Abstract
Trichotillomania is defined by the Diagnostics and Statistic Manual of Mental Disorders (DSM-5) as an individual repetitively pulling of their own hair, which may be an unconscious action or intentional. The disease is considered one of the anxiety disorders as it has some obsessive-compulsive features. Many patients with this disorder go to a dermatologist for the first time with a complaint of hair loss (alopecia), and many of them deny the self-pulling behaviour. In rare circumstances, this psychological problem may coexist with a complication called gastric trichobezoar, like in this unusual case presentation, which is an accumulation of the patient’s hair in their stomach. It can be huge, presenting as a ‘tail’ extending into the duodenum and leading to what is referred to in the literature as ‘Rapunzel syndrome’. Gastric trichobezoars are most often seen in teenage females. Trichophagia has only been previously confirmed in one-third of these patients, but this is usually a late presentation, occurring after much hair eating for many years.
Key Points
1.Trichotillomania is an anxiety disorder-related behaviour where an individual repetitively pulls their own hair and can be complicated by subsequent gastric trichobezoar, particularly if the underlying trichotillomania is not recognised or addressed in a timely manner.2. This case shares a complicated presentation with multi-specialty involvement: psychiatry, dermatology, and gastric surgery. Diagnostic delay in alopecia can be due to confirmation challenges, as many patients and their families deny any obsessive–compulsive behaviours, and this delay may have significant consequences, such as gastric obstruction following protracted trichophagia.
3. Clinicians should always consider the psychological and emotional background of any toddler or adolescent presenting with a non-specific and unexplained long-standing skin rash or skin appendage changes (hair and nails).
INTRODUCTION
Trichotillomania (TTM) is a mental illness characterised by self-inflicted skin abnormalities. It is strongly linked to anxiety disorders. The American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies it as an impulse control disorder.
DSM-5 criteria for TTM include hair loss as a result of frequent plucking out of one’s hair; frequent attempts to reduce or eliminate hair pulling; the disruption results in clinically substantial distress or impairment in essential social, occupational, or other aspects of functioning; another medical problem that cannot be the source of hair tying or loss (e.g., a dermatological condition); and the symptoms of another mental disorder that do not adequately explain the hair pulling (e.g., in body dysmorphic disorder, attempts are made to correct a perceived imperfection or deficiency in appearance).1
This disease has a 1% lifetime prevalence across the board. In adulthood, females are more likely to experience this (ratio: 4:1). More children suffer from this condition than adults, but it is a gender equal disease. The average age of onset is between 10 and 13 years old.1 Clinically, it appears as foci of hair loss, without signs of scarring or skin change, and does not follow a characteristic pattern. Hair of variable lengths and thickness is observed within the affected area on the scalp, on the eyebrows, and on the upper eyelashes. It must be differentiated primarily from the focal forms of alopecia areata.2
The scalp is the most common site for hair pulling, followed by the eyebrows, eyelashes, pubic area, trunk, and extremities.3 Hair pull tests are almost always negative; however, if more than five hairs are extracted, the test is considered positive. Dermoscopy features include hairs of various lengths, hairs that are irregularly coiled, short hairs with split ends, and flame hairs.4 Histology shows intrafollicular fissures and haemorrhages in early phases. Granulomatous changes and/or perifollicular fibrosis may be seen in chronic stages. Other specific signs such as tricheomalacia (injured twisted follicles),2 a rare but sometimes serious complication, or trichobezoar (gastric hair ball) may be reported as in this unique case. It may cause intestinal obstruction, gastric or intestinal bleeding or perforation, acute pancreatitis, and jaundice.5
CASE REPORT
An 11-year-old female was brought to the emergency room of the Children’s Clinical Hospital ZA Bashlyaeva, Moscow, Russia. With a history of periodic moderate abdominal pain for a duration of 2 weeks’, the complaint worsened and became severe the day before the appointment, accompanied by nausea and vomiting. They were a little anxious and afebrile. Their vital indicators were all within normal limits.
Physical examination revealed an epigastric mass and a diffusely tender abdomen, but soft. Rebound tenderness was negative. Abdominal ultrasound showed no air-fluid levels, hepatomegaly, and signs of cholecystitis; however, the stomach looked bloated and was filled with echogenic material, which caused acoustic shadowing in the back. An oesophagogastroduodenoscopy was then performed; the stomach was filled with a massive formation of intertwined hair. A stomach X-ray with contract media revealed heterogeneous dense stomach contents throughout the entire volume (Figure 1). A trichobezoar was diagnosed.
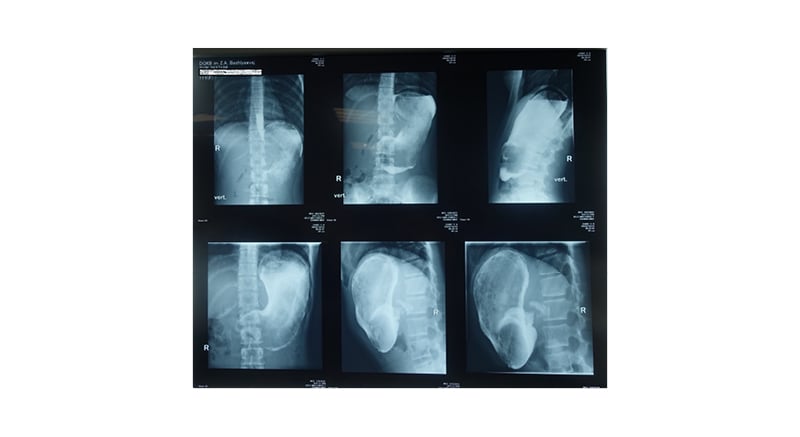
Figure 1: Stomach X-ray with contract media, which revealed heterogeneous, dense stomach contents throughout the entire volume.
Their white blood count was 14,000 with a left shift; haemoglobin: 10 gm/dL; and serum iron: 3.2 μmol/L. Their pancreatic enzyme lipase slightly was elevated, liver enzymes were normal, and serum electrolytes revealed hyponatraemia, which were all found in the laboratory investigation. As the patient prepared for operative laparotomy, a trichobezoar weighing 2.5 lbs was successfully removed (Figure 2). The patient’s postoperative recovery was uncomplicated.

Figure 2: Massive formation of intertwined hair.
On a post-operative dermatological consultation, a doctor found zones of bizarre thinning of sparse hair (diffuse alopecia) with variable lengths, mainly in the frontoparietal areas. The skin of the scalp was smooth and soft, without scaling, erythaema, or damage. There was no scaring or atrophy (Figure 3).

Figure 3: Zones of bizarre thinning of sparse hair (diffuse alopecia) with variable lengths, mainly in the frontoparietal areas.
The hair pull test from the edges of alopecia was negative. A Woods’ light exam to exclude fungal infections was also negative. Trichoscopy findings: decreased hair density, broken hairs of variable lengths, and trichoptilosis (split ends). Short vellus hairs, exclamation marks, or yellow dots were not seen. A blood test found that the patient was nutritional deficit (iron, serum ferritin, zinc, and vitamin B12) and their thyroid hormones were normal. On fungal scraping, there was no growth. A scalp biopsy was not completed. Examination of eyelashes and eyebrows revealed no damage. Other parts of the skin, nails, oral mucosa, and genitalia remain unchanged.
Their family history of alopecia was unremarkable except for their father (42-years-old), who was diagnosed with androgenic alopecia due to frontotemporal recession. Finally, the diagnosis of TTM was confirmed and a shampoo was described for thin hair treatment (DermoCapillaire [Eucerin, Birmingham, UK] or Selencin [Russia]) and thymuskin serum. Also, the patient was prescribed multivitamins with iron supplements for toddlers for their nutritional deficit (NovaFerrum [Greenville–Spartanburg–Anderson, South Carolina, USA) Their parents were advised to prepare a healthy meal filled with essential vitamins. Then, the patient was discharged with recommendations to follow a TTM treatment programme.
After that, the patient was referred for mental evaluation and consultation. The patient was agitated and lacked co-operation, as well as weak eye contact. When they became obsessed and other family members were not watching, such as at midnight or when they were alone, the patient admitted to pulling out their hair and eating it. They denied other behaviours such as nail or lip biting and picking skin. Furthermore, no signs of these actions were detected on clinical evaluation. They were in primary school and had high grades and no social communication issues with their classmates or teachers.
Their parents were completely unaware of their hair-eating habit (trichophagia). Despite this, their mother admitted that they noticed the changes in their daughter’s hair 2 years ago but did not ask for dermatological consultation because of the nature of patient’s parents’ work. The patient’s mother said that they took their daughter to the outpatient clinic after several months, where the doctor suspected malnutrition as a susceptible cause of hair thinning as the patient was under weight and BMI was 18.49. So, the doctor sent the patient to do several blood tests, which revealed iron, zinc, and vitamin D deficiencies. The patient’s mother then decided that these were the causes and that they should take care of their daughter’s diet. The patient’s mother did not return to the dermatology clinic to complete the consultation and diagnosis.
The psychiatrist revealed that the patient did not fully meet the diagnostic criteria for TTM as an obsessive-compulsive disorder (OCD) as defined by the DSM-5 as they did not try to reduce or eliminate hair pulling. In addition to that, their disorder did not significantly affect their social and educational life. However, the other three criteria were present in this patient, including repetitive hair pulling; no other dermatological condition can be the source of her hair loss; and no other psychological problems can better explain this disorder.
Exploring the other family members was unremarkable except for a history of ‘nervous breakouts or feeling down’, which sometimes required anxiolytic medications, so a family history of similar or related disorders was negative. As a result of a long history of hair pulling and hair eating, which had disastrous consequences, the doctor recommended selective serotonin reuptake inhibitors such as low-dose fluoxetine (Prozac [Eli Lilly and Company, Indianapolis, Indiana, USA] 10 mg/day) and N-acetylcysteine (1,200 mg/day) for 12 weeks, as well as cognitive-behavioural therapy. The patient and their parents were warned that long-term regular follow-up is crucial for successful management and to prevent recurrence.
DISCUSSION
In 1889, a French dermatologist coined the term TTM (from the Greek tricho, meaning hair; tillo, meaning pull; and mania, which means excessive enthusiasm). Infantile or early-onset TTM usually resolves on its own or with simple interventions.6 When it occurs later in life, during adulthood, or in elderly patients, it is associated with a poor prognostic outcome. Genetic abnormalities and environmental influences have been linked to TTM and other OCD-related disorders in twin studies.7 There have been reports of structural and functional brain changes. Many neuroimaging studies have revealed abnormalities such as thickening of the right inferior frontal gyrus and decreased cerebellar volumes.8 TTM is frequently associated with other pathomimic behaviours such as nail biting (onychophagia), picking skin at pimples, picking the nose, biting lips, and chewing cheeks.9 Hair pulling may or may not be done with full awareness. This behaviour can also be obvious while the patient is engaged in other activities such as watching television, studying, and conversing. It is also prevalent during panic episodes and anxiety. Chronic pulling may lead to permanent hair loss and secondary bacterial infections. A trichoscopy and skin biopsy, along with a detailed and accurate history, can help to differentiate the disease from other types of alopecia such as alopecia areata, telogen effluvium, and androgenic alopecia, as well as fungal infections. A biopsy can reveal a high number of catagen and telogen hairs (due to chronic pulling), with no signs of inflammation, dystrophic fractured hair shafts, melanin and keratin casts, plugging of dilated hair follicles, perifollicular haemorrhage, and a relatively normal dermis.
OCD is a common psychiatric health problem in which a person experiences unwanted urges and intrusive thoughts, and uses repetitive behaviours to temporarily relieve these feelings, which are unpleasant due to the anxiety caused by these uncontrollable thoughts. It can affect people of all ages and of any sex. Many patients experience symptoms as early as puberty. OCD is distressing, disrupts daily life, and can be a social stigma. On the other hand, long-term monitoring and treatment can help keep the disease under control.
A trichobezoar is a mass of hair that accumulates in the gastrointestinal tract. Baudomant described the first case in the literature in 1779, and Schonbern conducted the first surgical removal in 1883. In ‘Rapunzel syndrome’, the foreign material extends through the pylorus into the small intestine, which may lead to significant complications.10 Gastrointestinal trichobezoars are rare, making up about 6% of all bezoars.11 It is frequently seen in adolescent females with psychiatric or intellectual disabilities, neglect, depression, anxiety, and emotional or family stress.12 A gastric endoscopy can detect this uncommon consequence in less than 1% of all individuals with nonspecific abdominal symptoms. Phytobezoars (vegetables), pharmacobezoars (drugs), and trichobezoars (hair) are the three main categories of bezoars.13
The treatment is largely psychological. The dermatologist can prescribe shampoos and serums to help with hair growth and loss, as well as topical mild steroids to reduce inflammation if it is present. Also included is the correction of any nutritional deficiencies that may exist. Habit reversal training and cognitive behavioural therapy are commonly prescribed in psychiatric treatment programmes for TTM. The following are the components of habit reversal therapy: first, the patient should be taught to be aware of their actions (hair pulling). Then, the patient should force themselves to resist the urge to pull their hair and instead engage in other activities. The final component is social support from close friends and family, which encourages the patient to persevere. Selected serotonin reuptake inhibitors have been shown to be effective in recent research. More recent data showed that olanzapine and quetiapine had some beneficial effects.14 Furthermore, management with N-acetylcysteine produced favourable results.14
CONCLUSION
This intriguing and unusual case highlights a number of critical and underappreciated clinical facts. Unfortunately, the link between psychocutaneous disorders and surgical emergencies has been grossly underappreciated. An increased understanding of psychological disorders and their dermatological manifestations, particularly in children and teenagers, can aid in the early detection of TTM and trichophagia, as well as the prevention of serious life-threatening complications such as trichobezoar.
Trichobezoar should be considered as an uncommon differential diagnosis in children and teenagers, with or without a clear history of TTM and trichophagia, and regardless of family history of psychiatric disorders.
A multidisciplinary team approach involving dermatologists, psychiatrists, and general surgeons is critical for proper diagnosis and management, resulting in better patient outcomes. Furthermore, one of the most important methods for improving understanding and management of this complex entity is education of family members. Long-term follow-up is recommended as a routine part of treatment.






