BACKGROUND AND AIMS
Quality improvement (QI) has proven instrumental in identifying and addressing systemic changes in healthcare, yet its application in medical education remains limited. The authors hypothesize that QI interventions can be effectively adapted to enhance didactic medical education. Here, they describe their experience applying QI strategies to improve an extracurricular journal club known as the “Sweet Hour Journal Club”. This was a monthly extracurricular session led by a volunteer resident or faculty member, discussing a publication of interest in pulmonary and critical care. Held after hours (5:15 p.m.–6:00 p.m.) in the residency lounge, prereadings were distributed via email the week prior, and both faculty and residents were invited to attend optionally. Desserts were provided per the presenter’s request.
METHODS
The authors employed QI methodologies, including process mapping, plan-do- study-act (PDSA) cycles, and run charts, to strengthen the extracurricular Journal Club didactic series.
Process mapping revealed that the after-hours timing and the requirement of prereadings likely contributed to decreased attendance and engagement rates. Additionally, qualitative interviews with attendees and volunteer presenters identified residents’ intimidation in discussing methodology and statistical analysis as a barrier to presenting at the club.
During the first PDSA cycle, the Sweet Hour Journal Club was rescheduled to a bimonthly optional session held during the noon break (12:00 p.m.–1:00 p.m.). In the second cycle, prereadings were eliminated, and guest speakers were invited to act as study critics, facilitating discussions on study methodology and result generalizability. In the final PDSA cycle, a critical appraisal worksheet was integrated into each session, enabling learners to actively document their thoughts on study randomization, internal and external validity, and result interpretation (e.g., number needed to treat, number needed to harm, and statistical and clinical significance).
RESULTS
Following these interventions, the authors’ run chart (Figure 1) indicated a trend toward higher attendance rates with each successive PDSA cycle.
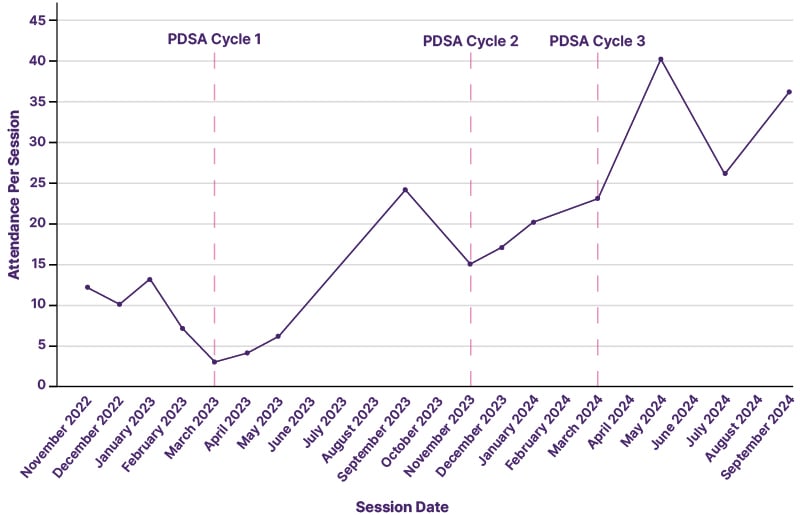
Figure 1: Attendance per “Sweet Hour Journal Club” session.
PDSA: plan-do-study-act.
CONCLUSION
QI methodologies can enhance curricular design and didactic medical education. Further studies are needed to determine if such interventions lead to higher knowledge retention and learner engagement compared to traditional didactic methods.







