Abstract
Brucellosis is a zoonotic infectious disease of worldwide distribution and is still endemic in some developing countries. Brucellosis is a systemic disease in which any organ or system of the body can be involved. The most commonly affected systems are the locomotor, gastrointestinal, genitourinary, haematological, cardiovascular, respiratory, and central nervous systems. Cutaneous manifestations are rare in brucellosis and the lesions are not specific to the disease. Skin involvement is reported to range between 0.4% and 17.0% of the patients with brucellosis. The cutaneous manifestations in brucellosis are seen because of the direct inoculation of bacteria into the skin, hypersensitivity phenomena, deposition of immune complexes in the skin, and invasion of the skin via a haematogenous route of spread of the micro-organism. Papulonodular and maculopapular eruptions, and erythema nodosum-like lesions are the most frequently encountered cutaneous lesions in brucellosis. Brucellosis should be kept in mind by clinicians in the diagnosis of patients with complaints of fever and eruptions, especially in endemic regions.
INTRODUCTION
Brucellosis is a zoonotic infectious disease of worldwide distribution, it is still endemic in some developing countries and it causes substantial morbidity in both human and animal populations. Major endemic areas are the Mediterranean Basin, Persian Gulf, Indian mainland, Mexico, and Central and South America.1-4 The disease is also a major cause of public health problems and economic loss in many developing countries. Brucella melitensis infection causes a serious public health problem in bovines in some countries. A similar condition is observed in cattle with Brucella suis biovar 1 in South American countries.4 Brucellosis commonly affects sheep, goats, cattle, water buffalo, and pigs, and it is transmitted directly or indirectly to humans from these animals. Among the Brucella species which are causative agents of disease in humans, B. melitensis leads to disease principally in sheep and goats, Brucella abortus in cattle and water buffalo, B. suis biovar 1–3 in pigs and B. suis biovar 4 in deer.1,5 The principal pathogenic species of Brucella worldwide are B. abortus, B. melitensis, and B. suis. These three types of Brucella strains lead to great economic loss, usually by causing abortion in animals and they are also causative agents in most brucellosis cases in humans.
Brucella bacteria are found in urine, milk, placenta, and other animal bodily secretions.1,5 Humans generally acquire the disease by consuming foods such as unpasteurised milk (e.g. cream, butter, ice cream), cheese, and undercooked meat from the infected animal. Humans may also acquire the disease through coming into conjunctival contact with secretions of infected animals via non-intact skin lesions in their hands and arms and inhalation of infected aerosols.1,6-8
Brucellosis is a systemic disease in which any organ or system of the body can be involved.1,9 The most commonly affected systems are the locomotor, gastrointestinal, genitourinary, haematological, cardiovascular, respiratory, and central nervous systems.10 Infection can be manifested by local or systemic symptoms. Localised infection can be seen in approximately 27.7–43.2% of patients. When localised infection is seen as a result of systemic infection, it can also be called a complication. It can be observed in acute, subacute, and chronic infections.1,2,10-17 Skin involvement observed in patients with brucellosis was described in 1940.18 Skin involvement is reported to range between 0.4% and 17.0%.2,10,13,16-31 It is rare and the lesions are not specific to brucellosis.19 Due to its non-specific nature and rarity, in this review we evaluate misdiagnosed skin involvement associated with brucellosis and raise awareness about this manifestation of brucellosis.
PATHOGENESIS
The cutaneous manifestations in brucellosis are seen because of direct inoculation of the bacteria into the skin, hypersensitivity phenomena, deposition of immune complexes in the skin, and invasion of the skin via a haematogenous route of spread of the micro-organism.32 Skin lesions can be seen because of a direct effect of microbial replication, host response to bacteria, or interaction between them.33 The invasion of skin via a haematogenous route of spread of Brucella bacteria is the most important underlying pathological mechanism of cutaneous lesions. Direct invasion of the skin by the bacteria reaching the skin through the haematogenous route and endotoxins released from the bacteria may explain the effect during the acute phase of the disease. Hypersensitivity phenomena, deposition of immune complexes in the skin, and granuloma formation may cause the cutaneous manifestations observed during the chronic phase of the disease.18,19,34
THE CUTANEOUS LESIONS OBSERVED DURING THE COURSE OF BRUCELLOSIS
There are a limited number of studies evaluating the cutaneous lesions associated with brucellosis. Relevant studies and the most frequently observed cutaneous lesions are shown in Table 1. When the studies performed were evaluated, it was seen that papulonodular and maculopapular eruptions and erythema nodosum-like lesions were the most frequently encountered cutaneous lesions in brucellosis and they were located on the trunk and lower extremities in most of the patients.1,21,22,24,25,27,32,35,36 The cutaneous manifestations of brucellosis are summarised in Table 2.
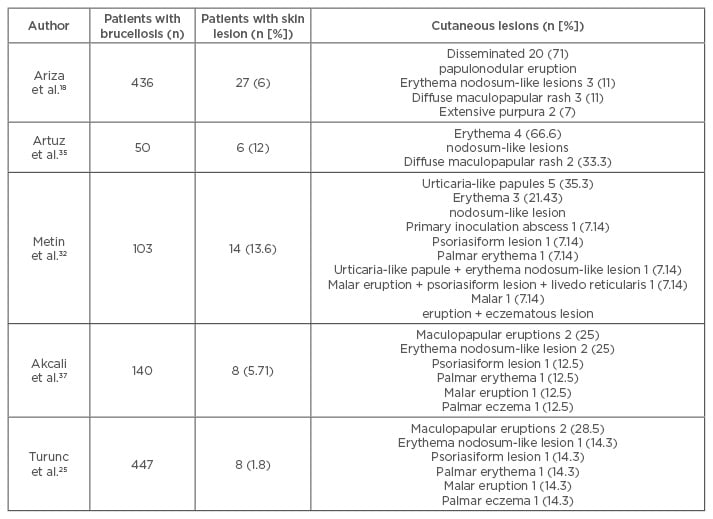
Table 1: Study abstracts of cutaneous manifestations associated with brucellosis.
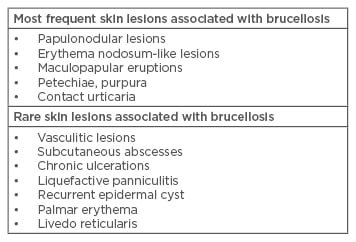
Table 2: Summary of skin lesions associated with brucellosis.
DISSEMINATED PAPULONODULAR LESIONS
It has been observed that disseminated papulonodular lesions accounted for approximately 32% of the cases in the studies examining cutaneous manifestations in brucellosis.18,25,32,35,37 Disseminated papulonodular lesions have a smooth surface, they are erythematous, and they are frequently seen on the upper trunk, shoulders, and thighs, and especially the lower legs. Skin lesions were non-pruritic with their sizes ranging from a few millimetres to >1 cm. There were central ulcerations in some lesions. Brucella bacteria were isolated from some cultures performed from papulonodular lesions. This suggests that these lesions were caused by the haematogenous route of spread of the micro-organism during the bacteremic phase of the disease. When disseminated papulonodular lesions were evaluated histologically, it was observed that there was an inflammatory process consisting of perivascular and periadnexial regions localised principally in the dermis and a granuloma structure. The same granulomatous findings were also discovered in erythema nodosum-like lesions, which were another frequently encountered lesion. It is believed that both lesions develop as a result of a similar pathogenetic mechanism.18,38,39
ERYTHEMA NODOSUM-LIKE LESIONS
Erythema nodosum-like lesions account for 25% of the cutaneous lesions associated with brucellosis. Erythema nodosum-like lesions develop due to hypersensitivity phenomena or involvement of the panniculus because of the haematogenous route of spread of the micro-organism. The cutaneous lesions associated with brucellosis are characterised by multiple erythematous nodules and located on the extensor surfaces of the lower legs. Lesions are usually painless. While these lesions are clinically similar to erythema nodosum, they are histologically different from the classical erythema nodosum. There is no deep dermal tissue inflammation or invasion of fat lobules in erythema nodosum. Additionally, plasma cells and necrosis seen in erythema nodosum-like lesions associated with brucellosis are not observed.18,19,37,38
MACULOPAPULAR ERUPTION
The pathogenesis of maculopapular eruption is not known. Although involvement is widespread in diffuse maculopapular eruption, the lower extremities are especially affected. There is no pruritus of the skin. While no previous drug use has been reported in most of the cases, drug reaction should be necessarily excluded in diffuse maculopapular eruption.18,35
VASCULITIC LESIONS
Vasculitic lesions associated with brucellosis were reported as case presentations (Figure 1).40-50 Yrivarren and Lopez41 described cryoglobulinaemia and cutaneous vasculitis in three patients with brucellosis. Hermida Lazcano et al.42 reported a case with renal failure, cutaneous vasculitis, and peritonitis due to brucellosis and they concluded that the entire clinical picture (renal, hepatic, and cutaneous) was mediated and/or caused by cryoglobulins. Dizbay et al.43 determined hypocomplementaemia, increased levels of polyclonal immunoglobulins, positivity of rheumatoid factor, and perinuclear anti-neutrophil cytoplasmic antibodies in their patients with renal failure and leukocytoclastic vasculitis due to brucellosis; the authors stated that they thought that this picture was caused by mixed cryoglobulinaemia. In general, it is considered that immunological mechanisms play a role in the pathogenesis of these lesions.32

Figure 1: Non-blanchable maculopapular eruptions on the anterior parts of tibias in a patient with leukocytoclastic vasculitis and brucellosis.
Adapted from Korkmaz et al. 2016.45
ALLERGIC LESIONS
A hypersensitivity reaction may also cause the cutaneous lesions observed in brucellosis. While the relationship between lesions and hypersensitive reactions could not be described exactly, cases of allergic vasculitis are reported.46-48 Contact urticaria is an erythematous eruption observed in veterinary physicians and pet-sitters. Eruption begins with pruritus and erythema in the upper extremities within a few hours after exposure, sometimes face and neck may be involved, and the lesion improves approximately within 2 weeks.38 Trunnell et al.49 suggested that the pathogenetic mechanism causing contact urticaria could be an allergic hypersensitivity reaction.
OTHER LESIONS
Multiple cutaneous and subcutaneous abscesses and chronic ulcerations have been described in brucellosis patients with high occupational exposure risk.50,51 Additionally, purpuric eruptions associated with coagulation disorders can also be seen in brucellosis patients.18,52,53 Vaccination is effective in cattle. However, live animal vaccines may cause disease in humans.4 Also, the occurrence of local reactions (swelling, redness, pain) and deep dermal nodules due to the Brucella toxin after accidental inoculation of the Brucella vaccine was reported.54
CLINICAL CHARACTERISTICS
The cutaneous lesions associated with brucellosis can be seen in every phase of the disease. In a study performed by Metin et al.,32 103 brucellosis cases were evaluated and skin involvement was determined in 14 (13.59%) of these patients. In this study, the cutaneous lesions occurred in chronic, acute, and subacute phases of the disease in 50.0%, 35.7%, and 14.2% of the patients, respectively. In a study performed by Akcali et al.,37 140 brucellosis cases were evaluated and skin involvement was determined in 8 (5.71%) of these patients. In this study, the cutaneous lesions occurred in the acute phase of the disease in 62.5% of the patients. Skin lesion was observed in 27 (6%) of 436 brucellosis patients in a study performed by Ariza et al.18 Skin lesion was observed in 24 patients at the initial period, in 4 at relapse, and in 1 both at the initial period and at relapse.18 In a study performed by Buzgan et al.10 evaluating 1,028 brucellosis cases, the rate of skin involvement was 2.4% and the rates of cutaneous lesions in acute, subacute, and chronic periods of the disease were 2.4%, 3.2%, and 2.1%, respectively. When the case presentations were evaluated, it was observed that the cutaneous lesions were usually determined in the acute phase of brucellosis.38,42,44,54-56 Since cutaneous lesions observed in brucellosis are non-specific, the time of determination of the lesion may have varied in the studies performed.
When the studies related to the cutaneous lesions associated with brucellosis were evaluated, fever was observed in all cases except chronic patients.25,44,45,55-58 Since systemic symptoms generally predominate in the patients with brucellosis and the cutaneous lesions regress with anti-brucellosis treatment, presentation to the dermatology clinics is rare. Since the cutaneous lesions are non-specific, it is difficult to diagnose some subacute and chronic cases.18,32,35,38,54
Therefore, brucellosis should be kept in mind in the differential diagnosis of cases of fever of unknown origin, especially in regions where brucellosis is endemic. When the brucellosis patients with and without cutaneous lesions were evaluated regarding systemic symptoms and clinical findings, no difference was determined.18,32,35 When the patients with brucellosis were evaluated by sex, cutaneous lesions were more commonly seen in females.18,32,37
DIAGNOSIS
The definitive diagnosis of brucellosis requires the isolation of Brucella species from blood, bone marrow, or tissue samples. A culture should be performed from the affected area in the presence of focal complications. The Brucella bacterium grows slowly in vitro media. DNA amplification using polymerase chain reaction can be used in the blood and non-blood samples. Polymerase chain reaction is more sensitive than the culture irrespective of the stage of the disease; it can be used for identification of the bacterium in the tissue.1,5,59
The cutaneous lesions associated with brucellosis can be diagnosed histopathologically. Biopsy should be performed for all of the cutaneous lesions. Frequently there is a granulomatous structure in these lesions. The presence of plasma cells and necrosis in erythema nodosum-like lesions associated with brucellosis is beneficial for differential diagnosis from the classical erythema nodosum. However, histological changes may be insignificant in some patients and they can be observed as mild cell infiltration without a granulomatous structure.18,38,54
Since brucellosis is a multi-systemic infectious disease, it should be considered for the differential diagnosis of patients with rash and fever. However, skin involvement is generally not specific to brucellosis. This can be beneficial for the differential diagnosis of the lesions in the presence of non-specific complaints such as fever, fatigue, joint pain, and contact with animal tissues or consumption of non-pasteurised dairy products, especially in individuals living in endemic regions. It is necessary to increase awareness among clinicians and especially dermatologists in regions where the disease is endemic.
TREATMENT
There are two major treatment regimens for the treatment of uncomplicated brucellosis (without features such as spondylitis, neurobrucellosis, and endocarditis) in adult patients. The treatment regime of doxycycline (2×100 mg/day, 6 weeks) and streptomycin (1 g/day, 2–3 weeks) recommended by the World Health Organization (WHO) for combination treatment is used for the treatment of brucellosis. Another combination treatment recommended by the WHO is doxycycline (2×100 mg/day) and rifampicin (600–9,000 mg/day) for 6 weeks. In vitro efficacy of quinolones, especially ofloxacin and ciprofloxacin, is good. Although high relapse rates were observed with quinolone monotherapy, successful results were obtained with combination treatment; however, they were not first-line agents.1,5 In the presence of focal involvements such as neurobrucellosis, endocarditis, and spondylitis, the period of treatment should be longer (at least 8–12 weeks) and combination treatment with at least three drugs is frequently recommended. In general, the type and period of treatment in other forms of localised infection is as in uncomplicated brucellosis cases.1,5,60`
Type and duration of treatment of brucellosis patients with cutaneous lesions is not different from classical treatment. It was observed that a regression occurred in the lesions within the first week after starting anti-Brucella treatment.18,38,44,45,55,56 It was observed that this period of regression was as long as 1 month in some patients.39 Classically, the period of regression was 6 weeks in the patients where the duration of treatment was indicated.38,44,49,55-57
CONCLUSION
Brucellosis is an important public health problem causing substantial morbidity in both human and animal populations. While skin involvement is rare in brucellosis, a patient with brucellosis may primarily present with cutaneous lesions. Cutaneous manifestations are not specific to brucellosis and the differential diagnosis can be made histopathologically. Brucellosis should be kept in mind in the differential diagnosis of patients with non-specific complaints of fever, weight loss, muscle, and joint pain who consume unpasteurised dairy products and engage in animal breeding in case of the presence of skin eruptions, especially in the endemic regions.







