Latex allergy is a common occupational disease among healthcare workers who use latex gloves.1-3 Diagnosis of latex allergy is determined by analysis of personal history, physical examination, skin prick, patch, and challenge tests, or specific IgE determination, while self-administrated questionnaires are used to assess data about natural history, risk factors, etc.4-7 The main aim of this study was to determine the prevalence of allergy to latex gloves among dental students and the role of exposure duration in latex allergy.
In this prospective study, a total of 240 students completed a self-administered questionnaire providing information about gloves, working habits, signs and symptoms related to glove use, precautions taken to minimise it, etc. The students were separated as non-exposed, shortly-exposed, and longer-exposed to natural rubber gloves during school practice. The challenge and patch tests were performed through latex gloves, and the skin prick test for latex, pneumoallergens, and trophoallergens with commercial extracts.
The questionnaire items and diagnostic tests revealed that one-quarter of the participants were suspicious of latex glove hypersensitivity. Their mean value for skin reactions, such as contact urticaria, irritant, or allergic dermatitis, was between 10% and 14%, while for non-cutaneous symptoms the mean value was <5% (Table 1). The average latex exposure was estimated to be ~214±71 hours (SE), with a maximum of 11,500 hours. The correlation between studied variables and the time exposure to latex gloves revealed weak-to-moderate relations with respect to reported latex allergy, eczematous reactions, hand erythema after glove wearing, irritant reactions during wash/ washout procedures, recent concentration problems during usage of latex gloves, or dyspnoea attack during latex exposure (Table 2). In general, the students who experienced latex exposure for >2 years during their school practice have shown a two-fold positive response for statements or diagnostic tests on latex gloves hypersensitivity (Table 1). Additionally, the Kendall’s tau coefficient progressed from the non-exposed group to the longer-exposed group for the majority of items. Logistic regression analysis revealed an association between different questionnaire items and positive allergy tests among suspected and diagnosed cases of latex allergy, but not with control tests, including between the positive patch test and presence of non-cutaneous symptoms. Sensitisation to aeroallergens and trophoallergens was shown in 38% and 12% of subjects, respectively.
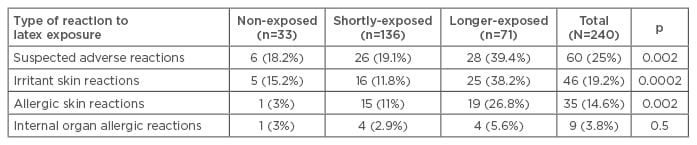
Table 1: Reactions to latex exposure.
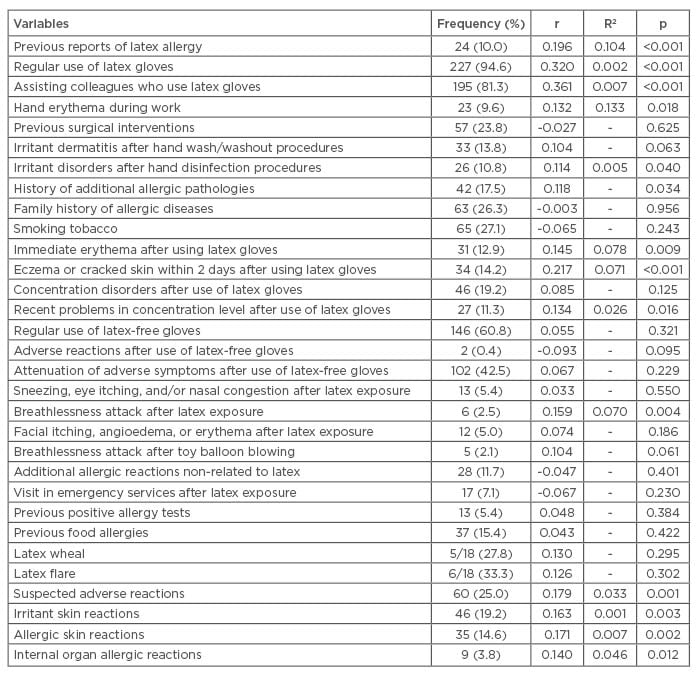
Table 2: Correlation between latex exposure duration and other study variables.
This study reinforces the notion that it is essential to recognise which professionals are sensitive to latex in order to provide appropriate treatment and to establish adequate prevention.3 Due to the relationship between allergic reactions to latex gloves and some medical histories during school practice, it is necessary to undergo pre- matriculation evaluation and periodic health surveillance of dental students.8 A positive history of allergic and irritant symptoms, determined by a questionnaire, was a significant predictor of a positive response to latex antigens.5 This, in combination with positive diagnostic tests, confirms suspected latex allergy, especially when pathology is already established. This study also demonstrated that latex allergy patients are more predisposed to be sensitised to aeroallergens and trophoallergens compared to the general population. This predisposition can be considered an important risk factor for the development of food allergy and respiratory allergic diseases.3,7 Moreover, our findings suggested that respiratory exposure plays an important role in the interaction between different mechanisms during sensitisation processes, and that questionnaire statements about latex allergy in combination with positive diagnostic tests can be reliable in the identification of allergic subjects.9,10






