BACKGROUND
Healthy sleep habits are highly recommended for individuals with chronic kidney disease (CKD)1 to improve their quality of life and reduce the decline in kidney function.2 However, there is limited research on the sleep habits of individuals with CKD and how these impact sleep quality and fatigue. This study3 aims to describe sleep habits in the CKD population and identify their correlation with sleep quality and fatigue.
METHODS
A cross-sectional survey was conducted in four nephrology units across three Australian states between 1st August 2024–31st December 2024. Data were collected anonymously from adults with CKD using both paper-based questionnaires and online surveys. Validated instruments, including the Sleep Hygiene Index (SHI), Pittsburgh Sleep Quality Index (PSQI), and Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), were used to assess self-reported sleep habits, sleep quality, and fatigue, respectively. Spearman’s rank correlation was used to assess the relationship between sleep habits, sleep quality, and fatigue.
RESULTS
A total of 173 surveys were returned. Mean age was 64 years, 70% were male, and participants were predominantly receiving haemodialysis (78%). Overall, sleep hygiene engagement was good (mean SHI: 13.6; SD: 7.9; maximum obtainable: 52, with higher scores indicating poorer sleep hygiene). However, sleep quality was poor across all participants (median PSQI: 8; interquartile range: 5–12; maximum obtainable: 21, with a score of 5 or greater indicating ‘poor’ sleep). Moderate fatigue was identified (mean FACIT-F: 29.9; SD: 12.8; maximum obtainable: 52, with higher scores indicating a lower level of fatigue). There were a small number of responses from patients receiving conservative management (n=3), those with CKD not requiring kidney replacement therapy (n=7), and post-kidney transplant (n=6); therefore, these cohorts are not included in the subgroup comparisons. Sleep hygiene engagement and sleep quality were similar between patients receiving haemodialysis and peritoneal dialysis. FACIT-F scores showed that patients receiving haemodialysis reported a higher level of fatigue compared to those on peritoneal dialysis. Of all sleep hygiene behaviours, four were most commonly reported: 1) having daytime naps; 2) different bedtime from day-to-day; 3) different wake time from day-to-day; and 4) thinking, planning, or worrying while in bed. Over 50% of participants reported these behaviours as occurring sometimes, frequently, or always (Figure 1). Correlation analysis revealed a weak but statistically significant relationship between sleep habits and sleep quality (r=0.36; p<0.001) and fatigue (r= –0.31; p<0.001).
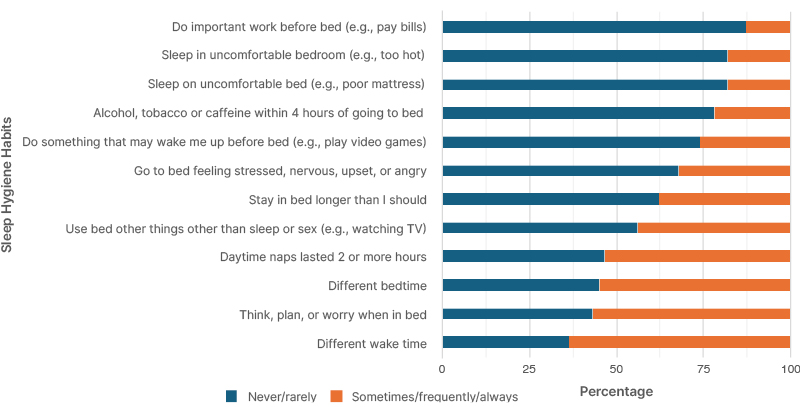
Figure 1: Self-reported sleep hygiene in people with chronic kidney disease.
CONCLUSION
This study highlights that overall sleep hygiene practices are good among individuals with CKD. Although correlations between sleep habits, sleep quality, and fatigue were weak, they were statistically significant, indicating these relationships are unlikely to be random. These findings suggest that healthy sleep habits are correlated to both fatigue and sleep. The four most commonly reported sleep hygiene behaviours identified in this study could serve as targets for interventions to promote sleep hygiene in patients with CKD. However, this study also demonstrates that other factors influencing sleep may not yet have been identified. Therefore, further research is needed to explore these factors to enhance sleep among individuals with CKD. Additionally, future studies should prioritise recruitment efforts targeting people with CKD who are not receiving dialysis to gain a more comprehensive understanding of the impact of sleep on this population.






