BACKGROUND
Axial spondyloarthritis (axSpA) is a chronic inflammatory disease that can lead to irreversible structural damage. Assessing new bone formation (NBF) in the spine and its progression is crucial but currently relies on radiography,1 which has limited sensitivity to change. Novel imaging techniques, such as MRI-based synthetic CT (sCT) and low-dose CT (ldCT) have been shown to perform better than radiography in detecting NBF in the spine.2 Psoriatic arthritis (PsA) shares similarities with axSpA but is also described to exhibit distinct axial joint manifestations.3 Nonetheless, data on these patterns of axial involvement in PsA remains scarce, particularly regarding imaging findings from ldCT. Additionally, the potential of sCT to visualise these structural axial lesions without radiation exposure, as accurately as ldCT, has yet to be explored.
OBJECTIVE
This study aims to 1) describe the occurrence of different types of NBF in the spine in patients with axSpA, PsA, and rheumatoid arthritis (RA), and in healthy controls (HC) using ldCT; and 2) determine the sensitivity and specificity of sCT to detect NBF with ldCT as the reference standard.
METHODS
Patients meeting the Assessment of SpondyloArthritis International Society (ASAS) classification criteria for axSpA, or the Classification Criteria for Psoriatic Arthritis (CASPAR) criteria for PsA, or the European Alliance of Associations for Rheumatology (EULAR)/American College of Rheumatology (ACR) 2010 criteria for RA were included, along with HC without a history of chronic back pain. All participants underwent ldCT and MRI of the entire spine. sCT was reconstructed using the BoneMRI v1.8 (MRIGuidance B.V., Utrecht, the Netherlands) application, a quantitative 3D MRI technique that generates CT-like MR images. Images were pseudonymised and scored separately for ldCT and sCT by a reader blinded to all other clinical and diagnostic information. NBF types were defined prior to image evaluation: marginal syndesmophyte, non-marginal syndesmophyte, and osteophyte (Figure 1).
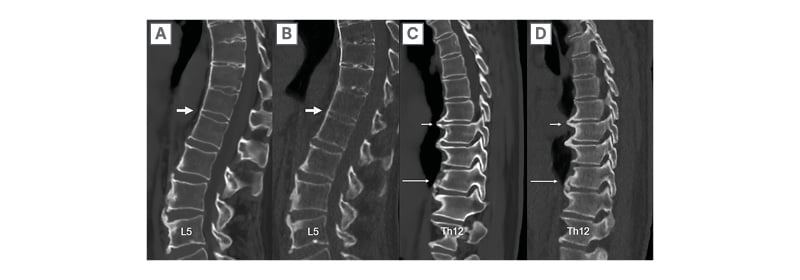
Figure 1: Types of new bone formation, as seen on MRI-based synthetic CT and low-dose CT.
MRI-based synthetic CT (A) and low-dose CT (B) of the lumbar spine and part of the thoracic spine in a patient with axial spondyloarthritis.
Thick arrows: bridging marginal syndesmophyte originating from the corners of L1 and L2, with a vertical orientation at origin (>45 degrees measured from the endplate).
MRI-based synthetic CT (C) and low-dose CT (D) of the thoracic spine in a patient with psoriatic arthritis.
Short arrows: osteophytes originating horizontally (<45 degrees) from the lower corner of Th7 and upper corner of Th8.
Long arrows: non-marginal syndesmophyte originating vertically above the corner of Th10.
RESULTS
Sixty-eight participants (33 females; mean age: 52) were included: 30 with axSpA, 19 with PsA, 9 with RA, and 10 HC. On ldCT, marginal syndesmophytes were most frequently scored in the axSpA group (343 lesions out of 4,140 possible; 8.3%). For non-marginal syndesmophytes, the highest score on ldCT was also found in patients with axSpA (186 lesions out of 2,760; 6.7%) compared to 1.8% in the PsA group, 4.1% in the RA group, and 2.6% in HC. Osteophytes were the most frequently scored type of NBF on ldCT in all groups, with the highest prevalence in the RA group (16.4%) and the lowest in the axSpA group (8.7%). The thoracic spinal segment had the highest sum scores for all NBF types, with the lesions primarily located at the anterior corners. Using ldCT as the reference standard, the sensitivity of sCT to detect any type of NBF in the spine in all groups was 0.69, with a specificity of 0.96 and an accuracy of 0.92. The sensitivities of sCT to detect marginal syndesmophytes, non-marginal syndesmophytes, and osteophytes were 0.57, 0.39, and 0.50, respectively (all with specificities and accuracies >0.90)
CONCLUSION
Marginal and non-marginal syndesmophytes were more frequently observed in patients with axSpA. No pathognomonic pattern emerged to differentiate participants with PsA, RA, and HC. Osteophytes were the most common NBF type across all groups, predominantly located in the thoracic spine. sCT demonstrated excellent specificity (≥0.94) and accuracy in detecting all NBF types when using ldCT as the reference standard, and a moderate sensitivity. However, the sensitivity to detect any type of NBF was good, highlighting the large potential of this innovative sCT imaging technique for future assessment of spinal NBF, and changes therein over time, in trials and practice of patients with spondyloarthritis.







