While ‘home’ remains the preferred place for end-of-life care for most, fulfilling this preference remains challenging. This study highlighted the importance of early identification of patients at-risk, as well as the need for personalised care plans in CKM. Recognition of these poor prognostic values may facilitate timely referrals to hospice service.






