Erosive pustular dermatosis of the scalp (EPDS) is an uncommon, chronic, and progressive amicrobial pustular idiopathic disorder most commonly occurring on the scalp of elderly females and ultimately leading to scarring alopecia.1 The combination of the clinical picture, negative microbiological exam, and the histopathological exclusion of other inflammatory conditions allows for a correct diagnosis. It is generally accepted that histopathology is nonspecific and of little value in diagnosing EPDS.2,3 To delineate the clinicopathologic spectrum of the disease, the clinical and pathological records of patients with a diagnosis of EPDS from 2011–2016 were reviewed. Thirty patients were identified, including 22 males and 8 females (mean age at disease diagnosis: 77 years). The mean disease duration before diagnosis was 15 months, ranging from 3–36 months. EPDS was clinically suspected in only three patients, whereas nonmelanoma skin cancers comprised the majority of considerations (21/30). Severe androgenetic alopecia was present in 19 patients. Triggering factors included mechanical trauma in 10 patients, surgical procedures in four patients, and herpes zoster virus infection in one patient. Three patients were affected by autoimmune disorders. The vertex was the most common disease location and presentation varied markedly from tiny, erosive, scaly lesions to crusted and haemorrhagic plaques mimicking pustular pyoderma gangrenosum. The pathologic changes differed according to the lesion type, disease duration, and baldness severity.
Biopsies of patients with severe androgenetic or total baldness (Figure 1A) produced specimens showing nonspecific pathologic changes (22/30), including atrophic, eroded and/or thickened epidermis with spongiform pustules and overlying scale-crusts, granulation tissue, variable dermal fibrosis, and hair loss (Figure 1B). The infiltrate was a mix of lymphocytes, neutrophils, and plasma cells. Interestingly, in patients with a hair-bearing scalp (Figure 1C), histopathologic examination identified eight cases with a dense infiltrate of neutrophils and lymphocytes around and within the infundibula of multiple, adjacent terminal hair follicles in concert with prominent spongiosis and focal or total disruption of the follicle wall (Figure 1D). Extravasated erythrocytes were also seen in the surrounding stroma. All patients were treated with high-potency steroids applied topically overnight; 27 patients showed marked improvement after 4 weeks. The remaining three patients were unresponsive to the topical steroids and were treated with low-dose systemic prednisone (0.5 mg/kg/day) for 2 weeks with gradual tapering, and then showed improvement. The maintenance regimen for all patients consisted of twice weekly clobetasol propionate 0.05% ointment applications and sun avoidance.
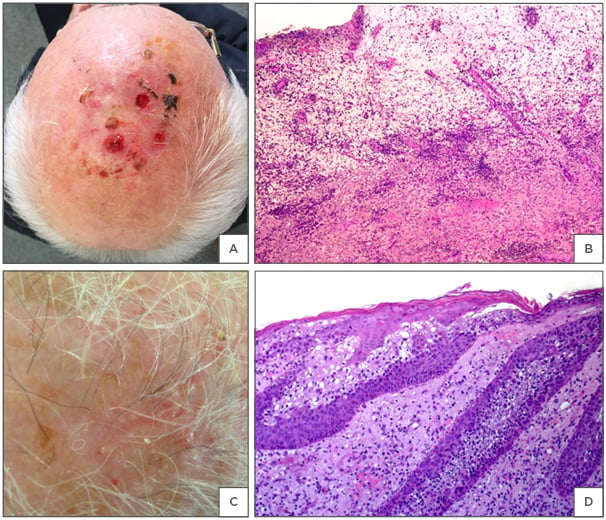
Figure 1: Erosive pustular dermatosis of the scalp.
A) Multiple eroded and crusting lesions localised on the scalp. Diagnostic considerations were actinic keratoses versus squamous cell carcinoma. B) Unspecific histopathological changes characterised by granulation and scar tissue with numerous neutrophils and haemorrhage, viewed using a haematoxylin and eosin stain. C) Follicular pustules and erosions on an atrophic scalp with androgenetic alopecia. D) Spongiotic pustules in the infundibula and erosion of the epidermis, viewed using a haematoxylin and eosin stain.
On the basis of our study, we believe that EPDS is a neutrophilic-mediated skin disorder in which the primary lesion (at least in patients with a hair-bearing scalp) is an infundibular spongiform pustule. The clinicopathologic similarities between EPDS and pustular pyoderma gangrenosum, when lesions do not usually develop into frank ulcerations and infundibular pustules may be observed, suggest EPDS should be included in the spectrum of autoinflammatory dermatoses for which pathergy may play a pathogenetic role.4
The recognition of EPDS is of utmost importance to avoid inappropriate surgical treatments that may lead to a worsening of disease.5







