Abstract
Aggressive angiomyxoma (AA) is a rare, locally invasive, benign tumour that mostly affects women of reproductive age. Its occurrence during pregnancy is extremely rare and may delay diagnosis due to its painless, gradual growth and resemblance to common vulvovaginal lesions. The authors report a 23-year-old primigravida who presented in active labour with a large vulval mass. The mass had progressively enlarged during pregnancy, causing discomfort in daily activities. An emergency lower segment caesarean section was performed after excision of the 30x21x10 cm mass. Histology confirmed AA. Postoperative recovery was uneventful, and the patient was discharged with plans for long-term follow-up. This case emphasises the clinical importance of AA during pregnancy, its potential to mimic other vulval lesions, and the necessity for surgical management and histopathological diagnosis, along with close follow-up due to its high risk of local recurrence.
Key Points
1. Aggressive angiomyxoma is a rare, locally infiltrative tumour that can enlarge significantly during pregnancy and mimic benign vulval lesions, delaying diagnosis and increasing the risk of obstructed labour and complex surgical intervention.2. This case report describes a 23-year-old primigravida who presented in active labour with a giant vulval aggressive angiomyxoma requiring emergency caesarean section and multidisciplinary surgical excision of a 30x21x10 cm mass.
3. Clinicians should maintain a high index of suspicion for aggressive angiomyxoma in enlarging vulval masses during pregnancy, as optimal management requires complete excision, histopathological confirmation, and long-term follow-up due to high recurrence rates.
INTRODUCTION
Aggressive angiomyxoma (AA) is a rare, slow-growing, but locally infiltrative mesenchymal tumour primarily affecting women of reproductive age and most commonly affecting the vulva, perineum, and pelvis.1 Its incidence in pregnancy is exceptionally uncommon, with only a few occurrences reported in literature. These tumours can develop to significant proportions and are usually distinguished by their painless, soft, gelatinous nature. They frequently resemble benign lesions such as Bartholin gland cysts, lipomas, or fibromas.1 Malignant transformation and distant metastasis are exceedingly rare during pregnancy, but must be investigated.2 In this context, the authors report a rare case of a giant vulval AA discovered during pregnancy, which resulted in obstructed labour and necessitated an emergency caesarean section followed by surgical excision of the mass.
CASE PRESENTATION
A 23-year-old primigravida at 37+3 weeks of gestation was brought to a gynaecological emergency room with complaints of labour pains and the presence of a large obstructing vulval mass. She noticed a pea-sized mass in the vulva during her first trimester and, over the duration of her pregnancy, the mass progressively enlarged in size, beginning to interfere with her daily activities. Notably, she had a similar vulval swelling 2 years prior, which resolved with oral medication. This recurrence was temporally associated with hot-wax hair removal, after which she opted not to seek treatment due to concerns regarding fetal harm. As the patient presented directly to the emergency department in active labour, there was no opportunity to perform any advanced imaging such as CT or MRI. Only a routine obstetric ultrasound was undertaken to assess fetal well-being. Given the obstructed labour and need for urgent intervention, surgery could not be delayed for further imaging. Additionally, the patient was unbooked, limiting the availability of prior antenatal investigations. The patient had been prescribed progesterone support by her local general practitioner due to suspected preterm labour, as she reported experiencing intermittent lower abdominal pain during pregnancy. She was also given multiple courses of antibiotics by the same practitioner, prescribed prophylactically in anticipation of a possible underlying infection, although no confirmed diagnosis was documented.
She was haemodynamically stable at the time of admission. Abdominal examination revealed a term-sized uterus consistent with the symphysio-fundal height, with normal fetal heart sounds and movements. Vaginal examination revealed a 5 cm dilated cervix with a soft, anterior os, but significant obstruction at the introitus due to the vulval mass. In view of the obstructed labour and patient preference for mass removal, a decision was made to proceed with emergency lower segment caesarean section and concurrent excision of the mass under general anaesthesia. Intraoperatively, the uterus showed signs of obstructed labour (Bandl’s ring was observed). A healthy 3 kg male infant was delivered with good Appearance, Pulse, Grimace, Activity, and Respiration (Apgar) scores.
The mass, measuring 30x21x10 cm (Figure 1), was excised by a combined gynaecology and plastic surgery team using sharp and blunt dissection. It was noted to have both cystic and solid components. Excess vulval skin was excised, and the defect was closed primarily with adjacent skin flaps using sutures. A closed-suction drain was placed, and an aseptic dressing was applied. The total surgery time spanned approximately 4–5 hours.
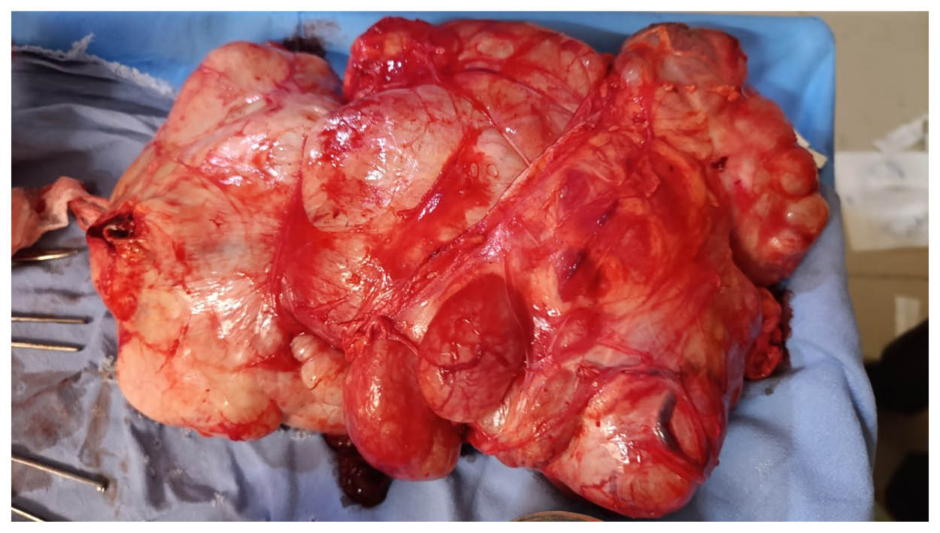
Figure 1: Vulval mass measuring 30x21x10 cm at 37+3 weeks gestation.
Postoperatively, the patient was monitored in the ICU on ventilatory support due to the prolonged duration of anaesthesia, but was successfully extubated and transferred to the general ward within 24 hours. She started on broad-spectrum antibiotics, iron supplementation, and was advised on wound care with sitz baths using warm water, hydrogen peroxide, and povidone-iodine. Iron supplementation was continued throughout the patient’s pregnancy, as empirical iron therapy is routinely practised in the authors’ region due to the high prevalence of iron deficiency among pregnant women. Although commonly administered, the patient herself was not anaemic. She was discharged on the fifth postoperative day with instructions for follow-up on Day 7 for suture and drain removal.
Histopathological examination of the excised mass confirmed the diagnosis of AA, a rare, locally infiltrative mesenchymal tumour known for its recurrence rate in women of reproductive age. The patient was counselled extensively about the benign, yet locally aggressive, nature of the tumour; the potential for recurrence; and the need for long-term surveillance, including routine imaging and clinical evaluation.
DISCUSSION
AA is a rare, benign, hormonally sensitive mesenchymal tumour that primarily affects women of reproductive age.3 While women of reproductive age account for the majority of cases, there are occasional occurrences in premenstrual women and children. This can be explained by the tumour hormone’s responsiveness, as its growth is promoted by oestrogen and progesterone.4 In the present case, the patient had received progesterone support during pregnancy, which may have contributed to the tumour’s growth due to its hormonal sensitivity. The tumour is primarily found in the pelvic and perineal area. Uncommon locations include the orbit, larynx, liver, and lung.5 The tumour may occur in male patients, in sites such as the inguinal canal and scrotum.6 The female to male ratio is 6:1.6 Although its pathophysiology is unclear, the high mobility protein isoform C, which is associated with DNA transcription, has recently been shown to have atypical manifestations as a result of a translocation at the level of chromosome 12.7
Typically, AA manifests as a soft, compressible, progressive vulvar or perineal tumour. It displaces pelvic organs and is encapsulated, extending into the paravaginal, pararectal, or retroperitoneal regions. It looks grey, glossy, and uniform, with potential bleeding and necrosis, on gross examination. Under a microscope, it has a loose myxoid stroma with mesenchymal cells that are stellate and spindle shaped, distinctive, irregularly distributed blood vessels and peripheral finger-like projections. Mitoses rarely occur. Smooth muscle actin, desmin, and vimentin show positive immunohistochemistry, which suggests fibroblastic or myofibroblastic origin.8
It is frequently misdiagnosed as a vulvar abscess, Bartholin’s cyst, vaginal prolapse, vaginal mass or polyp, pelvic floor hernia, and more on clinical inspection.9 In this case, multiple empirical courses of antibiotics were prescribed by local practitioners under the assumption of an infectious aetiology, delaying accurate diagnosis and definitive management. To determine the tumour’s extent and schedule surgical removal appropriately, preoperative imaging is crucial. It appears as a cystic or hypoechoic mass on ultrasound.10 On MRI and CT, the bulk exhibits a clear characteristic of layered and swirling tissue with alternating low and high signal strands, which represent the tumour’s myxoid and fibrous septa.11 These imaging results make it easier to accurately estimate the depth and margins of the tumour, which is essential when planning a wide local excision to decrease the likelihood of it reoccurring.12 The infiltrative nature of the tumour and its proximity to important tissues make its total excision difficult.12
Gonadotropin-releasing hormone agonists (e.g., triptorelin, leuprolide) and antagonists (relugolix) target oestrogen and progesterone receptors, and have demonstrated potential in preoperative tumour volume reduction, residual disease treatment, and recurrence management.13 In cases of resistance, aromatase inhibitors may also be helpful when used with gonadotropin-releasing hormone agonists.14
CONCLUSION
AA is a rare, hormonally sensitive, and locally infiltrative mesenchymal tumour that presents significant diagnostic and management challenges, especially during pregnancy. Delays in detection are frequently caused by its benign histology, slow growth, and clinical resemblance to common vulvovaginal lesions. This case highlights the importance of maintaining a high index of suspicion for AA in women presenting with enlarged vulvar masses, especially during pregnancy. Hormonal therapy can help reduce the size of the tumour and manage its recurrence. For optimal management, timely imaging, multidisciplinary surgical planning, and histological confirmation are crucial.







