Meeting Summary
This symposium took place during the 28th congress of the European Academy of Dermatology and Venereology (EADV). Dr Seité began the meeting by emphasising the rising incidence of allergy, and the societal and economic impact this has in Europe. This was followed by the presentation of a worldwide epidemiology study conducted this year, which found that 20–42% of the population in the countries surveyed reported being affected by allergies, most commonly skin allergies followed by respiratory and food allergies. Of these individuals, 48–89% in each country experienced skin reactions, and these were treated primarily with oral or topical medication. Dr Lazic Strugar introduced the skin barrier as the first interface between the environment and the immune system, and she explained that its disruption can lead to immune dysfunction, resulting in dermatitis, skin infections, and allergies. Skincare products such as emollients can provide moisture and lipids, supporting bacterial diversity in the microbiome and restoration of the skin barrier. Dr Seité followed up with a report of a recent observational study investigating the benefits of a facial moisturiser designed specifically for sensitive skin and individuals with allergies. In this study, patients with allergies experiencing skin reactions used the product for up to 1 month, in addition to taking antihistamines alone or in combination with steroids. After 4.9 days, all subjects felt their symptoms had improved, and after the full month of treatment, both cutaneous clinical signs and subjective signs had significantly improved in most participants (>95% and 90%, respectively). Dr Seité concluded the meeting by stressing that dermatologists have an important role to play to help patients with allergies to manage their skin reactions.
Improving the Understanding of Allergy Worldwide
Doctor Sophie Seité
Allergies represent a significant, rising health concern. Recent figures indicate that 150 million Europeans experience chronic allergic disease, which includes 100 million with allergic rhinitis, 70 million with asthma, and 7 million with food allergies (some individuals have >1 allergic disease).1 It has been estimated that by 2025, 50% of Europeans will be affected by an allergy; when we consider that 45% of allergic patients are likely to be misdiagnosed in the European Union (EU) and that 8% of food allergies produce acute anaphylaxis and are potentially fatal, it is clear that allergies have a huge societal and economic impact.1
Allergies place a considerable burden on daily life and productivity: asthma and allergic rhinitis alone are estimated to result in >100 million lost workdays and missed school days in Europe every year.1 Appropriate, easily available, cost-effective treatments have the potential to produce an average saving of €142 billion per annum.1
To improve our understanding of allergy, a worldwide epidemiological study was conducted in early 2019, across 5 countries including 11,069 adult subjects.2-5 This survey was conducted with representative samples (gender, age, socioprofessional status, and regional distribution) from the general population of France (n=2,036) (La Roche Posay, data on file), Russia (n=2,010),3 Brazil (n=2,003),2 China (n=3,010),4 and the USA (n=2,010).5
Of the surveyed population, 20–42% reported having allergies, which extrapolates to 650 million people across these 5 countries. Over 60% of these individuals had been diagnosed by at least 1 physician. Considering the six main allergy symptoms, allergic rhinitis and eczema/atopic dermatitis were the most commonly reported in most countries, with the incidence of asthma, conjunctivitis, bronchitis, and oedema varying between countries (Figure 1). Types of allergies included skin, respiratory, and food, the most common of which were skin allergies. Respiratory allergies were less common in Russia and China compared to other countries.2-5
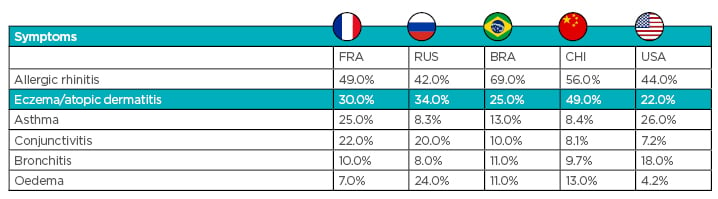
Figure 1: Symptoms associated with allergies per country. Figures represent the percentage of allergic respondents who identified this as a symptom.2-5
BRA: Brazil; CHI: China; FRA: France; RUS: Russia. Data sourced from Seite S, Taieb C et al.;2 Seite S, Taieb C et al.;3 Seite S et al.;4 Seite S et al.;5 and La Roche Posay (data on file).
Pollen was the most common type of allergen reported in France, China, and the USA, with house dust mites and mould more common in Brazil, and food and pollen equally common in Russia.2-5
High numbers of respondents reported skin reactions (48–89% of respondents per country), with the highest incidence in China.2-5 Treatment across all five countries tended to be topical, followed by oral medication.2-5 All countries were less likely to treat skin reactions with dermocosmetics than topical or oral medication, particularly the USA (14% of respondents) (Figure 2).2-5 The high level of skin reactions in allergic patients is an opportunity for dermatologists to intervene, and the underutilisation of dermocosmetics is an opportunity for the development of targeted skincare.
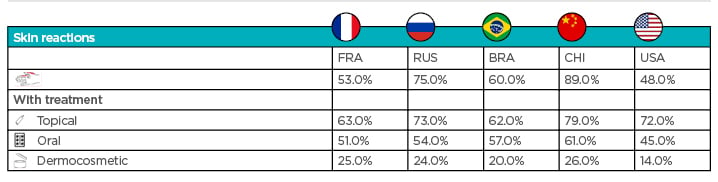
Figure 2: Skin reaction incidence and treatment by country. Figures represent the percentage of allergic respondents who reported skin reactions and treatments for the condition.
RA: Brazil; CHI: China; FRA: France; RUS: Russia. Data sourced from Seite S, Taieb C et al.;2 Seite S, Taieb C et al.;3 Seite S et al.;4 Seite S et al.;5 and La Roche Posay (data on file).
Allergic skin reactions can be managed in several different ways, depending on the type, cause, and severity of the allergy. Management can include allergen or irritant avoidance (for example by avoiding chlorinated water and irritating fabrics), restoration of the skin barrier by bathing daily with mild soap and applying fragrance-free moisturisers, application of topical immunomodulators (such as steroids, alitretinoin,6 tacrolimus,7 or pimecrolimus creams7), systemic immunosuppressants, and antifungal therapies.8
Many of these therapies are associated with side effects, and the British Association of Dermatologists (BAD) recommends that improved skincare products are considered for prevention of occupational dermatitis, and that research should be conducted in development of dedicated products to repair the skin barrier.6
Skin Barrier Dysfunction, Allergic Sensitisation, and the Role of Moisturisers in Repairing the Skin Barrier
Doctor Tamara Lazic Strugar
Allergies are becoming more prevalent across the globe and can be linked to several skin diseases. While the cause of this rise is not entirely clear, it has been attributed to factors such as stress, use of antibiotics, poor nutrition, growing up in clean and urban homes (the ‘hygiene hypothesis’), and exposure to environmental pollution.9
The skin barrier is the first interface between the environment and the immune system. This skin interface is constantly exposed to factors such as pollution, ultraviolet radiation, and harsh skincare products.9 There are four different functional layers to the skin barrier: the microbiome layer (micro-organisms on the skin); the chemical layer, including natural moisturising factor, lipids, β-defensins, and cathelicidins; the physical layer, including corneocytes, lipids, keratinocytes, and tight junctions; and the immunologic layer, including antigen presenting cells, innate lymphoid cells, and memory cells.9 All four layers need to work in harmony for the skin barrier to function correctly and if one layer becomes disrupted due to external or internal factors, this can lead to a domino-like effect resulting in immune dysfunction.9
It has been known for some time that the skin barrier plays a critical role, not only in retaining water, but in excluding allergens, irritants, and pathogens that have the potential to disrupt the immune system, causing allergic sensitisation.9 Disruption of the immune system in the skin can lead to inflammatory diseases such as atopic and contact dermatitis, skin infections, and allergies. Recent data have suggested that food allergies develop via transcutaneous sensitisation in infancy.10 There will likely be a primary barrier deficiency in at least some individuals with sensitive skin. Skincare products such as emollients can provide moisture and lipids, supporting bacterial diversity in the microbiome and restoration of the skin barrier.9 Maintaining or regaining a healthy skin barrier is critical for the management of chronic inflammatory diseases. Dermatologists play an important role in the treatment and prevention of these conditions by counselling patients on the proper use of skincare products.
The Role of Dermocosmetics in Managing Skin Reactions in Allergic Subjects
Doctor Sophie Seité
Originally developed to enhance personal appearance, cosmetics have taken on a new role in dermatology because of an increasing understanding of how they can modify the physical and biological properties of the skin, and they are now part of the management of a number of skin disorders.11 Dermocosmetics, alone or in combination with medications, are used to improve dry skin, acne, atopic dermatitis, rosacea, seborrhoeic dermatitis, and psoriasis, enhancing quality of life and reducing side effects associated with some treatments.11 Because of this, trials evaluating cosmetics are now expected to adhere to rules comparable to those used for pharmaceutical product trials.11
An observational study was recently conducted in Russia to investigate the use of a face moisturiser (Toleriane Ultra; La Roche-Posay, Poitou-Charentes, France) on facial skin reactions in patients with allergies consulting an allergist (La Roche Posay, data on file). The product studied was designed specifically for sensitive skin and individuals with allergies, and works by reinforcing the skin barrier and decreasing skin reactivity.12
A total of 1,932 subjects with allergies were included in the analysis during consultation with allergists (n=200). The mean age was 36 years (range: 15–65), and most subjects were women (90.3%). Most subjects were affected by respiratory allergies (92.0%). All subjects showed skin reactions on the face (>90.0% on the eyes), and many on the hands (73.3%) (Figure 3). All subjects were being treated with antihistamines, and concomitant corticosteroids in 50.0% of cases. During the study, subjects applied the skincare product to affected areas until skin reactions were alleviated.
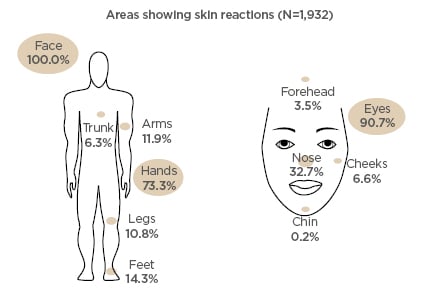
Figure 3: Location of skin reactions in subjects at baseline.
After 4.9 days of treatment, 100.0% of subjects felt their symptoms had improved. At the end of the study, skin reactions (erythema, dryness, oedema, desquamation, and pruritus) were significantly improved in >95% of subjects, and subjective signs (itching, burning, and tingling) had significantly improved in >90% of subjects. Both allergists and patients considered tolerance of the product was good to excellent in 97% of cases. Many allergists (85–100% depending on the type of allergy) felt that the product was effective against allergy-related cutaneous reactions (excluding metal allergy). All patients in the study were satisfied with the product. In conclusion, this study supports the use of skincare products, specifically formulated and tested for allergic individuals, as part of a treatment strategy for skin reactions. It is clear that dermatologists have an important role to play in order to help patients manage their skin reactions associated with allergies.







