Interview Summary
For this article, EMJ conducted an interview with Ahmed Abdelmoity, Professor and Director, Division of Neurology, Children’s Mercy Kansas City, The University of Missouri-Kansas City, USA, in April 2025. Abdelmoity discussed the current treatment landscape for patients with drug-resistant epilepsy (DRE), navigating the unmet needs and integral challenges within patient management, including the need for clearly defined treatment algorithms and utilisation of non-pharmacological treatment modalities, as well as looking to future treatment approaches for patients who are non-responsive to anti-seizure medications (ASM).
DRUG-RESISTANT EPILEPSY AND THE TREATMENT GAP
DRE is defined as the failure of two tolerated and appropriately chosen antiepileptic drug schedules (either monotherapy or combination) to achieve sustained seizure freedom.1 Epilepsy affects approximately 50 million people worldwide, with an estimated third continuing to experience refractory seizures despite suitable intervention with ASMs.2-4 The majority of patients who achieve seizure freedom do so after their first or second ASM regimen, with any subsequently attempted ASM regimen having a diminished likelihood of seizure freedom.5
Abdelmoity emphasised the high burden associated with DRE, including “a decrease in quality-of-life metrics spanning mood and anxiety, behaviour, sleep quality, overall development and quality of life, and risk of sudden, unexpected death.”3,4 He highlighted the ‘treatment gap’: a discrepancy between patients diagnosed with epilepsy and those who have achieved seizure freedom with pharmacological management. Despite the increase in available ASMs over the last 40 years, Abdelmoity explained that the proportion of patients who remain refractory to pharmacological management remains at approximately 30%, consistent with earlier findings from the 1980s, when only a few treatment options were available.3–7
The treatment gap results in patient bottlenecks that are not being adequately managed to achieve seizure freedom. Consequently, there has been no significant improvement in disease prognosis over the past few decades, highlighting the need for enhanced action and realignment in the DRE management strategy.3-5
Currently, there are several non-pharmacological management options for the treatment of DRE, Abdelmoity explained. These range from surgical methods, including resective surgery or ablation, in which epileptic tissue is safely removed, to neuromodulation, which can be intracranial or extracranial, as well as dietary options. Despite the variety of available modalities, the treatment gap persists, and alternative non-pharmacological options such as resective surgery and neuromodulation remain underutilised.
MITIGATING THE TREATMENT GAP: EARLY REFERRAL AND TREATMENT ALGORITHMS
Referring to a 7-year analysis (2012–2019) from the National Association of Epilepsy Centers (NAEC), USA, Abdelmoity highlighted the marked increase in accredited centres, as well as epilepsy monitoring unit admissions, epilepsy monitoring unit beds, and epileptologists per million population served (Figure 1).8
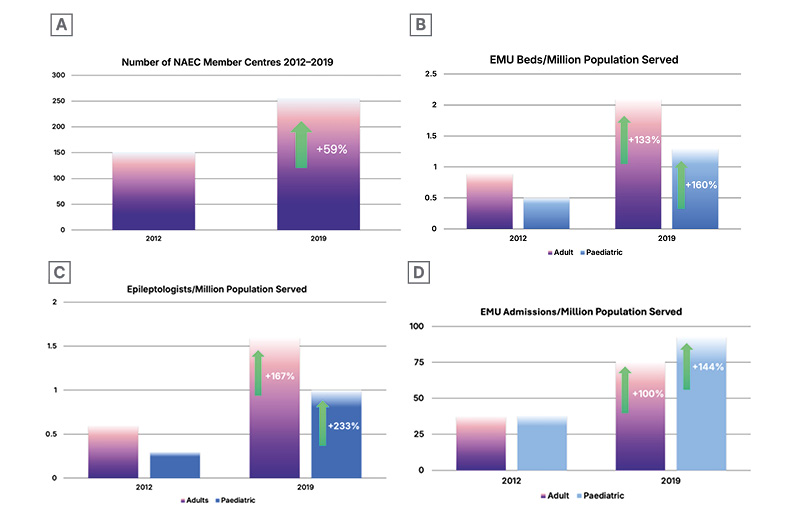
Figure 1: NAEC Centres, EMU Admissions, EMU Beds, and Epileptologists in Paediatrics and Adults from 2012–2019
A) Number of NAEC Centres, B) EMU Beds Per Million, C) Epileptologists Per Million, D) EMU Admissions Per Million
EMU: Epilepsy monitoring Unit, NAEC, National Association of Epilepsy Centres.
Data from Ostendorf et al.8
Although access to care, number of diagnoses, and the number of specialists have increased, Abdelmoity noted that certain non-pharmacological procedures have not increased at the same rate. Whilst responsive neurostimulation (RNS; +114%) and laser interstitial thermal therapy (+61%) increased, the number of temporal lobectomies and extratemporal resections lagged, whilst the overall amount of callostomies (-13%) and vagus nerve stimulation (VNS) procedures (-2.4%) decreased, contributing to an overall decrease in median volumes of procedures per centre.8 This may be due to several factors, Abdelmoity commented, including a delay in confirmed DRE diagnosis and establishing patient suitability for alternative, non-pharmacological treatments, as well as a lack of alignment across treatment centres in the decision-making process.
Early specialist referral is crucial for the optimal management of patients with epilepsy, particularly for DRE, in which patients are likely to benefit from the next level of care. However, Abdelmoity reflected that community and/or general neurologists might delay referral to a specialist centre. He speculated reasons for the delay, echoing the same problems: delays in establishing a DRE diagnosis, barriers preventing access to specialist centres, and a lack of a consistent treatment algorithm.
Abdelmoity explained: “The current variability is vast, allowing for a lack of consistency and inability to measure and compare outcomes of different treatments,” emphasising the need for an established DRE treatment algorithm that can be followed across treatment centres, defining the roles of the team and relevant pathways to enable early and prompt referral and streamlined patient care. He commented: “I think we simply need a better protocol that we can apply and implement across our epilepsy treatment centres.”
Regarding the application of potential treatment algorithms to broader epilepsy types, Abdelmoity stated that not only are they possible, but they are necessary. A broad algorithm, for example, would not need to define specific treatments or to be followed precisely at every centre, but would instead encourage timely consideration of alternative options at second ASM failure, he said. “Timeliness is so important; we shouldn’t keep waiting… it is important to manage and care for patients early, in a timely manner. It does not have to be precise and perfect.”
In his clinical practice, Abdelmoity’s multidisciplinary team (MDT) includes neurologists, epileptologists, and advanced nurse practitioners. His colleagues follow an algorithm based on the International League Against Epilepsy (ILAE) consensus guideline definition of DRE,1 which they continue to refine over time, based on supporting literature and real-world experience in their clinic.
MANAGING EXPECTATIONS AND SHARED DECISION-MAKING
Not only should treatment algorithms delegate the roles of the MDT and encourage timely specialist referral, Abdelmoity explained, but they should also encourage family and caregiver involvement. He explained that, ultimately, including the patient and caregiver in decision-making and managing expectations is key to achieving optimal treatment outcomes. He emphasised that: “Patients and families should be involved in decision-making from the start,” with the overarching goal of achieving seizure freedom through management. He outlined the importance of educating caregivers about DRE, the associated comorbidities and risks, including sudden unexpected death in epilepsy (SUDEP), as well as the benefits and risks of different treatments.
Abdelmoity shared that, in his clinical practice, they uphold a “triad of success” when navigating the patient journey with patients and caregivers (Figure 2). The triad of success consists of three pillars: be informative, compassionate, and assertive. Patients and caregivers often hold preconceived fears around alternative management methods, such as resective surgery and neuromodulation devices, Abdelmoity explained. “Caregivers may have fears around surgery and alternative methods of treatment. It is different to what they are used to (with ASMs), so it is important to communicate the benefits, side effects, and risks in an informative and constructive way early on, so they stay engaged and get involved.”
Figure 2: The Triad of Success.
Created with BioRender.com
SELECTING ALTERNATIVE TREATMENT APPROACHES
Abdelmoity emphasised that there is no one-size-fits-all approach to managing patients with DRE, particularly when considering surgical procedures or neuromodulation devices after the failure of ASMs. “These treatments are not mutually exclusive. It is a matter of what will work best for the individual patient to get them as close to seizure freedom as possible.” He cited findings from the 2-year PuLsE study, which demonstrated that patients with focal DRE who received VNS in adjunction to best medical practice (BMP) experienced a significantly increased health-related quality of life compared to that seen with BMP alone.9
For instance, in patients with lesional focal epilepsy, Abdelmoity recommended surgical management such as ablation or resective surgery after failure of a second ASM. For patients who are not suitable candidates for surgery, he recommended moving forward as early as possible onto neuromodulation, most likely VNS, given it is non-invasive, cost-effective, and accessible, with the additional benefit of a reported overall decrease in direct healthcare costs following VNS therapy.10
In a different situation, if a patient had a seed of focus in an eloquent cortex, for example, the neuromodulation device of choice would be RNS. Abdelmoity stressed that, as of now, no studies compare the different neurostimulation approaches head-to-head: VNS, RNS, and deep brain stimulation.
Looking to the future, Abdelmoity expressed hopes that the development of genomic medicines or new ASMs with clearly defined mechanisms of action could open the avenue to personalised precision medicines for patients with DRE. For now, Abdelmoity concluded that we must focus on what is readily available and approved for patients, working best with what we have today.
CONCLUSION
With approximately 50 million patients affected by epilepsy globally,2,3 one-third of whom are drug-resistant,3 Abdelmoity emphasised the need for a newly defined treatment algorithm to guide the management of patients with DRE. He stressed the importance of keeping patients and caregivers involved from diagnosis through to management considerations. Clinicians should maintain a compassionate, assertive, and informative approach while working collaboratively with their entire MDT. Prompt referral to specialised care is crucial, ensuring early access to alternative treatment options such as surgery and neuromodulation. Above all, after the failure of two ASMs in a patient, clinicians are encouraged to consider and initiate alternative treatment modalities as promptly as possible.







