I have been asked to share my opinion about the diagnostics of anaphylaxis and how to treat it. As you probably know, anaphylaxis is the extreme outing of an allergic reaction and is likely if any one of three criteria is fulfilled (Figure 1).1 Assessing anaphylaxis is hard to do because you must first assess or establish the eliciting condition. The European Academy of Allergy and Clinical Immunology (EAACI) has produced guidelines for allergic conditions to help clinicians establish the correct diagnosis and treatment for that condition.2 Although anaphylaxis may occur with different allergic conditions, one of the major eliciting factors for anaphylaxis is food, and food has been the main immunoglobulin (Ig)E-mediated cause for anaphylaxis hospitalisation in recent years.1,3 These guidelines are instrumental in the education of anyone dealing with patients at risk of anaphylaxis.
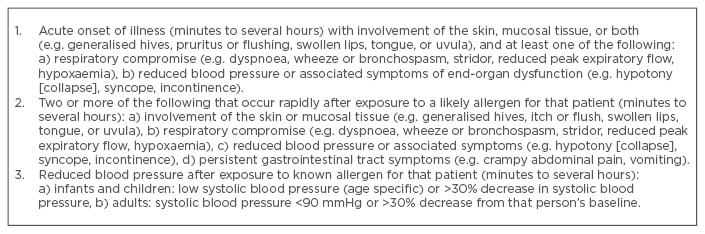
Figure 1: Criteria for an anaphylaxis reaction recognition.
Adapted from Sampson et al.1
It might be hard to diagnose patients with an allergic condition that may have the potential of anaphylaxis, and it all starts with the medical history. Listening to the patient telling their story about the reason why they are consulting their
family doctor, you need to know what to ask and how to interpret the answers; I know that is not an easy task. Then, when you have concluded that it could be an allergic condition that is causing your patient’s complaints, you might decide that you need to perform some additional analytical tests. Therefore, you tell him or her that you want some allergy tests performed, and it is here that misunderstandings may begin. The term ‘allergy test’, in this situation, is inaccurate and might set the patient on the wrong foot. The tests you are considering performing are tests which indicate the presence of antibodies to certain allergens, and, simply said, the result can be positive or negative. The absence of antibodies will “indicate that the patient does not have an allergy, but the presence of antibodies does not indicate an allergy, only sensitisation!”4 But just telling the patient that the result, as such, of the ‘allergy test’ (for a specific allergen) is positive might let the patient believe that he or she is allergic to that allergen, and that might not always be true.5,6 Therefore, I would stress banning the term ‘allergy test’ and calling it as it is.
The outcome of these tests is only valid in the diagnosis of the condition in relation to the medical history, and should be tests to confirm or disprove your suspicion. If you are not sure or in doubt, the only true means of telling whether a patient with a suspected food allergy truly has a food allergy is the use of oral food challenge under strict supervision, which is currently seen as the gold standard.7
How does this help us in assessing the diagnosis of the risk of anaphylaxis? That is difficult to say. The outlined procedure will help us in assessing whether a patient does have a food allergy but says nothing about the risk of anaphylaxis. So, how can we assess if an allergic patient is at risk of anaphylaxis? One way (and please note that it would be ethically questionable), is to perform an oral challenge, but then not to stop at the first signs or symptoms, but to proceed until the patient shows severe symptoms. The question is, do we want to go that way? What is the advantage or disadvantage for the patient? Does the outcome of this single test predict future outcomes? So, I ask the reader, can we genuinely advise the patient that he or she is at risk of anaphylaxis? In practice nowadays, we encounter a definite diagnosis of a true food allergy based on a severe allergic reaction or anaphylaxis in the medical history, and the concluded advice is that the patient is also at risk of anaphylaxis in the future. If the patient is lucky, they will get an adrenaline auto-injector prescribed, for the first aid treatment should an anaphylaxis occur, and advice to then call an ambulance. If the patient is lucky, they will also be educated in when and how to administer an adrenaline auto-injector and is instructed on how to avoid the eliciting allergen.
Unfortunately, it all comes down to luck. I know I am generalising, but the fact is that allergists in many countries are too few and only a few medical specialists are also experienced in allergy and anaphylaxis. Recently it was shown that “the primary care doctors expressed self-declared gaps in knowledge in most manifestations of allergy with a correspondingly high self-expressed educational need.”4 This realisation makes me both anxious and glad, as these doctors are the first in line to help the growing number of people with allergies; it makes me anxious because it shows that the knowledge of allergies is lacking and glad that they are willing to educate themselves. We know that knowledge is lacking in the majority of medically educated health professionals. Did you know that, for instance, in the Netherlands medical students in their 6-year education to be a basic doctor only get an average of 16–24 hours’ education on allergy! So, allergy, although a rising societal medical problem (some even say it is the 21st century epidemic), is hardly the focus of education policy makers!
But even after the basic medical education, students need to specialise themselves in an area of medical interest, and what do we see? The specialities focus mainly on organ systems, like internal medicine, otorhinolaryngology, dermatology, gastroenterology, respiratory medicine, cardiology, etc. Allergy is, in many countries, a subspeciality and first you should complete a primary speciality. Due to the length of medical education the decision to also choose an allergy subspecialty is only taken by the totally committed.
Another problem is that allergy is a ‘holistic’ condition; by this I mean that the symptoms that arise from an allergic reaction may appear in different organ systems, sometimes simultaneously, and are thus not restricted to one organ system. The only other ‘holistic approach’ speciality is paediatrics. We still have a long way to go and hopefully the education of policy makers will enable them to realise that allergy should have a prominent place in the medical curriculum.
There is a growing interest in allergy research. Researchers are considering the mechanisms of the immune system and try to find out the basics of the allergy mechanism. They have succeeded greatly in disclosing which different cells play a role in that mechanism. But why someone is sensitised and someone else not, given the same circumstances and conditions, has still not been explained. In my opinion, for these disclosures to happen it may still take a long time. I was told, when my child had an anaphylaxis in 1994, that it would probably take some 10–15 years before a cure would be available, and, although research has progressed a lot since, 23 years later there still is no cure. I do admit, at this moment there seems to be a positive effect due to food allergen immunotherapy, but that is still in an experimental stage and not in daily clinical practice.8 We must continue on this path, as people at risk of anaphylaxis are looking out for these kinds of therapies because living with allergies and the risk of anaphylaxis reduces their quality of life immensely. Policy makers should allocate public funds for clinical and societal research and not have the impression that the problem is not so great because only a limited number of fatalities occurred compared to other conditions or diseases. Focussing only on fatalities does not reflect the impact of the problem. They should consider the hospitalisations and reduction in quality of life.
What is, then, my message to the world? Until there is a cure, education is key. Education not only for the medical professional on how to guide and educate their allergic patients, but also for parents and the patients themselves on how to deal with this condition and the risk of anaphylaxis. This will raise their quality of life through the knowledge that their condition is manageable and they can take control. They need to know that, in general, the risk of anaphylaxis is due to the eliciting allergen entering their body, they need to know what they react to, and what the allergens are that might cause anaphylaxis. The parents need to know the assessed real risk and not the perceived risk, as the perceived risk may become the projected anxiety in the allergic child, thus developing an anxiety disorder.9
Education in the manageability of their allergy requires the correct information provision and the skill to communicate it to the social environment. This will allow the allergic individual to fully participate in society, with some restrictions, but no limitations.






