BACKGROUND
Blaschkitis is a rare, acquired inflammatory dermatosis following the lines of Blaschko, classically seen in adults. Paediatric cases are infrequently described in the literature and may be confused with more common dermatoses such as lichen striatus or atopic dermatitis. The authors present a unique case of paediatric blaschkitis characterised by multilinear distribution and spongiotic histology, adding to the evolving spectrum of Blaschko-linear acquired inflammatory skin eruption.1
CASE
An 11-year-old girl presented with a 3-month history of a mildly pruritic papular eruption involving the left leg, buttocks, and abdomen. Past medical history included eczema and hay fever, and family history was notable for atopy. Prior treatment with topical corticosteroids and oral antibiotics had no effect. On physical examination, numerous erythematous papules had coalesced to form plaques distributed in multiple well-defined bands, 2–5 cm in diameter, in a Blaschko linear fashion (Figure 1).
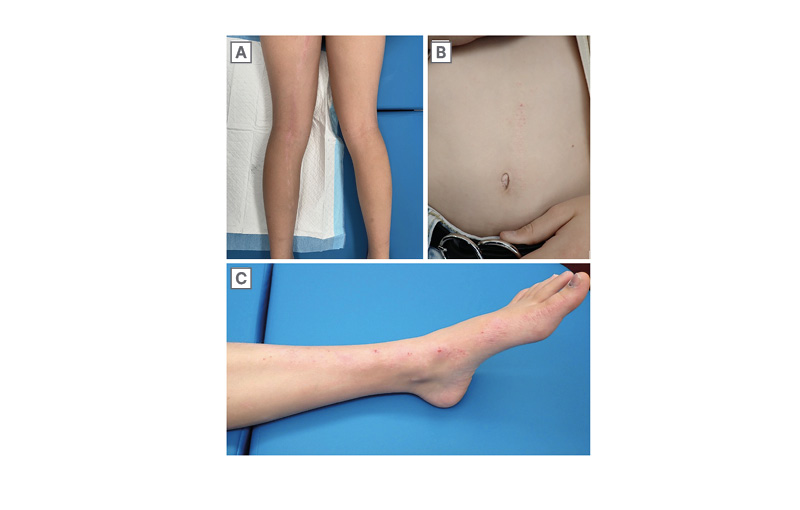
Figure 1: Linear and whorled erythematous plaques following Blaschko’s lines on the posterior aspect of the left leg (A), abdomen (B), and anterior aspect of the left leg (C).
Histopathology revealed an epidermis with foci of spongiosis and patchy parakeratosis (Figure 2). Mild-to-moderate perivascular lymphocytic inflammation was evident in the upper dermis, with infrequent eosinophils. The deeper dermis appeared normal, and no fungal organisms were identified on a combined periodic acid-Schiff/Alcian blue stain. Given the time frame, distribution, and histology, a diagnosis of paediatric blaschkitis was favoured. The lesions were successfully treated with the application of moisturiser several times daily. At the time of reporting, there have been no recurrences.
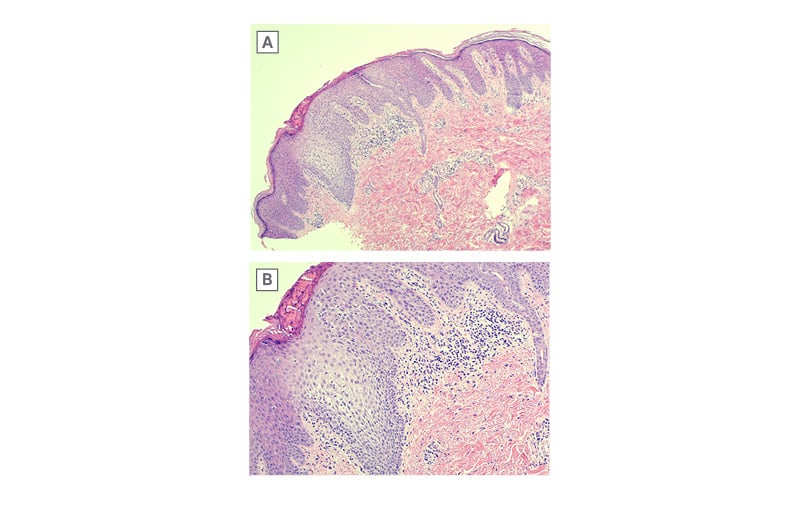
Figure 2: Histopathological features of paediatric blaschkitis.
A) Spongiotic reaction with sparing of deeper dermis (H&E; x25). B) Detail of epidermal spongiosis and lymphocyte exocytosis, with locules of serum in surface parakeratin and no lichenoid component (H&E; x100).
H&E: haematoxylin and eosin.
DISCUSSION
Blaschko’s lines are linear patterns on the skin representing the migration of epidermal cells during embryogenesis.2 Numerous cutaneous conditions present as linear dermatoses following Blaschko’s lines and are a manifestation of cutaneous mosaicism.3 Lichen striatus (LS) is the most common acquired Blaschko-linear dermatosis, primarily affecting children 5–15 years of age.4
It is characterised by an eruption of hypopigmented to erythematous papules that coalesce to form a solitary, narrow band distributed along the extremities.4 LS is typically asymptomatic and self-limiting, with histology showing spongiosis accompanied by lichenoid and periadnexal inflammation.4 In contrast, ‘adult blaschkitis’ is an acquired Blaschko-linear dermatosis distinguished from LS by its later age of onset, truncal distribution, and multiple broad bands.5 Whilst its time course is rapid (1–4 months), relapse is commonly observed.5 On histology, blaschkitis features a primarily spongiotic rather than lichenoid dermatitis.5
Adult blaschkitis and paediatric LS have historically been regarded as distinct conditions. However, rare cases of blaschkitis in children and LS in adults have been reported.3,4 It has since been proposed that they represent two endpoints of Blaschko linear acquired inflammatory skin eruption, a spectrum of acquired dermatoses characterised by their inflammatory infiltrate and distribution along the lines of Blaschko.3,4 Clinically, the authors’ patient’s papulovesicular plaques distributed in a multilinear pattern are consistent with blaschkitis. The presence of spongiosis and focal parakeratosis in the absence of lichenoid and deep periadnexal inflammation further supports this diagnosis.
CONCLUSION
The authors’ report reinforces the relevance of clinical–histological correlation and contributes to growing recognition of blaschkitis in the paediatric population. Improved awareness of this condition may prevent misdiagnosis and unnecessary treatment.







