BACKGROUND AND AIMS
Cutaneous leiomyosarcoma is a rare smooth muscle neoplasm that can be classified as dermal or subcutaneous depending on the depth of origin. Dermal leiomyosarcoma (dLMS) is generally considered an intermediate-risk neoplasm characterised by a considerable risk of local recurrence but a low risk of metastasis. Although there is general agreement that dLMS presents a low risk of metastasis, the possibility of metastatic potential cannot be dismissed entirely, as reported metastasis rates in the literature vary from 0–14%.1-7 Furthermore, risk factors for dLMS remain poorly defined because methodological constraints, small sample sizes, and short follow-up have limited previous studies. The objective of this study was to investigate risk factors for metastasis and local recurrence, and to propose a high- and low-risk classification for dLMS.8
MATERIALS AND METHODS
The data were extracted from the Danish National Health Registers. These registers, as well as individual-level linkage of data across all registers, have been described previously.9 All patients diagnosed with dLMS in Denmark between 1980–2022 were included. All tumours were diagnosed following WHO guidelines for sarcomas, and treated at specialised sarcoma centres in accordance with the Danish national guidelines.¹⁰ Absolute 5-year risks were estimated with the Aalen–Johansen method, treating all-cause mortality as a competing risk. The results were presented as 5-year absolute risks and risk differences (RD) with 95% CIs. The classification of dLMS into high- and low-risk groups was based on risk factors associated with a 5-year RD of >5% for metastasis and >10% for local recurrence based on the overall 5-year risks for each outcome.
RESULTS
Among 381 patients (median age: 66 years; 71% male), the 5-year risks of metastasis and local recurrence were 2.4% and 10.0%, respectively (Figure 1).
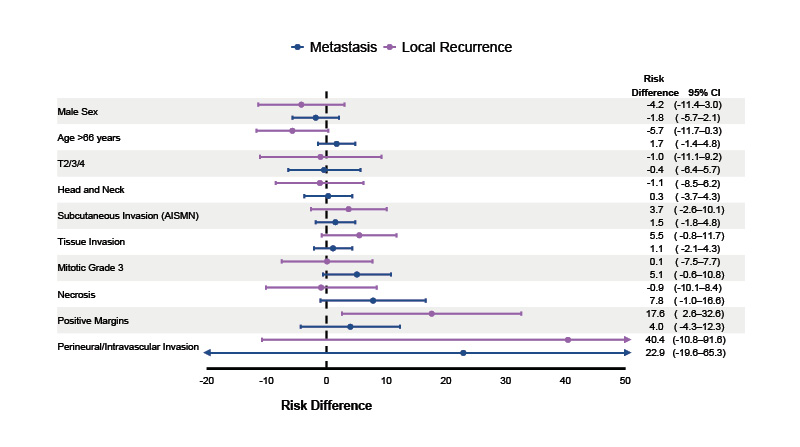
Figure 1: Forest plot of the univariable analysis of risk factors for metastasis and local recurrence.
AISMN: atypical intradermal smooth muscle neoplasms.
The presence of tumour necrosis was associated with a 5-year metastasis risk of 9.3% (95% CI: 0.6–18.0) compared to 1.5% (95% CI: 0.2–2.8) in those without tumour necrosis (RD: 7.8%; 95% CI: –1–17). Patients with mitotic Grade 3 had a 5-year metastasis risk of 6.5% (95% CI: 1–12) compared to 1.4% (95% CI: 0–2.8) for Grades 1 and 2 (RD: 5.1%; 95% CI: –0.6–11.0). Perineural or intravascular invasion was linked to a 25.0% (95% CI: 0–67) risk of metastasis compared to 2.1% (95% CI: 0.7–3.6) in patients without invasion (RD: 23%; 95% CI: –20–65).
For local recurrence, positive surgical margins were associated with a 5-year risk of 26.0% (95% CI: 11–41) compared to 8.4% (95% CI: 5.5–11.0) in patients with negative margins (RD: 18%; 95% CI: 3–33). Perineural or intravascular invasion was associated with a 50.0% (95% CI: 0–100) risk of local recurrence compared to 9.6% (95% CI: 6.6–13.0) in patients without invasion (RD: 40%; 95% CI: –11–92).
CONCLUSION
The authors propose that high-risk dLMS could be defined by the presence of necrosis, mitotic Grade 3, perineural/intravascular invasion, or positive surgical margins. The authors suggest that all patients with dLMS could have clinical visits twice in the first year, followed by annual visits for 3 years, as no further relapses occurred after this time point (4 years). The follow-up of patients with high-risk dLMS could be extended to also include either PET/CT or CT of the chest in the first 2 years due to the risk of distant and pulmonary metastases. The follow-up of patients with low-risk dLMS could be limited to annual examinations with a general practitioner or dermatologist.






