BACKGROUND
Hypertensive disorders of pregnancy (HDP) are associated with an increased postpartum risk of cardiovascular disease or kidney failure. In recent years, the profile of pregnant women has changed. Factors such as older age at pregnancy, obesity, diabetes, chronic hypertension, and chronic kidney disease, and the use of assisted reproductive technologies, have become more common. These changes have contributed to a rise in HDP cases, with the WHO estimating an incidence of 2–10% globally.1-8
However, there is scarce information on current practice regarding follow-up of HDP in diverse healthcare systems, especially in an evolving demographic environment. Spain is one of the Western European countries that does not yet have a national HDP registry.
Recognising this gap, a multidisciplinary group of Spanish healthcare professionals, including nephrologists, primary care physicians, and obstetricians, has proposed a national postpartum care plan. This plan will focus on vascular and kidney health, aiming to improve prevention, health promotion, and long-term monitoring for affected women.
This study9 aimed to analyse, for the first time, the incidence and trends of HDP in Spain between 2016–2022. It also sought to identify regional differences in HDP rates across the country.
METHODS
Researchers used data from the Spanish Ministry of Health’s Registry of Specialized Care Activity (RAE-CMBD). HDP cases were identified using international statistical classification of disease (ICD) codes (ICD-9 and ICD-10): pre-existing hypertension complicating pregnancy, childbirth, and the puerperium (010); chronic hypertension with superimposed preeclampsia (O11); gestational (pregnancy-induced) oedema and proteinuria without hypertension (012); and gestational hypertension (O13).
Incidence was calculated by dividing the number of HDP cases by the total number of births and multiplying by 100. To assess trends over time, the incidence in each year was compared to that in 2016. Relative risk (RR) and 95% CIs were used to determine statistical significance. Regional differences were analysed using Poisson regression models, and adjustments were made for multiple comparisons using the Benjamini-Hochberg method. If the p value for the interaction was <0.05, the temporal evolution differed between the two regions being compared.
RESULTS
The study found a significant increase in HDP incidence in Spain in 2021 (1.80 versus 1.84; RR: 1.055; 95% CI: 1.033–1.076) and 2022 (1.80 versus 1.90; RR: 1.063; 95% CI: 1.041–1.084), compared to 2016 (Table 1). The regions with the highest rates between 2016–2022 included the Balearic Islands, Canary Islands, Melilla, Aragón, Catalonia, and Ceuta (Figure 1).
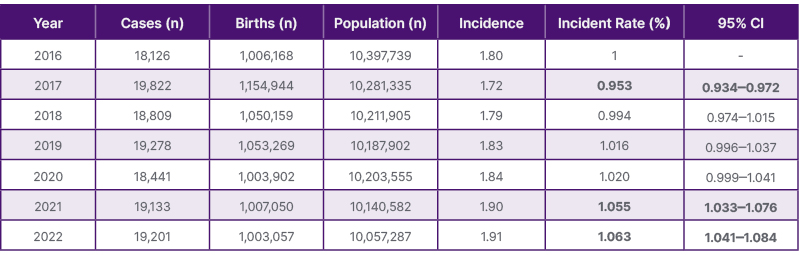
Table 1: Incidence of hypertensive disorders of pregnancy according to between 2016–2022.
Bold font means the comparison is significant, where 0.953 is a significantly lower incidence, and both 1.055 and 1.063 are significantly higher incidences.
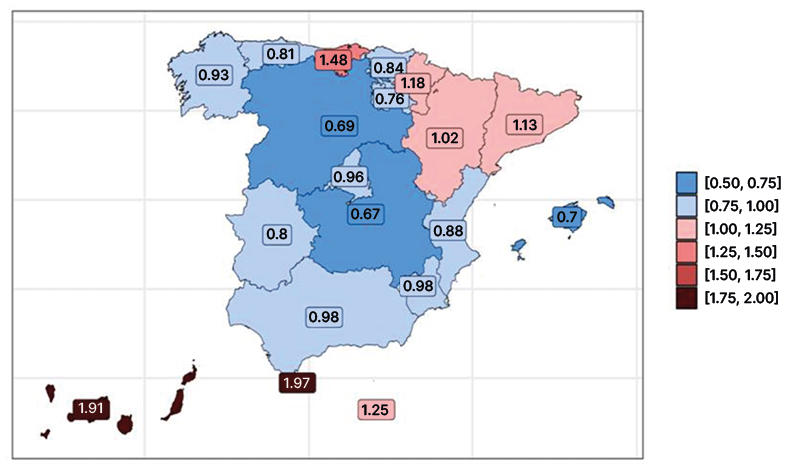
Figure 1: Incidence rate of hypertensive disorders of pregnancy during 2016–2022 in the different regions of Spain.
Color-coded map illustrating incidence rates, with blue representing regions of lower incidence and red indicating areas of higher incidence. The gradient reflects the range of incidence values observed across the dataset.
Importantly, there were significant differences in HDP incidence across Spain’s regions, suggesting inconsistencies in diagnosis or reporting practices (Table 2). While Spain’s overall HDP incidence (1.8%) is lower than that of other European countries like France (2.3%), Greece (2.2%), and Norway (4.0%), this may reflect underdiagnosis or gaps in follow-up care.10,11
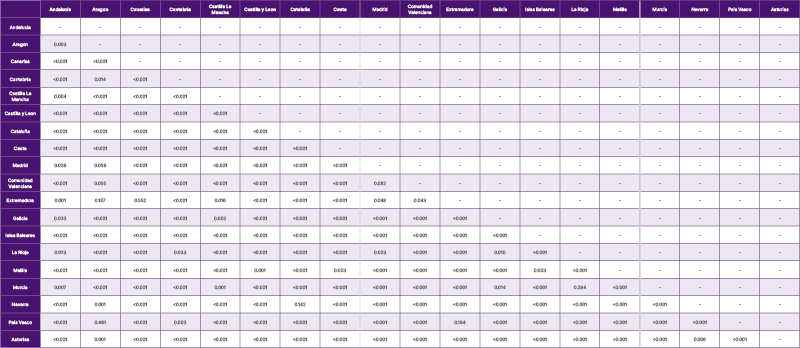
Table 2: Comparison of temporal trends across Spanish regions.*
Poisson regression models applied to analyse the temporal evolution in different regions. The models include an interaction term between time and Spanish region, allowing for the assessment of differences in temporal trends across regions.
*Please note, data for this table are not fully visible, please download the PDF to view the full data set.
CONCLUSION
This is the first nationwide study to examine HDP incidence in Spain and its regional variations. A significant increase in incidence was observed over time in Spain from 2016–2022. Most regions in Spain reported an incidence below 1. The relatively low incidence suggests that many cases may go undiagnosed, potentially putting women at risk for future cardiovascular complications. The significant difference in incidence variability between the different regions in Spain points out the need for a homogeneous discharge and hospitalisation follow-up protocol for primary care. A national registry and coordinated follow-up system could help ensure better outcomes for mothers and their children.






