Interview Summary
Atopic dermatitis (AD) is a common, chronic inflammatory skin disease that presents heterogeneously across patients. It carries a high disease burden, with symptoms such as pruritus (itch) severely affecting patients’ quality of life. Despite advances in AD treatments, patients who are sub-optimally managed may continue to experience residual disease burden. Novel frameworks for AD management, such as the Aiming High in Eczema/Atopic Dermatitis (AHEAD) consensus recommendations, as well as clinical guidelines and consensus statements in different countries, advocate aiming for higher treatment goals, such as minimal disease activity (MDA). MDA represents the concomitant achievement of optimal treatment targets on both a clinician-reported outcome (ClinRO) and a patient-reported outcome (PRO). Achievement of MDA is associated with better PROs and improvement in quality of life compared to patients who do not achieve it. In addition, patients who achieve MDA experience fewer, shorter flares, and fewer healthcare visits compared to those who do not achieve MDA. Recent research discussed in this article by experts Yousef Binamer, Chairman, Department of Dermatology, King Faisal Specialist Hospital & Research Center, Riyadh, Saudi Arabia; and Maria-Angeliki Gkini, Consultant Dermatologist at Barts Health NHS Trust, London, UK, can help the dermatology community to better understand the value of achieving MDA, paving the way to advancing the standard of care in atopic dermatitis.
THE BURDEN OF DISEASE AND UNMET NEEDS IN ATOPIC DERMATITIS
AD is a common, chronic inflammatory skin disease with a significant impact on patients’ lives.1 As a heterogeneous disease, AD has substantial variability in pathogenesis and clinical presentation. Gkini noted that AD reflects “a systemic condition rather than a skin condition.” In addition to skin lesions, itch is a commonly reported symptom that can have many psychosocial consequences. Both Binamer and Gkini agreed that pruritus, or itch, is the most commonly reported and most burdensome symptom for patients with AD.
Gkini further noted that “pruritus can be really debilitating. Patients are itchy, scratching, which can affect all aspects of their daily life and mental and general well-being. They are not able to sleep, they are not able to go to work, they are not able to go to school, they are not able to function.” In a global patient research survey carried out to evaluate the burden of AD, over 75% of patients reported itch, skin redness, dry/flaky skin, and sleep disturbance every 1–3 days, with more than half reporting mental health issues at least 2–3 times a month.1 These impacts can persist despite treatment, with 56% of patients still reporting sub-optimally controlled disease.2 In patients treated with systemic therapy, the burden of AD can extend beyond the physical signs and symptoms, including sleep disturbances multiple nights per week, frequent flares, multiple healthcare appointments, and impairment of work productivity and activity. Those impacts worsen with increasing disease severity levels,3 and may accumulate over the life course of a patient living with AD.4 Binamer explained: “Some of our patients with very frequent flares have work absences, for example, every 2 weeks, as they are spending time travelling to appointments, refilling prescriptions, going to the emergency room, and completing many assessments.” Therefore, if patients are sub-optimally controlled, even those treated with systemic therapy can continue experiencing significant challenges to their quality of life.4,5 Given the broad impact of AD, patients favour using a combination of patient-reported and clinician-reported outcomes to reflect the total burden of their disease.5 AD management should be individualised, incorporating patient needs in a shared decision-making approach.
THE AIMING HIGH IN ECZEMA/ATOPIC DERMATITIS APPROACH: AIMING FOR MINIMAL DISEASE ACTIVITY
The AHEAD consensus-based recommendations outline a novel approach to AD management that combines shared decision making with a treat-to-target approach.6 Prior to the establishment of the AHEAD recommendations, international experts had identified a lack of evidence on patients’ treatment goals, needs, and expectations in AD management. As a result, the experts conducted a qualitative patient research survey, which provided robust evidence for the creation of the AHEAD recommendations and supported a patient-centric approach to AD management.1,6
The AHEAD recommendations established MDA as a preferred treatment goal in AD. Simultaneous achievement of optimal targets on a PRO and a ClinRO constitutes achievement of MDA (Figure 1 and Table 1).6 An increasing number of national guidelines and consensus statements have since adopted MDA as a recommended treatment goal, including those from China, Argentina, Czechia, and the United Arab Emirates.7-10
Figure 1: Achievement of minimal disease activity in atopic dermatitis.
Created in biorender.com.
ClinRO: clinician-reported outcome; MDA: minimal disease activity; PRO: patient-reported outcome.
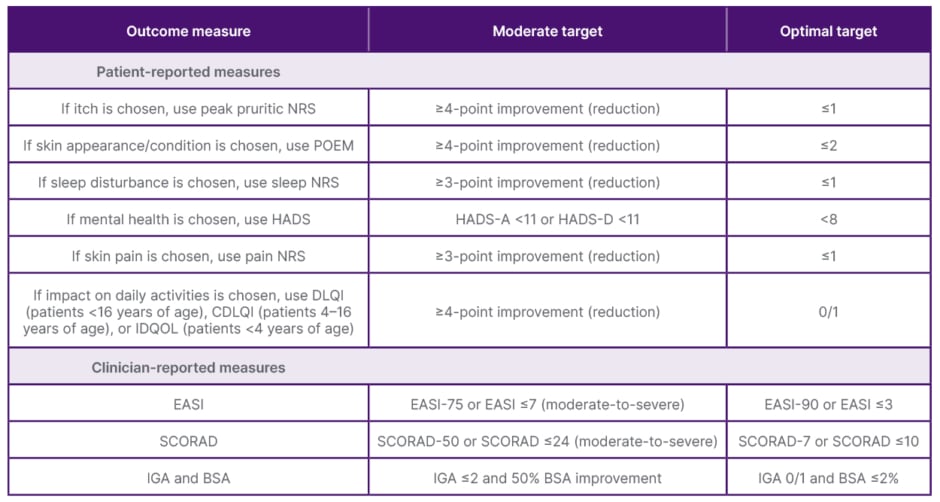
Table 1: Recommended treatment targets for patient-reported and clinician-reported measures.*6
*Targets are for all AD severities, unless otherwise specified. Both ‘moderate’ and higher ‘optimal’ targets were developed to reflect that optimal targets may not be currently achievable in all patients and all parts of the world due to availability and access to advanced treatment options. Achievement of ‘optimal’ targets is defined as MDA.
Adapted from Silverberg et al.6
AD: atopic dermatitis; BSA: body surface area; CDLQI: Children’s DLQI; DLQI: Dermatology Life Quality Index; EASI: Eczema Area and Severity Index; EASI-75/90: 75%/90% improvement in EASI; HADS: Hospital Anxiety and Depression Scale; HADS-A: HADS-Anxiety; HADS-D: HADS-Depression; IDQOL: Infants’ Dermatitis Quality of Life; IGA: Investigator’s Global Assessment; MDA: minimal disease activity; NRS: Numeric Rating Scale; POEM: Patient-Oriented Eczema Measure; SCORAD: SCORing Atopic Dermatitis.
Gkini added that STRIVE-AD, a modified Delphi consensus conducted in the UK, is pending publication, and also serves as a practical recommendations guide on optimising the management of patients with moderate to severe AD. It will focus on five key areas, including a patient-centric approach and aiming for control of the disease with a percentage of patients achieving MDA.
MDA reflects the burden of AD through the lenses of the patient and the physician, enabling a holistic approach to AD management.6 Gkini emphasised that “it’s really important to understand what patients experience, how they feel, what their key concerns are, so as to be able to address them.”
Gkini and Binamer strongly emphasised the importance of shared decision-making with patients. “By discussing which goals they want to achieve, and how we can set up their treatment to achieve them, we try and reach optimal outcomes,” said Binamer. He continued, explaining: “However, if we are not achieving these goals, we need to either modify the management plan or look again and discuss with our patient.” Per the AHEAD recommendations, treatment modification or escalation should be considered if treatment targets are not met within 3–6 months.6 Gkini explained that by using the AHEAD and STRIVE-AD recommendations, rather than just managing symptoms as and when they arise, clinicians and patients can work towards clearly defining specific treatment goals, short-term and long-term, and optimise treatment when goals are not achieved.
WHAT DOES ACHIEVING OPTIMAL TREATMENT TARGETS AND MINIMAL DISEASE ACTIVITY MEAN FOR PATIENTS?
Recently published data indicate that achieving MDA is associated with the greatest levels of improvement in health-related quality of life (HRQoL) compared to not achieving MDA.11 In a post-hoc analysis of the Measure Up 1, Measure Up 2, and AD Up Phase III trials, patients randomised to AD treatment or placebo were pooled and stratified into three mutually exclusive response groups meeting optimal, moderate, or neither treatment target for each ClinRO or PRO, and those achieving MDA at Week 16.11 The reported impact on HRQoL was measured across eight domains: itch, other skin symptoms, quality of life, sleep, daily activities, emotional state, work productivity, and treatment satisfaction. The AHEAD recommendations indicate that the primary treatment goal in AD management should be a satisfied patient with a high quality of life, clear or almost clear skin, and a minimal degree of itching.
Across all measures, a higher proportion of patients who achieved optimal treatment targets were able to attain stringent patient HRQoL outcomes, compared to those meeting moderate or neither treatment target. In addition, patients who achieved MDA were more likely to attain stringent HRQoL outcomes, versus those who did not achieve MDA. This means that patients who achieved MDA experienced little to no impact of AD on sleep disturbance, daily activities, emotional state, and overall quality of life, among other quality of life measures.11 Specifically, patients who achieved MDA by simultaneously achieving optimal treatment targets of clear or almost clear skin and a minimal degree of itching (i.e., 90% improvement in Eczema Area and Severity Index [EASI-90] and Worst Pruritis Numerical Rating Scale [WP-NRS] 0/1) were five-times more likely to experience little to no impact of AD on sleep and on daily activities, compared to those who did not achieve this definition of MDA. Furthermore, nearly 73% of these patients were also able to achieve little to no impact on their quality of life (i.e., DLQI 0/1), compared to approximately 4% of patients who did not simultaneously achieve EASI-90 and WP-NRS 0/1 (Figure 2).
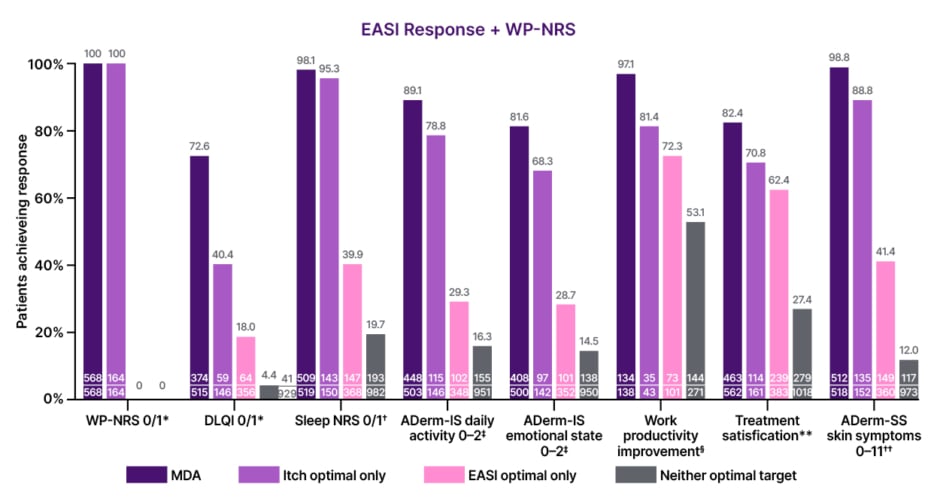
Figure 2: Effect of achievement of minimal disease activity, patient-reported outcome optimal only, clinician-reported outcome optimal only, and neither optimal targets on patient health-related quality of life outcomes by Eczema Area and Severity Index and itch.
Analyses were based on available data for each outcome. Sample size may vary depending on data availability
of the measures involved.
*For patients with baseline score >1.
†ADerm-IS item no. 2 sleep 0/1 among those with baseline score >1.
‡Among those with a baseline score >2.
§WPAI overall work impairment ≥20-point improvement among those with a baseline score ≥20.
**Patient Global Impression of Treatment reporting “extremely satisfied” or “very satisfied.”
††Among those with baseline score >11.
Adapted from Silverberg et al.11
ADerm-IS: Atopic Dermatitis Impact Scale; ADerm-SS: Atopic Dermatitis Symptom Scale; DLQI: Dermatology Life Quality Index; EASI: Eczema Area and Severity Index; MDA: minimal disease activity; NRS: Numerical Rating Scale; WP-NRS: Worst Pruritus Numerical Rating Scale.
Regarding these results, Binamer explained: “The difference is clear between a patient who has achieved MDA and one that has not. Achieving MDA means improvement in quality of life, productivity, and psychosocial impact.”
Gkini highlighted the real-world impact of achieving MDA from the patient perspective: “[Achieving MDA] can really transform patients’ lives. Why? Before achieving their goals, imagine someone who is constantly itchy and who is not able to sleep. They are not able to function, they’re not able to study or work. It can affect their relationship with friends, family or partners. It is not only the quality of life. It is the mental health, many patients become depressed, anxious or suicidal because of their condition. Therefore, managing it effectively can be life-transformative. Binamer added: “Many of our patients with AD are young…teenagers or in their early 20s, so they have lots of activities, busy social lives, daily activities… so achieving optimal goals, MDA, such as no more itch, is major for our patients.”
Moreover, Binamer reflected on how the achievement of treatment goals, such as MDA, not only impacts patients but also everyone around them. “It does not affect the patient only; it affects their parents, the household, and their work environment. Beyond the numbers and the tests, there is a real-world impact.”
Gkini noted that not all patients with AD may be able to achieve MDA, but it should be seen as an optimal goal, in alignment with the AHEAD recommendations.6,11 These data demonstrate that patients who achieve MDA experience optimal quality of life improvements across multiple dimensions of their lives, thereby underscoring the importance of aiming for higher treatment targets when treating patients with AD.11
WHAT DOES ACHIEVING OPTIMAL TREATMENT TARGETS AND MINIMAL DISEASE ACTIVITY MEAN FOR PHYSICIANS?
Gkini and Binamer also discussed a post-hoc analysis of the real-world MEASURE-AD study, recently presented at the American Academy of Dermatology (AAD) 2025 Annual Meeting, which examined the association between achieving MDA with flare occurrence and healthcare utilisation in patients with AD.12 Of the 1,434 patients included in the analysis, 20% had received systemic therapy continuously over the past 12 months. The number of flares, duration of flares, and number of healthcare visits in the preceding 6 months were assessed in patients who had achieved MDA versus those who had not achieved MDA. A questionnaire was used to assess whether patients thought their AD was being adequately controlled. Patients who achieved MDA reported fewer flares with shorter duration, compared to those who did not achieve MDA. Patients who achieved MDA also reported fewer AD-related healthcare visits and were more likely to agree that their AD was well controlled.12 Reflecting from a physician’s perspective, Gkini added: “Generally, in medical dermatology, we want our patients to be well controlled so that there is no need for frequent visits in the clinic.” Binamer elaborated that a high number of flares and subsequent use of healthcare services result in a significant burden on already-strained clinics. He continued to explain that patients with controlled disease have fewer appointments, resulting in lower utilisation of healthcare services. He emphasised that less time spent with doctors means patients can spend more time living their lives.
He also explained that patients who achieve MDA will spend less time attending the clinic, which eases pressure on busy healthcare professionals and saves money in the longer term, both for the patients themselves and the practice as a whole. Moreover, Binamer emphasised the importance of sharing a rescue plan with patients, explaining what they should do in case of flares if they are unable to see a physician, thereby freeing up time in the clinic for newly presenting patients.
HOW DO CLINICIANS IMPLEMENT THE AIMING HIGH IN ECZEMA/ATOPIC DERMATITIS APPROACH AND MINIMAL DISEASE ACTIVITY IN REAL-WORLD CLINICAL PRACTICE?
Gkini and Binamer agreed that the AHEAD approach and aiming for MDA have helped shape their approach to AD management. As clinics are often busy, utilising the AHEAD approach helps to streamline appointments and ensure that every minute spent with the patient is as useful as possible.
Binamer highlighted that a crucial moment in patient management is the first time a patient attends a dermatology clinic. He recommends that healthcare professionals grasp this opportunity: “Give the patient your time in the first few visits, and this will make subsequent visits shorter as you have taken that time to lay out a management plan.” In his clinical practice, Binamer explained: “We always ask the patient, ‘What is most bothersome of your symptoms?’ We want this from the perspective of the patient, and then from the perspective of the clinician.” Both Gkini and Binamer use EASI scores when assessing patients, and suggest that within the clinic, physicians retain familiarity with a specific assessment tool, which can be EASI, ScORing Atopic Dermatitis (SCORAD), or Investigator Global Assessment (IGA) and Body Surface Area (BSA), using it across the entire patient follow-up period.
Binamer recommended a step-by-step approach to management. With the overarching goal of MDA, for example, he suggests beginning with aiming for moderate targets. If moderate targets are achieved, then he recommends stepping up to optimal targets. If moderate targets are not achieved within 3–6 months, however, physicians can discuss this outcome with the patient and consider treatment modification or escalation. “My advice for physicians is that if the patient is not responding to treatment, speak to them about what they want to achieve, and evaluate what they did not achieve,” Binamer said.
Gkini elaborated that it is crucial for treating physicians to inform patients about their available options and the potential that they have to achieve clear or almost clear skin. Often, patients present in clinic with severe disease, but they report being happy, and are reluctant to change treatment, since they were much worse before. “It is our responsibility to provide all the relevant information and raise awareness so patients can make informed decisions.” She added that, in the UK, patients are assessed 16 weeks after receiving treatment. If they have fulfilled their goals, patients continue treatment. If they do not, physicians consider treatment optimisation, which can be adding other agents or switching to another treatment, and discuss this with the patient.
Binamer acknowledged that some physicians may be reluctant to adopt the AHEAD approach, perceiving it as time-consuming. However, he emphasised that the structured approach facilitates clinical efficiency. By identifying the patient’s most burdensome symptom and setting goals with them, clinicians can use continual evaluation for consistent monitoring of patient response to treatment. “This is not a 100-metre sprint, it’s a marathon, and we are running this marathon along with our patients,” said Gkini.
WHAT DOES THE FUTURE HOLD FOR PATIENTS WITH ATOPIC DERMATITIS?
Binamer and Gkini reflected on the dramatic evolution that the AD therapeutic landscape has undergone in recent years. Binamer highlighted that only a decade ago, the clinical benchmark for success was a 50% improvement in disease severity. Today, therapeutic goals have advanced substantially, with targets such as EASI-90 considered realistic in many patients.
With MDA recognised as an attainable and clinically meaningful treatment goal for certain patients, dialogue between patients and physicians around outcomes continues to evolve. Once limited to discussions of partial symptom control, treatment discussions can now focus on eliminating itch alongside clearing skin and improving HRQoL. The latest evidence from Silverberg et al.11 emphasises this shift, demonstrating that those achieving MDA experience the greatest improvements in HRQoL across multiple domains. Supported by the growing availability of targeted systemic therapies, MDA is now a realistic outcome for patients with AD. These changes mirror the progress observed in psoriasis management, Binamer remarked.
To conclude, Binamer underscored three key principles for future practice. Firstly, to avoid “holding treatments hostage,” and recognise the available options for treatment for moderate-to-severe AD. Secondly, if a patient is unresponsive to topical therapy, act promptly, as timely consideration of systemic therapies is crucial. Finally, to seek appropriate experience. If physicians are uncertain in managing AD, they should seek out those who have experience and can guide them.
Overall, with timely intervention, modern therapies, and tailored and individualised treatment goals, the future for patients with AD and those managing it looks to be promising.






