INTRODUCTION
Multiple sclerosis (MS) has been traditionally considered a chronic, immune-mediated disease of the central nervous system (CNS).1 However, recent studies have highlighted the potential role of systemic factors, especially vascular comorbidities, in influencing disease progression.2,3 Vascular risk factors (VRF), including hypertension, diabetes, dyslipidaemia, obesity, alcohol intake, and smoking, have been associated with higher disease activity, greater lesion burden, faster brain atrophy, and earlier disability milestones in MS.4,5 While prior research has primarily examined the impact of VRFs on global MRI measures, their influence on specific CNS structural networks, such as the sensorimotor network (SMN), remains largely unexplored. Based on this background, the authors investigated the impact of VRFs on disability, motor performance, and the structural integrity of SMN regions in people with MS.6
METHODS
In this cross-sectional study, 268 patients with MS and 180 healthy controls (HC) were categorised based on VRF presence (HC-VRF[+]), MS-VRF[+]) or absence (HC-VRF[-], MS-VRF[-]). Disability and motor performance were assessed using the Expanded Disability Status Scale (EDSS), the Timed 25-Foot Walk, and the Nine-Hole Peg Test. Structural integrity of the SMN was evaluated using volumetric and diffusion-weighted MRI data. Specifically, the authors analysed cortical thickness of the primary motor and somatosensory cortices; normalised deep grey matter (GM) volume; volumes of the anterior (ACMA) and posterior (PCMA) cerebellar motor areas; fractional anisotropy (FA), mean diffusivity (MD), and lesion volume (LV) of the middle (MCP) and superior (SCP) cerebellar peduncles, the medial lemniscus, and the corticospinal tract; as well as the mean upper cervical cord area (MUCCA). Group differences in clinical and MRI metrics and interactions between disease status and VRFs were explored. In patients with MS, associations between clinical and MRI data were analysed, focusing on VRF influence.
RESULTS
At least one VRF was present in 74 (41.1%) HC and 179 (66.8%) patients with MS. Smoking was the most common VRF among patients with MS, affecting 53.0%. Unfortunately, HC and MS groups were not age-matched (p value corrected for false discovery rate [pFDR]=0.003), with HCs being younger. Nevertheless, compared to their relatives and HC groups, patients with MS exhibited greater lesion burden, global and regional brain atrophy (including deep GM and cerebellum), reduced cortical thickness, spinal cord atrophy, and widespread microstructural WM damage. MS-VRF[+] showed significantly more disability and a higher prevalence of progressive MS forms compared to MS-VRF[-] (pFDR≤0.004). A significant interaction between VRF and disease status was observed on walking capacity, manual dexterity, deep GM volume, ACMA volume, and medial lemniscus MD (pFDR≤0.039), suggesting an additive negative effect of VRFs on motor performance and the structural integrity of specific SMN regions. These findings are consistent with prior studies investigating individual VRFs’ impact on CNS structures.7-10 In patients with MS, higher EDSS scores were linked to damage across nearly all SMN regions (pFDR≤0.029). Notably, only for the medial lemniscus, the authors found a significant interaction effect between VRFs and FA of this tract in explaining disability (β:1.931, p=0.042; Figure 1). This result confirms the role of VRFs in worsening MS disability, and it is consistent with previous evidence showing that central pontine lesions are more strongly associated with ageing and vascular comorbidities, while peripheral lesions are more MS-specific.11
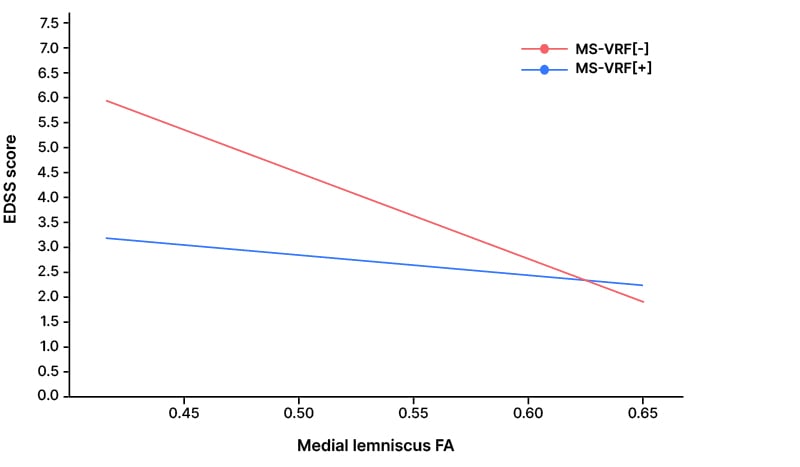
Figure 1: Scatter plot showing the association between medial lemniscus fractional anisotropy and Expanded Disability Status Scale scores in patients with multiple sclerosis, with (red) and without (blue) vascular risk factors.
EDSS: Expanded Disability Status Scale; FA: fractional anisotropy; MS-VRF[-]: patients with multiple sclerosis without VRFs; MS-VRF[+]: patients with multiple sclerosis with VRFs; VRF: vascular risk factors.
CONCLUSION
VRFs appear to exacerbate disability and motor performance, and contribute to structural and microstructural damage of specific SMN regions among patients with MS. Targeting modifiable VRFs may represent a promising strategy to mitigate their impact on MS progression.







