Meeting Summary
Hereditary angioedema (HAE) attacks are unpredictable and can be debilitating and potentially life-threatening. The burden of HAE disease and its treatment can negatively impact individuals’ quality of life (QoL). A group of internationally recognised HAE experts convened for a sponsored symposium, which took place on 14th June 2025 as part of the European Academy of Allergy & Clinical Immunology (EAACI) Congress held in Glasgow, UK, to discuss gaps in HAE management. They discussed how, despite evidence-based treatment guidelines that make recommendations for all HAE patients to carry on-demand treatment at all times, and that all attacks should be treated as early as possible, many patients do not carry medication or treat attacks early. The panel and audience heard HAE patient perspectives through video clips and survey responses and discussed how patient and physician perspectives differ in terms of disease control and management. The wide-ranging discussions between panel members highlighted some of the barriers that patients face when it comes to following treatment guidelines for on-demand treatment of HAE attacks and offered perspectives on what more needs to be done to overcome these hurdles to allow patients with HAE to be more in control of their disease.
Introduction
Hereditary angioedema (HAE) is a rare genetic condition characterised by unpredictable episodes of cutaneous or submucosal swelling in different parts of the body, which can be life-threatening when affecting the upper respiratory tract.1 The condition can have significant negative impacts on patient quality of life (QoL). Attacks are often debilitating and can result in work or school absences and may require hospital stays.1 In addition, the unpredictable nature of attacks means that patients may adapt their lifestyle to avoid triggers, even avoiding some ‘normal’ activities.2 The treatment burden of having to self-administer parenteral medication or attend hospital to receive treatment leads to delayed or missed treatment of HAE attacks and a prolonged attack duration, and can also negatively impact QoL.1
Despite published international guidelines3 that recommend all patients always carry enough on-demand medication to treat at least two HAE attacks, many patients fail to carry their medication and often delay treatment. This can lead to exacerbation of symptoms and have further negative impacts on QoL. Early treatment is associated with a shorter time to symptom resolution and shorter total attack duration, regardless of attack severity.4 Indeed, treatment guidelines recommend that all HAE attacks are considered for on-demand treatment and that treatment starts as early as possible after the initiation of the attack.3
In this sponsored symposium, an HAE expert panel chaired by Doug Jones, Global Allergy Immune Network, USA; and including Stephen Betschel, Unity Heath, Toronto, Canada; Thomas Buttgereit, Institute of Allergology, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität Zu Berlin, Germany; and Sinisa Savic, University of Leeds, UK, discussed the gaps that exist in HAE management between patient and physician perspectives of disease control. They also identified some of the barriers that patients face when it comes to following treatment guidelines for on-demand treatment of HAE attacks, and asked what more needs to be done to overcome these hurdles to allow patients with HAE to be more in control of their disease.
Treatment Burden and HAE Control
Jones opened the symposium with a stark reminder that HAE attacks can cause significant anxiety, describing a case where he was called by police to sign a death certificate for a patient with HAE who had potentially failed to access or take on-demand medication. Jones went on to ask the audience whether, in their experience, more than 50% of their patients are in control of their disease. Most participants voted no.
To provide direct insights from patients, the audience was shown video clips from three individuals with HAE who described the challenges they face day-to-day to stay in control of their HAE. Laura, one of the patients, who was diagnosed with HAE at age 15 years, said: “[It’s] always on your mind because you know the potential for how bad it (HAE) can be and how dangerous it can be.” They went on to explain that having on-demand treatment means it is easy to treat an attack without needing to find a hospital. “You have the flexibility of essentially being able to live your life because you can treat wherever you are.” However, Laura continued by explaining that depending on where they are, they have a concern about whether they will be able to find a sterile environment to administer their intravenous medication. Chip, another patient with HAE, is 34 years old, and their partner is expecting a baby. Chip does not take LTP but does treat attacks with on-demand treatment. On a recent trip to the USA, Chip experienced an HAE attack and the only place available to inject the on-demand treatment was in a toilet. “It was not very hygienic,” Chip said, and went on to explain that if you administer medication in a public space, people can get concerned and think you are injecting recreational drugs.
Jones highlighted that there is a worldwide consensus on best practice for treatment with on-demand medication for HAE attacks. International guidelines3 state that all patients should carry sufficient on-demand medication to treat at least two attacks, that all attacks should be considered for treatment, and all attacks should be treated as early as possible.3 Jones emphasised that the consensus is that the goal should be for patients to experience no HAE attacks, but they asked: “How realistic is it for HAE patients to achieve no angioedema attacks?” Approximately 50% of people with HAE are not completely attack-free despite taking first-line LTPs.5 In addition, many people, including those who take LTP, face ongoing anxiety regarding the unpredictability of attacks and when anticipating taking current on-demand therapies.6,7 Jones added that on-demand therapy for HAE remains a critical need, even for patients receiving LTP.
Jones opened up the discussion to the panel by asking: “Are patients achieving control of their HAE attacks?” Betschel responded first, highlighting that the guidelines state that patients should be able to achieve total control and normalise their lives.3 This suggests that total control means a complete absence of attacks, Betschel said. However, they do not believe this to be the case, but rather an aspiration. “We know that many people don’t have that total control, and that is the gap we are trying to close.” Betschel added: “How do people who still have attacks maintain control of their disease?”
Savic expanded the discussion, saying: “With HAE, it is not just a physical condition. There is a psychological component to the disease.” The worry and anxiety of having an attack can be significant and varies between patients. “We haven’t explored these [psychological] aspects of the disease fully yet.” For Buttgereit, it is important to be able to distinguish between having control of the disease and having control of attacks. “Does total control mean that you do not have to go to the emergency room to get an injection or infusion, or you don’t need to stay overnight in hospital? Or does it mean doing the things you want to do, to participate in all aspects of life, work, school, without limitations?”
Jones then presented a slide with quotes from patients illustrating that individual patients define control differently and this differs from how physicians might define control. “It is important for us as clinicians and experts to communicate with our patients and understand their perspective, understand their challenges, and align them with our treatment approach and with the guidelines,” Jones emphasised, inviting the panel to choose a patient comment that resonated with them.
Betschel picked out a patient comment that read, “I start to feel the attack resolving, at least somewhat, and I am able to resume normal activities.” Jones responded: “I like this one, ‘The pain goes away, and my anxiety slows down.’ This says to me that the patient knows things are going to get better.” Buttgereit’s chosen comment was: “I know I’m in control when I feel the swelling or pain start to subside.” “This is key to treating attacks,” Buttgereit explained. “Patients could be in a life-threatening situation. Even if you just have a headache, you want to know when you will get symptom relief. You know the treatment works; you are confident you did the right thing; you are looking for the first sign that the treatment is working.” Sivac selected a quote that read: “I am able to get my medication started before my attack is bad.” “This is important,” Sivac continued. “Being able to use the treatment when you need it, having access to on-demand treatment and treating early, are all key.”
Benefits of Treating Attacks Early and the Barriers Patients Face
Patients who treat early feel in control sooner (Figure 1).8 “This is an ongoing theme,” explained Jones who outlined the results of a survey of 107 patients with HAE that demonstrated the mean time to feel in control of attacks after on-demand treatment was twice as long for those who waited 1 hour or longer, compared to those who waited less than an hour. 9
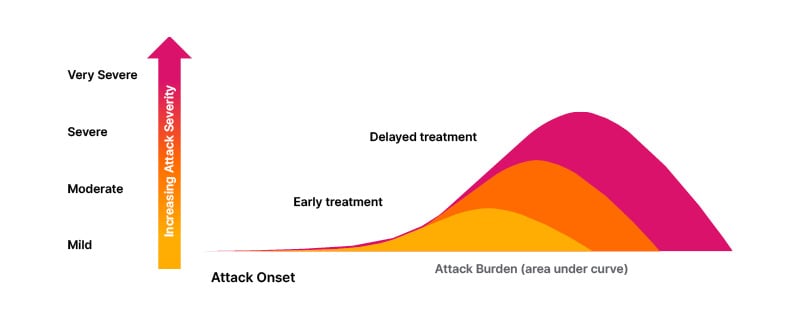
Figure 1: Patients who treat early feel in control sooner.
Adapted from Cohn et al.8
“So why are people waiting before taking on-demand medication?” Jones asked. “What is creating so much anxiety?” They outlined data from patient surveys that show almost two-thirds of patients don’t always carry on-demand medication with them.10 Moreover, 57% of patients don’t treat all their attacks.6 Patients waited an average of 3.8 hours before initiating treatment after the first signs of an attack.11 Jones went on to explain that a significant number of patients (44%) avoid triggers to prevent attacks from happening, despite being on LTP and having on-demand treatment available,2 with 48.6% of patients experiencing moderate-to-severe anxiety when anticipating on-demand treatment.12 “People are changing their lives, not just to avoid attacks, but to avoid triggers,” Jones added. There is consensus that patients are delaying on-demand treatment across healthcare systems and across geographies.13,14
Jones went on to ask the audience whether they thought most of their patients with HAE feel like they live a normal life. The majority voted no. The audience then heard short clips from patients with HAE, Camilla, Laura, and Chip. “It’s difficult because you are trying to be a normal functioning member of society while controlling an unpredictable disease. That is quite isolating because people, quite literally, cannot understand what it is like,” Camilla explained. Laura said: “I don’t think my normal will ever be the same as other people’s normal… It was a weird concept to me that other people had never been to A&E (accident and emergency, also known as the ER, or emergency room) or been in a hospital.” As part of Chip’s contribution, they said: “I don’t have total control, because I don’t have control over when I have attacks, but I do have control of managing them with my medication. It is not ideal, as I need to be more prepared to be ready to inject if I need to.”
Jones explained that people with HAE have a unique perception of how to normalise their lives and how to feel in control. Savic expanded on this, saying there are several very effective medications available that can, for some people, completely stop HAE attacks for long periods of time. “I spoke to one patient who said: ‘I feel really weird; you’ve taken my disease away completely.’” Savic explained that many people have grown up with HAE and the disease experience leaves a lasting imprint on their mind. “Treating attacks earlier and controlling the disease from an early age can reduce trauma and makes it easier for individuals to normalise their lives,” they reiterated. This was illustrated by one of the patient quotes presented to the audience: “Normalising my life is access to effective treatment, a good physician, and a good patient–physician relationship.” Savic challenged this perspective, saying, “There is too much ‘physician’ in there! They should not be relying on the relationship with the physician to have a normal life. That is the gap that we are trying to bridge.”
Jones summarised by saying that if you can make the disease course more predictable, then you feel more in control, and asked: “What can we do to help our patients to feel more in control?” Despite treatment guidelines that document the global consensus that patients should have access to effective medications and should treat attacks early with on-demand medication, globally, patients do not follow these guidelines. “Patients’ anxiety levels escalate until they decide to treat (Figure 2).15 This is the key gap that we have to close,” Jones said.

Figure 2: How do patients know they are in control of their attack after on-demand treatment?
Evolving the Discussion with Patients
“Should we re-examine the current definition of control and normalising patients’ lives?” Jones asked the panel. “Everyone has a different definition of normal life,” Buttgereit said, explaining that clinicians and patients have different perceptions of what is considered normal. In addition, the perception of what defines ‘early treatment’ by patients and physicians differs, Savic believes, saying: “We need to do more to understand what ‘early treatment’ means in our [professional] language and what it means in patients’ language,” adding that, “Surprisingly, some patients think that treating within a few hours of the start of an attack is early treatment.” Other panel members agreed. “Definitions are important, and physicians need to get onto the same page as patients,” Jones confirmed.
Betschel agreed and argued that: “We spend a lot of time collating evidence and publishing guidelines that recommend early treatment, but we are not doing a good enough job at communicating treatment recommendations.” Knowledge translation is key. “We have all this knowledge. So, what are we doing to facilitate change in practice?” Betschel asked. In the clinic, Betschel asks patients whether they have their medication with them, and if not, where it is. “I am learning what the barriers are and what factors are important to patients, so we can start to overcome them and try to reduce attacks on an individual patient level.” Buttgereit added that HCPs must listen to patients about the burden of treatment that they face, the availability of treatment, and whether they trust the treatment they take. Jones agreed, and expanded, saying that many patients have gone for up to 10 years without a diagnosis of HAE or have been misdiagnosed and treated with medications that have not worked. Therefore, physicians need to gain trust with these patients to individualise their treatment.
Referring to individualised treatment plans, Savic explained: “We need to accept that our definition of normalisation is not necessarily the same as the patients. Some people will tolerate a degree of attacks and discomfort. That is the landscape of their individual condition. But it is important to keep revisiting that question,” Savic added. “With trust in the treatment and trust in the relationship [with their physician], their goals may change.” It is also important, Buttgereit said, that on-demand treatment burden is considered as part of the normalisation of treating attacks. This burden is not normal for patients, nor for the community who may witness parenteral on-demand treatment administration. “The route of administration of on-demand medication plays a central role in the degree of normalisation.” Buttgereit reiterated. Betschel then asked, “What is getting in the way of trust and trusting the recommendations to treat early? What is getting in the way of using the treatment? Is it the drug itself, the cost, access? Are those barriers to trust? It is important to understand this.”
Summary
Jones summarised the session saying that patients are delaying treatment, but when they treat early, they feel more in control (Figure 3). Notably, perception of control is unique to individual patients. Anticipating on-demand treatment causes anxiety to patients, despite it helping them achieve a faster time to attack resolution, and this is an important factor for patients. The experts agree that more needs to be done to remove the barriers to treating HAE attacks early and reinforce that earlier treatment results in a faster time to feeling in control. “We have the data and the consensus guidelines, and we need to encourage more patients to adhere to them. We need to close gaps in trust, in access to treatment and reduce anxiety,” Jones concluded.
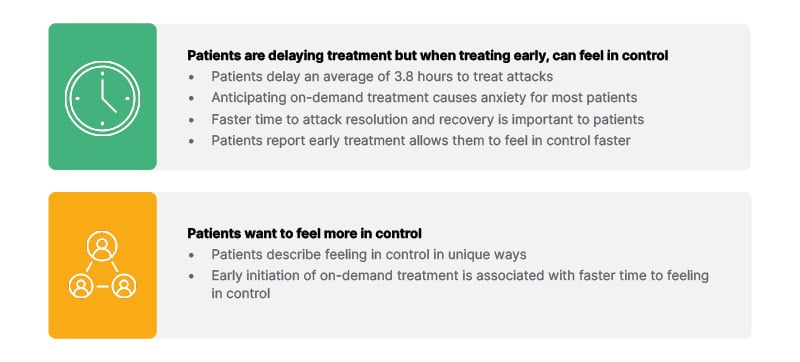
Figure 3: Summary.
Q&A Session
The Q&A session began with one audience member reiterating that whilst trust is important, we need to speak to the patients for their perspective on why they do not treat early. This is key and needs to be explored in depth. Betschel agreed and said physicians need to advocate early treatment and that means treating within an hour of the first symptoms. Savic added that patients are often part of cross-generational family groups who have different perceptions of control and health, and that should be optimised.
Another audience member then asked whether the panel members believe that prodromes should be treated. Betschel responded, saying that if patients have access to treatment, they should treat, although acknowledging there are varying degrees of access. “We have data that shows patients can predict attacks from prodromes, and that needs to be acknowledged and discussed.” Buttgereit added, “We need to recognise what the first symptoms of an attack are. They are not always clear. We need more information from patients about those first symptoms to give patients confidence in treating attacks early.” Betschel continued that, in paediatrics, there is a spectrum of symptoms. Nevertheless, if the symptoms of a prodrome are similar to those of an early-stage attack, then it should be treated. “I favour early treatment, especially if swelling is involved. If a patient understands what their symptoms are, then they should treat.”
Drawing the meeting to a close, Jones posed a final question: “What strategies can we use to help patients feel more in control?” Betschel responded: “Individualised care is great if you have [different treatment] options available,” and added that nurse-led clinics are especially important because there is more time for patients to ask questions in that setting. “The nurses can develop a much deeper relationship with the patient than I can. We also need to encourage patients to engage with patient organisations because they can connect patients.” Betschel added.
Jones concluded, saying: “It does take a village, physicians, nursing staff, patient advocacy groups, patients. We need to ask patients, and they need to be heard and validated. We need to gain trust, and then we can really start to communicate. The nursing staff has that ability to develop multiple touch points and help to build that trust.”




