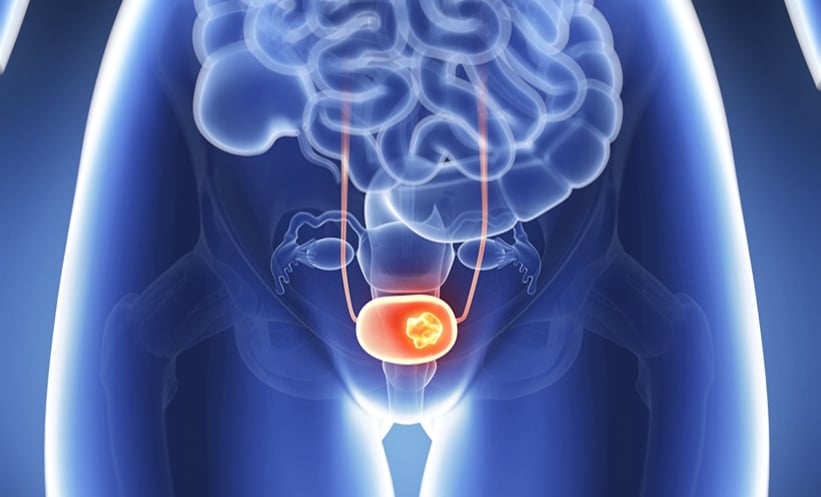
MUSCLE-INVASIVE bladder cancer (MIBC) is a particularly aggressive and life-threatening form of bladder cancer, distinguished by its invasion into the muscle layer of the bladder wall. Affecting roughly 20–25% of patients with bladder cancer at diagnosis, MIBC poses a major clinical challenge due to its high recurrence and progression rates, even with standard treatments such as radical cystectomy and chemotherapy. Globally, bladder cancer accounts for an estimated 550,000 new cases and 200,000 deaths each year.
MIBC is more prevalent in men, with a 3:1 male-to-female ratio, and typically presents in individuals aged 65–70. Despite aggressive interventions, the five-year survival rate remains below 50% for those with localised disease and plummets to less than 15% when metastasis occurs. Smoking is the leading modifiable risk factor, contributing to up to half of all cases, while occupational exposure, chronic infections, and prior pelvic radiation also increase risk.
Symptoms such as painless haematuria (blood in urine), dysuria, frequent urination, and nocturia are often misattributed to benign urological conditions, delaying diagnosis. This is especially dangerous given MIBC’s rapid spread to adjacent organs and distant sites like the liver and lungs.
Early and accurate detection is vital. Diagnosis typically involves cystoscopy and biopsy, supported by imaging techniques such as CT or MRI. Molecular subtyping, categorising tumours based on genetic expression, has advanced personalised treatment, but remains inaccessible in many settings due to cost.
As a more practical alternative, clinicians are increasingly relying on histopathology combined with immunohistochemistry (IHC). Markers such as GATA3 (luminal subtype) and KRT5/6 or p63 (basal/squamous subtype) help approximate tumour behaviour and guide treatment.
Incorporating IHC into routine diagnostics provides a cost-effective, accessible method to personalise care and improve outcomes for patients with this complex disease. While molecular profiling remains the gold standard, histology and IHC offer a promising path forward in managing MIBC across diverse clinical environments.
Reference
Attanasio G et al. Histological and immunohistochemical approaches to molecular subtyping in muscle-invasive bladder cancer. Front Oncol. 2025;15:1546160.