BACKGROUND
Leishmaniasis is a widespread protozoan zoonosis transmitted by sandflies that can cause a wide range of clinical manifestations. Cutaneous leishmaniasis (CL) is the most common form, usually presenting as a small papule on an exposed skin area that enlarges and finally ulcerates. Therapies for CL are limited, and the systemic treatments available are hampered by toxicity and parasite resistance. As an alternative, photodynamic therapy (PDT) has been reported to be a safe and effective treatment for CL.1,2
CASE REPORT
A female in her 60s presented with a solitary violaceous papule on her left cheek that had progressively enlarged over the previous 4 months (Figure 1A). Travel history was significant for a trip to Peru, in urban areas, 1 year prior to the current chief complaint. Dermoscopy examination showed comedo-like openings and few focused telangiectasias (Figure 1B). Reflectance confocal microscopy (RCM) revealed dilated follicular openings in the epidermis, marked adnexal structures, and prominent horizontal vessels in the superficial dermis. Histological examination showed non-necrotizing granulomas and intracytoplasmic structures compatible with amastigotes, confirming the diagnosis of CL (Figure 1D-F). The patient was treated with three courses of photodynamic therapy. A CO2 fractional laser was used as a drug delivery technique.3 After the third session, the lesion showed complete clinical response with excellent cosmetic results (Figure 1C). To confirm treatment response, RCM was performed demonstrating a regular honeycomb pattern, an unremarkable dermoepidermal junction, and normal dermal features 2 months later. The patient has not presented a relapse of the lesion during follow-up.
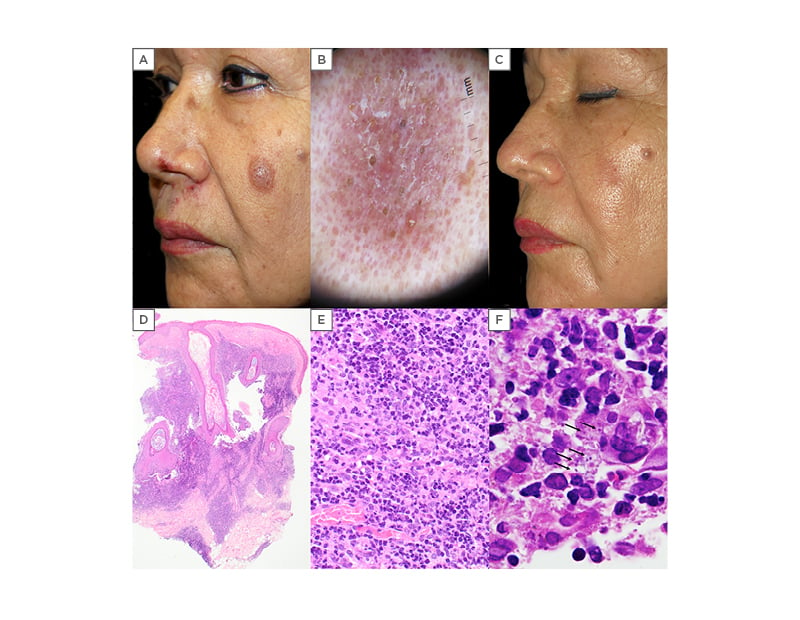
Figure 1: A) Initial clinical presentation showing a violaceous plaque on the left cheek. The patient also presented with multiple grouped erosions with superficial crusts on her upper lip and surrounding her left nasal meatus consistent with a Herpes Simplex recurrence; B) dermoscopy revealed superficial scales, orange comedo-like openings and white interfollicular structures over an erythematous background (DL100, 3Gen, California); C) clinical resolution after three sessions of photodynamic therapy, leaving a residual hypopigmented superficial scar; D) lesional biopsy specimen. Histological findings of flattened epidermis, with marked dilation of the follicular infundibulum and a mixed dermal inflammatory infiltrate with sparing of the papillary region (H-E, x2); E) inflammatory infiltrate consisting primarily of lymphocytes, plasma cells, and histiocytes in the dermis (H-E, x40); F) scattered intracytoplasmic structures (arrows), consistent with leishmania amastigotes (H-E, x100).
H-E: haematoxylin and eosin stain.
DISCUSSION
Although CL is usually a self-limited infection, treatment is advised to avoid ulceration, scarring, or disease progression. CL may constitute a therapeutic challenge, since evidence for an optimal treatment is ambiguous.4 Systemic drugs have potential adverse effects, and the risks and benefits of the available therapies should be discussed with every patient. In recent years, PDT has been introduced as a safe and effective alternative therapy for CL, with only mild side effects and excellent cosmetic outcomes.1,5 It has been reported as a successful treatment for CL in at least 75 cases, some with complex CL due to facial involvement. PDT protocols for treating CL have not yet been standardised. In most reported cases, topical 5-aminolevulinic acid or methyl aminolevulinate were applied as photosensitisers, followed by incubation and red-light irradiation, with 3–8 weekly sessions. Despite the limitation of in-depth evaluation, RCM can help to rule out common tumours of the face as it can show findings more suggestive of CL such as dilated linear and comma-shaped vessels, follicular plugging, and the presence of multinucleated giant cells in the superficial dermis.6 RCM, along with dermoscopy, could be a useful, non-invasive tool, not only to provide an in vivo diagnosis, but also to monitor healing, avoiding unnecessary biopsies or additional PDT sessions.
CONCLUSION
PDT is an effective and well-tolerated therapeutic option for the treatment of simple CL. The use of fractional CO2 lasers as a drug-delivery method could improve the results and shorten the number of PDT sessions needed. Further studies are needed to evaluate its use in cosmetically relevant regions and establish the optimal PDT protocol for treating CL. RCM is a promising complementary tool in the diagnosis and follow-up of patients with CL.








