BACKGROUND AND AIMS
Environmental air pollution has been linked to the pathogenesis of rheumatoid arthritis (RA).1 Nevertheless, there is no evidence linking higher concentrations of air pollutants with the risk of RA reactivations. The primary objective of this study was to determine the association between concentration of air pollutants and RA disease relapses. Revealing the possible connections between air pollutants and inflammatory arthritis severity and their chances to progress or relapse might help predict treatment response and healthcare utilisation of such patients.
MATERIALS AND METHODS
The study data on patients with RA was extracted from the registry of biological therapies at the University of Verona, Italy. The authors retrospectively collected longitudinal data of patients affected by RA starting from September 2013 to September 2018. They also collected data on the daily concentration of air pollutants in the Verona area from this time frame. The following air pollutant concentrations (µg/m3) were available: carbon monoxide (CO), nitrogen oxide (NO), nitrogen dioxide (NO2), nitrogen oxides (NOx), particulate matter <10 µm (PM10), ozone (O3), and particulate matter <2.5 µm (PM2.5).
The authors analysed the concentration of exposure to pollutants as area under the curve and mean concentration during the 30-day and 60-day periods before the appointment with the rheumatologist. The authors conducted a cohort cross-sectional analysis to determine the association between C-reactive protein (CRP) serum levels and the concentration of air pollutants. A case-crossover study can be used when brief exposures cause a transient change in risk of an acute-onset disease or reactivation of such diseases.2 In case-crossover studies, instead of obtaining information from two groups (cases and controls), the exposure information is obtained by comparing two different periods of time in the same group of patients followed longitudinally.
RESULTS
The authors collected data from 888 patients with RA who had 3,396 follow-up visits and 13,636 daily air pollution records from June 2013 to September 2018. From the general cross-sectional analysis of the overall cohort, the authors found that patients in non-remission (≥2.6 and >3.2 disease activity score 28 [DAS28]-CRP) and high CRP (≥5 mg/L) were frequently exposed to greater concentration of air pollutants when compared to patients in remission or low disease activity (<2.6 or ≤3.2 DAS28-CRP) and patients with low CRP levels. Patients exposed to PM10 concentrations ≥50 μg/m3 had a 70% higher risk of having CRP levels ≥5 mg/L (odds ratio: 1.696; 95% confidence interval: 1.245–2.311). Among patients with RA, 440 patients (49.5%) had at least two follow-up visits with a difference in DAS28-CRP of more than 1.2 points (with current DAS28-CRP ≥3.2) serving as the sample for the case-crossover study. All air pollutants concentrations were significantly higher in the hazard period when compared to control period (Table 1).
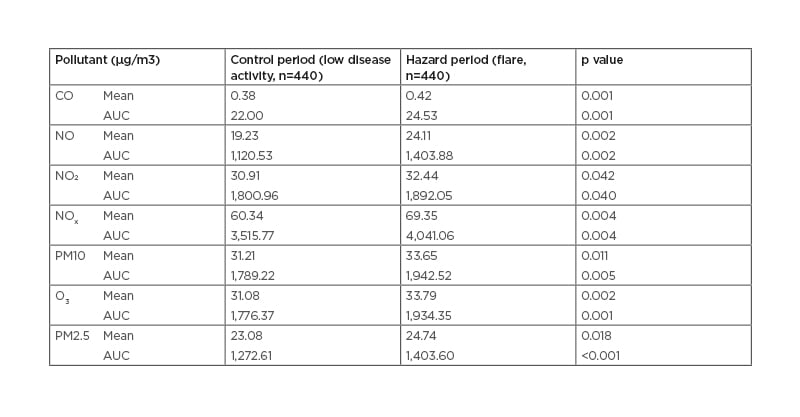
Table 1: Case-crossover study.
Mean of concentrations (mean and the AUC) of air pollutants in the 60 days before low-disease activity and flare visit (DAS28-CRP difference >1.2).
AUC: area under the curve; CO: carbon monoxide; CRP: C-reactive protein; DAS28: disease activity score; NO: nitrogen oxide; NO2: nitrogen dioxide; NOx: nitrogen oxides; O3: ozone; PM2.5: particulate matter <2.5 µm; PM10: particulate matter <10 µm.
CONCLUSION
The authors studied the association between air pollution and RA disease severity and reactivation in a cohort of patients followed longitudinally for more than 5 years. In patients with RA, the exposure to high levels of air pollutants (i.e., CO, NO, NO2, NOx, PM10, O3 and PM2.5) was associated with increased CRP levels and higher risk of experiencing a flare of arthritis.








