Abstract
Introduction:
For improving vaginal rejuvenation and minimizing vaginal laxity, the increased demand for soft tissue fillers may give females seeking such therapies the chance to have better general health and sexual performance. To address a wider range of female health issues, and support a more all-encompassing approach to personal wellbeing as cosmetic treatments improve, it is crucial to research the possible repercussions of these minimally invasive operations.
Methodology:
The strength of pelvic floor muscles was measured using the Laborie Peritron 9300 (Portsmouth, New Hampshire, USA) perineometer. A 110 mm long conical vaginal probe with a 26 mm diameter, that may extend to 33 mm under pressure, is a characteristic of this device. The vaginal probe is connected to the perineometer’s main body by an 80 cm plastic tubing. When the probe is squeezed, the gadget has a pressure sensor that tracks vaginal pressure. A silicone rubber sensor loaded with air is included into the probe itself, to detect pressure in cmH2O. The Female Sexual Distress Scale-Revised (FSDS-R) was used to measure the participants’ degrees of sexual distress, and this method made it easier to gauge the participants’ pelvic floor muscle strength.
Results:
The participants’ mean age was 39.43±2.12 years, and further demographic characteristics provided evidence that 44% of the participants were married for 10 years and had children; 36% were married for 5 years with no children; and 20% had been married for less than 5 years.
Conclusion:
Soft tissue fillers, which have shown a rise in popularity, are a viable means of resolving issues with vaginal elasticity and rejuvenation.
Key Points
1. The study focuses on the importance of dermal filler therapy in improving both physical and emotional aspects of female health, addressing issues like vaginal laxity and sexual distress effectively, and less invasively.2. The combination of perineometer and the Female Sexual Distress Scale-Revised (FSDS-R) demonstrates effective results, promoting a holistic approach to female wellbeing.
3. This study is not only filling a gap in the current research, but also providing a viable option for females experiencing vaginal laxity and sexual distress, which is also non-invasive.
INTRODUCTION
Female health has become one of the most discussed issues today. Many problems, like uterine prolapse, birth injuries, incontinence, and general vaginal health concerns cannot be neglected.1 Though vaginal laxity is associated with aging, and is rare in young females, it can occur due to many factors, including childbirth, hormonal imbalance, the intake of certain medications, or any pelvic surgery.1 Over 20 million females suffer from these conditions, due to reasons like increasing age, with factors like vaginal relaxation syndrome affecting wellbeing.2 Until recently, these topics were considered taboo, even among medical professionals.2,3 A survey conducted on female health reported that 95% of doctors assume vaginal laxity negatively impacts sexual function, yet only 14% of females opt for help regarding female sexual dysfunction, while experiencing psychological distress.4 However, public awareness campaigns have neutralized this taboo a lot. Doctors have taken education initiatives, including media coverage, leading to increased treatment demand.6,7 Due to increased knowledge, alternate interventions are being introduced, such as nonsurgical procedures, with a 30% rise in vaginal rejuvenation treatments between 2005–2006.7 There has been an increased approach towards cosmetic vaginal rejuvenation from 3.90% in 2012, to 28.97% in 2015.8 Minimally invasive procedures are preferred, with significant growth in botulinum toxin Type A operations (759%) and soft tissue fillers (274%) since 2000.9 Although significantly lower from 2014, by 9%, microdermabrasion has nevertheless had an overall increase of 8% since 2000.10 An increasing tendency in favor of non-surgical solutions for improving one’s beauty and general wellbeing is highlighted by this move towards the least invasive procedures.10,11 It is important to explore the impacts of these minimally invasive procedures to address a wider variety of female health concerns, and promote comprehensive wellbeing as cosmetic procedures advance.
METHODOLOGY
Study Design
A quasi-experimental study.
Study Setting
The study was conducted at Skin and Laser Clinic, Hyderabad, Pakistan.
Sample Size and Target Population
The study included a total of 25 females, who attended a dermatology clinic for vaginal rejuvenation and opted for dermal filler intervention.
Inclusion and Exclusion Criteria
Married females aged between 20–50 years in good health, who had provided consent to undergo filler cosmetic procedure for vaginal rejuvenation, were included; whereas pregnant females, and those below and above the given age limits, were excluded.
Intervention Strategies
The injection site was initially numbed with 1–2 mL of mepivacaine 2%, injected with epinephrine 1/100,000 on both sides, to promote a comfortable and less intrusive experience. For the technique, mannitol, a strong antioxidant recognized for its capacity to prevent the degradation of hyaluronic acid (HA), was added to pre-filled syringes containing cross-linked, non-animal HA. A filler with a peri 19 mg/mL HA content (referred to as ‘19 mg/mL HA filler’) was used to treat moderate hypotrophy. A filler with a concentration of 21 mg/mL HA mixed with mannitol (referred to as ‘21 mg/mL HA filler’) was favored in situations with moderate-to-severe hypotrophy. A 30-gauge needle was used to inject the first filler, and an 18- or 21-gauge cannula was used to insert the second filler. An initial entry point was made using a 19G needle in cases when the cannula was required. Two layers were engaged in the injection procedure. One-third of the filler was deliberately injected between the fibrous tunic and the lip dartos (a layer of smooth muscle cells found just beneath the skin), with the remaining two-thirds going into the subcutaneous layer. The longitudinal axis of the labia minora was aligned with the fan-shaped arrangement of these injections. In order to get the best results, the operator was able to spread the filler uniformly. Recommendation was made for the regular use of topical antibacterial and antimycotic therapy with phenethyl alcohol for 1 week. A 6-day course of antibiotic prophylaxis with amoxicillin clavulanate was advised for patients who had received 21 mg/mL HA filler via an 18- or 21 gauge cannula. At each session, there is an involvement of a total of four injections as a treatment protocol. Each injection consisted of 0.125 mL of the solution, making it certain that the delivery of HA filler is precisely controlled. This standardized approach allowed for consistent dosing and distribution of the filler across the treatment site, optimizing the therapeutic outcome for patients undergoing the procedure. This strategy was motivated by the realization that yeast and germs from the vagina and anus might potentially contaminate the vulvar region. However, Candida albicans generally produced vulval itching, Trichomonas vaginalis and Gram-negative bacteria were linked to vaginal discharge, and yeast and fungus were present in the vaginal flora of 21% of females, often without symptoms. Beyond these instances, germs and fungus often did not cause symptoms or abnormal discharge. Additionally, considering that greater cutaneous access often heals without sutures, antibacterial prophylaxis was provided to individuals who had received 21 mg/mL HA filler infiltration. HA was softly and progressively injected, with aspiration serving as a regular check to ensure that intravascular injection was avoided. Having a blunt tip was desirable when utilizing a cannula. Consideration of hyaluronidase usage was advised in cases of severe, excessively superficial, or non-homogeneous infiltration, as well as when patients displayed fast skin darkening, discomfort, or reticulated erythema.
Outcome Measures
During the study, the Laborie Peritron 9300 (Portsmouth, New Hampshire, USA), was used to measure the strength of the pelvic floor muscles. This perineometer has a conical vaginal probe that is 110 mm in length, with a measured length of 55 mm, and 26 mm in diameter (33 mm when pressurized). An 80 cm plastic tube connects the vaginal probe to the perineometer’s main body. A pressure sensor inside the gadget monitors the vaginal pressure when the probe is compressed by vaginal pressure. The probe itself has a silicone rubber sensor that is filled with air, and measures pressure in cmH2O. The perineometer’s values of occlusive pressure are substitute indicators of pelvic floor muscle strength. This methodology made it possible to measure the research participants’ pelvic floor muscle strength. The participants’ sexual distress was assessed using the Female Sexual Distress Scale-Revised (FSDS-R). The perineometer was used twice to test muscle strength at baseline, and at the end of study.
Data Analyses Strategies
Data were analyzed using SPSS version 26 (IBM, Armonk, New York, USA). Demographic details were illustrated in the form of frequency and percentage tables, whereas for inferential statistics paired t test at 95% confidence interval was applied.
Ethical Considerations
The study was carried out according to the guidelines of the Belmont report, as laid down for human subjects. All participants were informed regarding the purpose of study prior to induction, written consent was taken, and autonomy was given to leave the study at any time without assigning any reason. Moreover, principles of beneficence and non-malfeasance were maintained throughout the study, and keen steps were taken to maintain the confidentiality of participant’s information obtained during the course of study.
RESULTS
The analyses of the findings revealed that the mean age of the participants was 39.43±2.12 years, and further demographic characteristics provided evidence that 44% of the participants had been married for 10 years and had children; 36% were married for 5 years with no children; and 20% had been married for less than 5 years. Detailed demographic features are provided in Table 1.
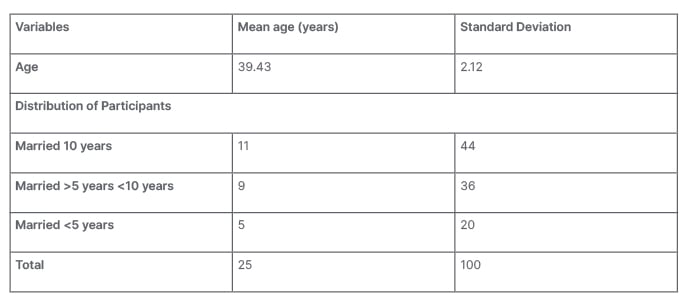
Table 1: Demographic characteristics of participants.
The effects of intervention were determined on vaginal muscle tone using a perineometer. Analyses of the findings revealed that at baseline, the vaginal muscular tone was 23.25±3.09 cmH2O, and improved to 27.56±2.11 after intervention. Inferential statistics revealed that the difference between the mean was significant (p<0.05), hence suggesting beneficial effects of dermal filler treatment in improving vaginal laxity (Table 2). Further, the effects of treatment were also determined on FSDS-R, and the findings revealed that at baseline, the values were 29.65±2.31, and were reduced significantly to 15.45±1.25 (p<0.05). Detailed descriptions of the findings are illustrated in Table 2.
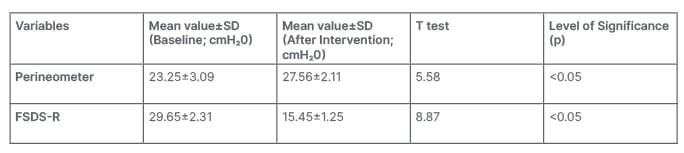
Table 2: Within group analyses to determine the effect of intervention on outcome measures.
FSDS-R: Female Sexual Distress Scale-Revised; SD: standard deviation.
DISCUSSION
In this study, the authors examined the influence of dermal filler therapy on female sexual discomfort, as well as its effects on vaginal muscle tone using a perineometer. Results showed that the intervention significantly improved the muscle tone of the vagina. The initial assessment of vaginal muscle tone was 23.25±3.09 cmH2O; however, following the intervention, this value significantly increased to 27.56±2.11 cmH2O (p<0.05). The FSDS-R was used to assess the effect of the therapy on the participants’ levels of sexual distress. The subjects’ first baseline FSDS-R scores were recorded at 29.65±2.31, indicating a significant level of sexual discomfort. However, following the intervention, there was a marked decline in these scores, with a statistically significant drop to 15.45±1.25 (p<0.05). These results point to the potential of dermal filler therapy as a valuable therapeutic option for enhancing the physical and emotional aspects of patient health, in addition to beneficial effects on vaginal muscle tone and sexual distress in the participants.
A study was performed to treat females with vaginal laxity, genitourinary syndrome of menopause, and vulvar cosmetic problems, through a non-surgical radiofrequency method paired with an injection of HA into the labia majora skin.12 The therapy considerably improved clinical results, as seen by better scores on the Vaginal Laxity Questionnaire (VLQ), Vaginal Health Index (VHI), and Female Sexual Function Index (FSFI), including 20 females with ages ranging from 36–72 years (mean age: 53.4).12 These 20 patients reported of sexual discomfort in the form of dyspareunia. Histological study showed greater levels of elastin and collagen in the vulvar skin and vaginal wall following the surgery (vulvar skin: elastin 61%, collagen 27%). Patient satisfaction was also significantly higher. These results demonstrate the effectiveness and safety of this radiofrequency and HA combination therapy, providing a viable approach to resolving the physiological, psychological, and cosmetic issues frequently connected to genitourinary syndrome of menopause, vaginal laxity, and vulvar health.12
The many uses of HA in the field of cosmetology have been explored in research, which highlighted its critical function in both non-invasive skincare through topical preparations and injectable procedures, such as dermal fillers. It also discusses the less important, but still significant functions, of HA in oral supplementation and vaginal preparations.13,14 The results show a growing understanding of HA’s esthetic potential among prospective beauty spree customs. While HA-based topical skincare treatments are in demand for their capacity to preserve skin moisture and counteract transepidermal water loss, HA injections, typically targeting regions like the lips, are favored for restoring skin firmness and smoothness. Rare side effects are frequently caused by immunological reactions.15 Temporary localized soreness at the injection site was the most frequent side effect; no significant adverse events were observed.
Multiple studies have suggested that HA functions as a versatile tool in cosmetology, enhancing skin vitality, and satisfying social demands for increased beauty and wellbeing.16,17 Multiple studies also suggest the benefits of HA for vaginal laxity.12,19-20 A well-defined approach, with in-depth explanations of the intervention and outcome measures, is one of the study’s many strengths. The findings are given more credibility by the use of objective tests, like the FSDS-R, and the Peritron 9300 perineometer. A dedication to patient safety is shown by the extensive safety precautions used, such as an antibiotic prophylaxis, and considerations for the use of hyaluronidase. But there are some restrictions that need to be understood. The study used a quasi-experimental methodology that could introduce bias and restrict causal inference by omitting randomization and control groups. Its Hyderabad single-center location might make it harder to generalize to a larger population. Questions concerning the longevity of reported results are raised by the study’s brief or undefined follow-up time.
CONCLUSION
In conclusion, the outcomes of this study are positive. The intervention showed great promise in addressing physical elements of female health by considerably increasing vaginal muscle tone. Together, these results indicate that dermal filler therapy has potential as a useful and less invasive therapeutic alternative, not only for improving physical features but also for fostering mental and sexual wellbeing in females.






