BACKGROUND AND AIMS
According to the European Association of Urology (EAU) Guidelines, tumour size exceeding 2 cm serves as a crucial factor in stratifying high-risk upper urinary tract urothelial carcinoma (UTUC) cases, prompting the recommendation of nephroureterectomy.1 However, in scenarios involving a solitary kidney, bilateral disease, or significant comorbidities, a conservative (kidney-sparing) surgical approach is considered.1 Notably, ureteroscopic treatment has demonstrated promising short-term oncologic outcomes in managing large, multifocal, low-grade UTUC.2 Yet, to effectively stratify risk for this subset of patients, there remains a critical need for long-term data on progression and survival rates.
MATERIALS AND METHODS
A previously published cohort analysis2 was analysed on a selective population of patients diagnosed with high-volume, low-grade urothelial carcinoma (upper tract tumour burden >3 cm) between 2002–2011. This database was updated through 2023 to include long-term outcomes.
Patients were stratified into two groups. Group 1 (ureteroscopic treatment), comprised those with a solitary kidney, bilateral disease, and patients who chose endoscopic therapy because of major comorbidities. Fifty-three percent (9/17) of the patients in Group 1 had a solitary kidney at the time of presentation. Group 2 (nephroureterectomy) included those treated according to established guidelines.
Demographic, clinical, and pathological data were collected, and a thorough longitudinal follow-up extending up to 20 years was conducted, including assessments of recurrence rates, disease progression, and overall survival.
RESULTS
Among the 160 patients diagnosed with UTUC during this period, 45 (28.12%) were identified as high-volume, low-Grade urothelial carcinoma; 17 (37.5%) of these patients were in Group 1, with nine (53%) having a solitary kidney (Table 1). The median follow-up period was 16.8 (range: 14.8–20.0) years, and 11.2 (8.0–15.4) years (p<0.01). Group 1 underwent significantly more ureteroscopy procedures, with 10.2 (6.0–12.0) compared to 6.1 (4.0–10.0) in Group 2 (p=0.03). Estimated overall survival rates (years) in Groups 1 and 2 were not statistically significantly different between the two groups (Table 1). Group 1 patients progressed to high-grade disease in 50% of patients over 15 years (Table 2).
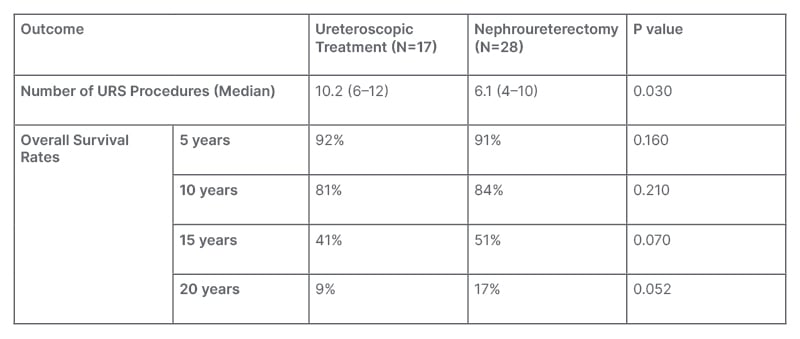
Table 1: Survival analysis.
URS: ureteroscopy.
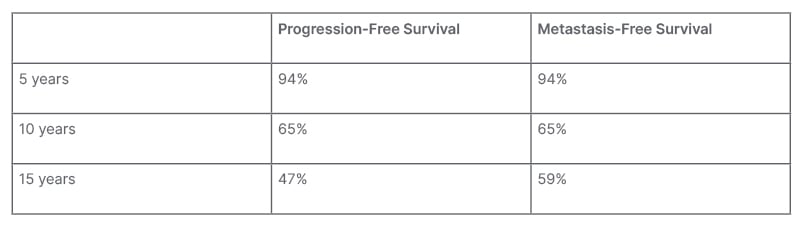
Table 2: Ureteroscopy progression and metastasis.
CONCLUSION
The authors’ study presents the longest follow- up of patients with high-volume, low-grade UTUC, who have been treated with endoscopic management. This elderly population has no statistically significant difference in overall survival at 10-, 15-, and 20-years of follow-up. Ureteroscopic treatment with surveillance is not only technically feasible, but is a reasonable alternative to nephroureterectomy in the elderly, high-risk patient population over long-term follow-up. Patients should be counselled that there is around a 50% chance of progression in Grade during 15-year surveillance, underscoring the need for continued ureteroscopic surveillance in this cohort. Patients must also be aware that progression in Grade commonly reflects progression in Stage and metastatic disease, but may not impact the overall survival in this subset of older patients.







