Meeting Summary
COPD is a growing problem worldwide. Symptoms of COPD may lead to exacerbations, which are associated with an increased incidence of cardiovascular (CV) events. This association is important to recognize as both COPD exacerbations and the presence of cardiovascular disease (CVD) are associated with an early death. At the 2025 American Thoracic Society (ATS) Conference, Nicola Hanania, Baylor College of Medicine, Houston, Texas, USA, and Patrick Cambier, HCA Florida Trinity Hospital, Trinity, Florida, USA; Interventional Cardiology Consultants, Clearwater, Florida, USA, presented the case for examining CV-related issues in all patients with COPD. Studies show that a COPD exacerbation is one of the key symptoms associated with further exacerbations. As such, intervention either prior to any exacerbation, or following the first such incidence, is key to trying to limit both further exacerbations and associated CVD. However, even at-risk patients with COPD are being undertreated, especially with regard to maintenance therapy. This, the experts posited, may pose a significant health burden. Hanania and Cambier also discussed that the assessment of CVD symptoms in patients with COPD is not routine. They called for cardiologists and pulmonologists to work together and cross-refer patients whenever they present with COPD. This approach can not only reveal CV-related issues in patients with COPD, but can also lead to more proactive, early treatment of such symptoms to slow disease progression and help prevent death.
Introduction
It is becoming increasingly recognized that people with COPD have an elevated risk of serious CV events,1 discussed Hanania and Cambier at the ATS 2025 conference. Such CV events can include myocardial infarction, arrhythmia, stroke, heart failure decompensation, and death.1 For example, analysis of 1999–2018 National Health and Nutrition Examination Survey data, representing over 31,500 adults, found that while the prevalence of CVD in people without COPD was around 9%, CVD prevalence in people with COPD (n=2,504) was higher: 17.5% in those with chronic bronchitis, 37.2% in those with emphysema, and 36.1% in those with both.2 “The magnitude of difference speaks to the idea that there is a ‘scarlet letter’ of concurrent pulmonary disease and [shows] why people [with COPD] need to be looked at much more upstream, treated much more aggressively, and watched a little bit more closely,” explained Cambier.
COPD Symptoms as Risk Factors for Exacerbations
Figure 1 shows findings from a retrospective analysis of nearly 60,000 patients with COPD in the UK. Here, increasing dyspnea severity at initial assessment is shown to be related to the risk of having ≥1 moderate-to-severe exacerbations in the following 12 months.3 This is of clinical importance, discussed Hanania, as analysis of nearly 1.5 million patients in the US showed that once a person has experienced an exacerbation, they are at a 1.5-fold risk of a future exacerbation following a single incidence, and a 2.5-fold risk following multiple exacerbations.4
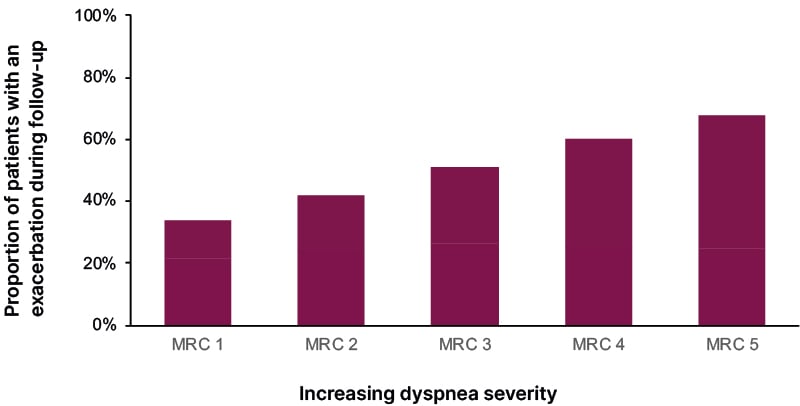
Figure 1: Increasing COPD symptoms are associated with an associated risk of exacerbations.3
MRC: Medical Research Council dyspnea grade.
Occurrence of COPD exacerbations is of importance, as analysis of IQVIA Longitudinal Access and Adjudication Data (LAAD) for this session, which utilized US pharmacy and medical claims information from January−December 2024, reveals that 42% of “at-risk” patients with COPD (defined as ≥2 moderate or ≥1 severe exacerbations in 12 months) attended an emergency room or urgent care center in a 12-month period, with 37% of these patients being hospitalized. Following hospitalization, 30-day readmission rates for all patients with COPD was 20%.5
Also of note, the risk of all-cause mortality is higher following an exacerbation. In a study including almost 436,000 newly diagnosed patients with COPD in the US, compared to patients who had not experienced an exacerbation, the hazard ratio (HR) for mortality within 30 days of the first exacerbation was 1.79 (95% CI: 1.58–2.04), with the risk of death remaining elevated for up to 2 years (HR: 1.15; 95% CI: 1.05–1.25).6 In the IQVIA LAAD analysis of patients at-risk of exacerbations, 30-day mortality was 9% following a hospitalization for COPD.5 In addition, a study utilizing US data from just under 1.3 million hospital admissions for COPD found that, following discharge, 26.2% of patients died within 1 year.7 “To summarize, symptoms drive exacerbation; one exacerbation drives a further exacerbation, and then it’s a vicious cycle,” said Hanania.
The Relationship Between Cardiovascular Disease and COPD
As can be seen from Figure 2, there is substantial supporting data that COPD exacerbations are associated with CV events, and both are associated with an early death. There are also indications that COPD symptoms alone may be associated with CV events.1 Recognizing these interactions, said Cambier, should encourage pulmonologists and cardiologists to work together, so that “we can […] be more effective in keeping people [with COPD] out of scenarios where they’re coming into the hospital.”
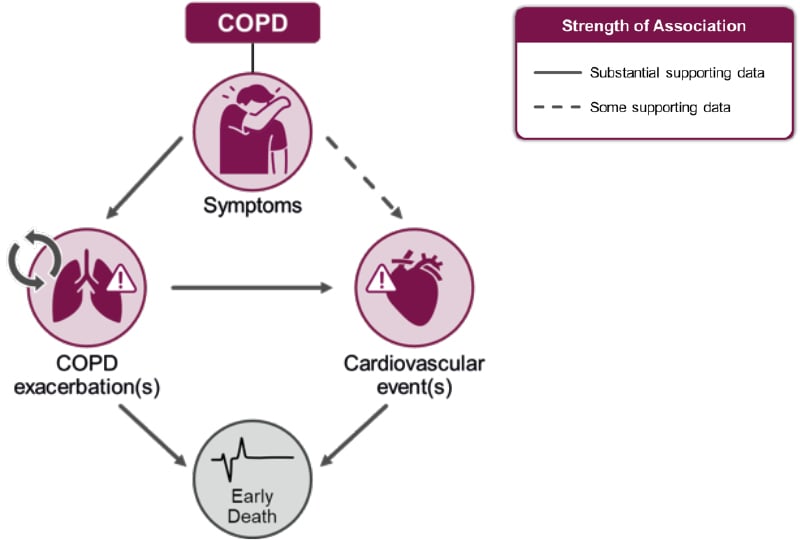
Figure 2: Associations between COPD and cardiovascular events may lead to early death.1
Adapted from Singh D et al.1
Licensed under CC BY-NC 4.0. COPD-associated cardiopulmonary risk.
The interrelationship between CVD and COPD is partly due to shared “syndemic” risk factors, such as smoking and aging, as discussed in the 2025 Global Initiative for Chronic Obstructive Lung Disease (GOLD) report.8 Other shared mechanisms for this relationship, Cambier and Hanania suggested, could include air trapping, hyperinflation, and inflammatory pathways.1
COPD Exacerbations as Risk Factors for Cardiovascular Disease
A global assessment of mortality and morbidity in patients with COPD who had CVD, or an increased CVD risk, found that the HR of a CV event in the 30 days following a moderate or severe COPD exacerbation was 3.8 (95% CI: 2.7–5.5). While the risk decreased over time, it remained above 1.0 for around a year (HR: 1.9; 95% CI: 1.5–2.4 at 91−365 days; Figure 3).9 Findings such as this, reported Hanania “have opened [pulmonologists’] eyes to start discussing things with our cardiology colleagues.”
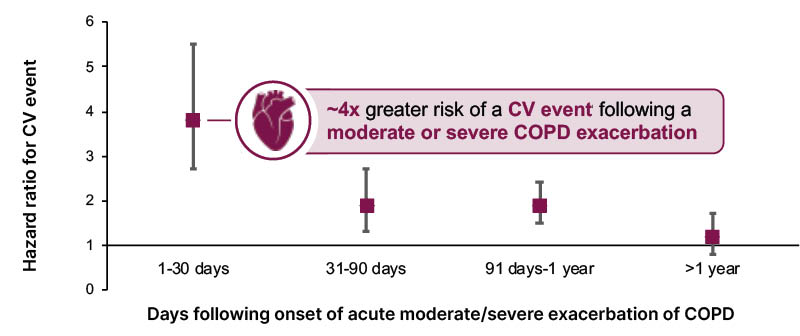
Figure 3: Increased risk of cardiovascular events persisted for up to a year after an exacerbation.9
CV events included myocardial infarction, stroke, unstable angina, transient ischemic attack, and death.
CV: cardiovascular.
However, Cambier relayed that he currently has two patients with COPD in the ICU for an exacerbation, who have never seen a cardiologist or recently undergone CV-focused tests. This highlights, he continued, how such patients are “simply being looked upon as [only having a] COPD exacerbation”. He explained that what potentially happens is that “we get into our track, and we see [a patient’s symptoms] as a singular disease, when in fact, they have an intimately connected comorbidity.” Of course, Hanania added, “we should be worried about the respiratory symptoms during [a COPD] exacerbation […] but we should also be worried about their heart.” This shows the need, Cambier reiterated, for “upstream recognition to be aggressive earlier, rather than just tide [patients] over, because the next [exacerbation] could be worse.”
Considering Cardiopulmonary Risk When Managing COPD
The evidence regarding the relationship between COPD and CVD, said Cambier, is “why we need to make sure we make adjustments in medications, or at least rethink what we’re treating patients with at [early] stages, because the next day they may have an even more dire outcome.” However, undertreatment is another major issue related to the under-recognition of COPD and CVD comorbidity, explained Hanania. For example, in an analysis of IQVIA LAAD claims data, only 50% of at-risk patients with COPD (≥2 moderate or ≥1 severe exacerbations in 12 months) were receiving maintenance treatment, and only 28% were receiving triple therapy with a long-acting β agonist, long-acting muscarinic antagonist, and inhaled corticosteroid.5 “Undertreatment poses a significant health burden in terms of maintenance,” commented Cambier.
Alongside appropriate drug therapy for both treatment and prevention of CV-related issues, the experts discussed how pulmonary rehabilitation may be useful for patients with comorbid COPD. Treatment, said Cambier, may also involve prompt initiation of proactive drug therapy, for example, low-density lipoprotein reduction in a patient with Class I−II heart failure. These patients may currently, in Cambier’s view, be considered to be in heart failure with only mildly reduced left ventricular function, but downstream this could lead to biventricular failure. At the moment, however, he reported that such patients may be “grossly undertreated” and possibly receiving only low doses of appropriate medication.
The Importance of Early Identification of At-risk Patients
With these figures in mind, Hanania stressed the importance of identifying at-risk patients,10,11 such as those with a recent history of COPD exacerbations,3 and then optimizing management,8,11 to prevent exacerbations, CV complications, and decrease mortality risk.8 CV issues should be investigated, said Cambier, alongside other commonly considered COPD-related diseases, such as diabetes.8 Timing of care is particularly important, and the latest GOLD report highlights how a more proactive disease management approach with appropriate evidence-based treatments can help improve outcomes.8
Cambier stressed the need to take any opportunity, when a patient with COPD presents, to carry out a range of CV-associated investigations. “Don’t be bashful about ordering CV testing,” he urged, and “look at other signs and symptoms of [for example] right heart failure, such as hepatic congestion, etcetera.” As an example, returning to his patient with COPD in the ICU, Cambier related how relatively high levels of brain natriuretic protein were discovered. Following an echocardiogram, the patient was found to have poor left ventricular function as well.
Cambier recognized that pulmonologists may feel this is more appropriately initiated by the patient’s primary care provider, but advised that pulmonologists can also send patients with COPD to a cardiologist for assessment of their ischemic burden. However, issues can arise, as discussed during open questions and answers, as in some cases, tests such as calcium screening and a chest CT scan have to be ordered separately, and the result of one may influence whether or not the next test can be undertaken.
Another query that arose during the discussion concerned which biomarkers should be used to assess COPD over time. This is an “important point, which is an unmet need,” said Hanania. “More strategies [are needed], from both the cardiology societies and lung societies, to come up with a consensus as to what biomarkers to follow.” For example, he said, the U.S. FDA12 have “adopted fibrinogen as the only biomarker they believe in for now for COPD, but there are more, and I think we need to work together to find a solution.”
Conclusion
“Certainly, we have to treat patients [with COPD] if they already have CV risk factors,” concluded Hanania; however, he continued, in people with COPD, between the pulmonologist and the cardiologist, “we need to see if, by interacting first and early, we can prevent the late [COPD] events and the CV events.”







