Meeting Summary
The importance of discussions around the management of women of childbearing age with psoriasis, an issue that has been largely neglected for many years, was introduced and emphasised by Prof Ryan as the topic for this symposium. The changing needs and hurdles faced by this patient population due to the different hormonal phases throughout a woman’s reproductive life can reduce quality of life (QoL), aggravate disease burden, and complicate treatment decisions. This was exemplified by Dr Kleyn using three case studies for which delegates provided useful insights on management options. It was noted that fears and misconceptions often result in women of childbearing age delaying the decision to start a family and that improved doctor–patient interactions are key to helping women overcome concerns surrounding conception and pregnancy.
Prof Augustin discussed the significant impact of psoriasis on physical and psychological comorbidities and stigmatisation using the concept of cumulative life-course impairment (CLCI) as a measure. He then presented clinical trial data on anti-TNF biologic therapy during pregnancy, with a particular focus on results relating to placental transfer and transfer into breast milk. The delegates’ opinions on family planning and postpartum flares were then sought for three relevant clinical scenarios illustrated by Prof Ryan. The use of anti-TNF agents in women who are actively trying to conceive, are pregnant, or are breastfeeding was discussed, with the majority of delegates indicating that they would recommend anti-TNF treatment to patients where appropriate. The lack of practical guidance in dermatology the management of women of childbearing age with psoriasis was highlighted, and the symposium concluded with an overview of current recommendations by the European League Against Rheumatism (EULAR) for patients with rheumatological conditions. These emphasise the importance of discussing family planning with female patients and directly involving them in treatment decisions to optimise their reproductive journey.
The Imprint of Psoriasis on the Patient’s Life
Professor Caitriona Ryan
A characteristic feature of psoriasis is that it affects all aspects of a patient’s life.1,2 It typically develops during the teenage years, when major decisions regarding relationships and careers are made and, therefore, the cumulative impact on social, emotional, and work life can be substantial, with negative effects on the individual’s ability to achieve their full potential.1,2 Furthermore, each patient is affected in a unique way by the condition, with constantly changing needs that may complicate treatment decisions.1,2
The major impact of psoriasis on both QoL and physical and mental health has been amply demonstrated in a USA-based study of data collected from 2003–2011 from >5,600 patients with psoriasis or psoriatic arthritis.3 Each measure of emotional burden, including self-consciousness, embarrassment, and frustration, was reported by nearly 90% of respondents.3 Physical symptoms, namely itching and pain, were reported by 93% and 83% of patients, respectively.3
Interestingly, there is evidence of a differential impact of psoriasis across sexes. An observational study of 2,450 patients found that, compared with men, women generally scored higher on subjective but not objective disease activity measures, indicating a greater experienced disease burden and worse QoL, potentially as a result of undertreatment.4 More women than men (37.7% versus 27.7%) had Dermatology Life Quality Index (DLQI) scores >10, but more men than women (35.3% versus 27.0%) had a high (>10) Psoriasis Area Severity Index (PASI).4 Of the patients receiving biologic therapy, the majority were men (67.1%).4
Hawro et al.5 demonstrated that women with psoriasis are also more likely than men to experience feelings of stigmatisation (e.g., anticipation of rejection, feelings of being flawed, sensitivity to others’ opinions; p=0.05, p=0.002, and p<0.001, respectively). This is important because stigmatisation is the strongest predictor of reduced QoL and depressive symptoms in psoriasis.5,6
The impact of psoriasis in women versus men is exacerbated by genital symptoms. In a study of 354 men and women with the disease, 63% had current or previous history of genital manifestations, such as burning, itching, pain, and stinging.7 These were reported more frequently by women, with a statistically significant difference for pain, burning, and discomfort during intercourse.7
Additionally, the course and risk of psoriasis can be affected by hormonal factors during puberty, pregnancy, and menopause.8,9 For example, there is evidence that in some patients, symptoms improve during pregnancy when oestrogen levels increase, and there is also evidence that the majority of women experience a worsening of symptoms soon after childbirth.8,9 In terms of psoriasis risk, a prospective analysis of 163,763 women concluded that those with irregular menstrual cycles or surgical menopause were more likely to develop the disease than women with regular cycles and natural menopause (multivariate hazard ratio [HR]: 1.32; 95% confidence interval [CI]: 1.01–1.73 and HR: 1.19; 95% CI: 1.01–1.40, respectively).10 By contrast, the risk was lower in women who had multiple births (≥2) or a breastfeeding duration ≥24 months than in women who had one birth or who had not breastfed (HR: 0.85; 95% CI: 0.71–1.01 and HR: 0.69; 95% CI: 0.51–0.93, respectively).10
Stories in Psoriasis: Exploring the Hurdles Encountered on the Road
Doctor Elise Kleyn
Three case studies were used to exemplify the impact of psoriasis on female patients (Box 1).
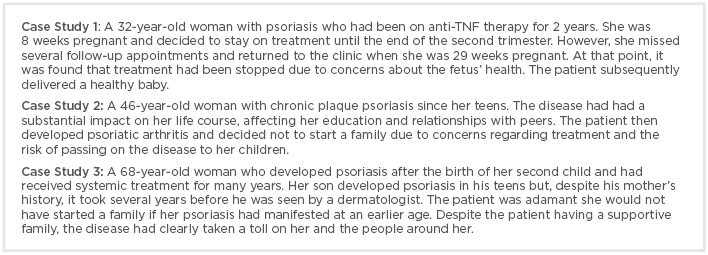
Box 1: Case studies demonstrating the impact of psoriasis on women.
A common theme emerging from the discussion of these case studies was that women of childbearing age with psoriasis often delay the decision to become a mother or abandon the idea altogether. Studies in patients with other chronic inflammatory conditions have shed light on the concerns and misconceptions behind such decisions. In one of these studies, 54% of women (n=622) aged 18–45 years living with rheumatic disease reported delaying their decision to start a family.11 The most frequently given reasons included fear of passing on the disease to the baby (46%), concerns about not being healthy enough to conceive and carry a child to term (23%), and not being emotionally ready to become a mother (19%).11 Additionally, and importantly, 10% of the women who admitted delaying the decision to start a family also reported a lack of support from their family physician.11
With regard to the actual genetic risk of passing on psoriasis to the offspring, it is worth noting that there is a 50% chance if both parents have psoriasis but a 16% and 8% chance if only one parent or neither parent, respectively, has the condition; there is also no evidence that psoriasis causes disease-specific defects in newborns.12 In terms of the ability to conceive and carry a child to term, research suggests that young women (<35 years) with psoriasis have a 22% lower pregnancy rate and 39% lower live birth rate compared to women without the condition.13
Of note, an estimated 50% of pregnancies in the USA are unplanned.13 While a good patient– physician relationship would be desirable, especially in the context of family planning, evidence suggests this is less than optimal at present. In a survey of 300 patients with psoriasis in Italy, >50% of participants emphasised that physicians should listen to their needs.14 Frequently reported desirable physician qualities included the ability to communicate in a simple language and convey feelings of control and hope about the curability of psoriasis.14
Beckman and Frankel15 published detailed data on the state of the patient–physician relationship. They found that patients are generally able to express their concerns in only 23% of office visits; the most common reason for this was interruptions by the physician, which were reported in 69% of office visits. The amount of time physicians spend listening to patients before taking the lead is a mean of 23.1 seconds, according to other research.16 However, data have suggested that just 2 minutes of physician listening would be enough for approximately 80% of patients.17 There is clearly a requirement among doctors for greater awareness of their patients’ needs and of ways to improve their relationships with them.
Avoiding the Obstacles Along the Way: From Puberty, Through Pregnancy, to Menopause
Professor Matthias Augustin
In his introductory overview on treatment- related needs in patients with psoriasis, Prof Augustin quoted the results of German registry data analyses,18,19 which showed that the most frequently reported needs are rapid improvements in skin appearance (93%) and healing of all skin defects (91%) (unpublished data). These results are somewhat expected given the nature of the disease and that such improvements would be straightforward to measure with PASI. However, the same analyses identified a broad range of other needs in all different aspects of life, including the need to be able to lead a normal life, feel less depressed, and be free of pain.
Additionally, it is evident that treatment-related needs differ across age groups and sexes. For example, compared with patients aged ≥65 years, those <65 years are more likely to report the need to be able to work and have a normal sex life.20 Needs such as feeling less depressed, sleeping better, and being more productive are more prevalent among women than men.
It is crucial to be able to identify and measure needs in different patient populations to be able to optimise treatment,20 and young women of reproductive age were perceived by the audience to be among those with the highest needs. The CLCI concept is useful in this regard because it measures the cumulative burden of psoriasis over a patient’s lifetime rather than at certain points in time.21 Specifically, it is possible to calculate for each patient a CLCI score that captures the effects of the condition over time in terms of its impact on physical comorbidities (e.g., psoriatic arthritis), psychological comorbidities (e.g., depression and anxiety), and stigmatisation (e.g., public rejection and self-image).21 The CLCI is influenced by coping strategies and factors, such as treatments and support from family and healthcare professionals. Tailoring these to the needs of the individual patient can help mitigate or reverse the burden of psoriasis.
Members of the audience noted the importance of early intervention to prevent the disease from having a cumulative effect on patients. It was highlighted that establishing good patient–doctor relationships has the potential to modify the trajectory of the life course of patients, empowering them to achieve their full potential.
Since psoriasis develops by 16 years of age in approximately 30% of patients,8 it is often already present during puberty. An analysis of data from 33,981 patients in Germany in 2005 found that those aged 0–20 years had double the comorbidity rate of subjects without the condition.22 More specifically, children and adolescents with psoriasis had increased rates of high cholesterol (2.12% versus 0.99%), obesity (8.40% versus 4.90%), hypertension (1.65% versus 0.83%), diabetes (0.86% versus 0.43%), rheumatoid arthritis (8.40% versus 4.90%), and Crohn’s disease (0.51% versus 0.14%).22 These results clearly indicate that comorbidities are also important to consider in patients with psoriasis.
Pregnancy can be a particularly vulnerable time for psoriasis patients. It has has been reported to be a trigger for the onset of psoriatic arthritis after childbirth in 30–40% of women.23 Furthermore, although an estimated 55.3% of women with psoriasis report symptomatic improvement during pregnancy, 65.2% experience substantial worsening soon after giving birth.9 An important implication of these findings is that adequate treatment in women of childbearing age with psoriasis is crucial. However, despite therapies being available, their use during pregnancy remains suboptimal.
Current therapies include topical treatments (e.g., mild corticosteroids), systemic drugs (e.g., cyclosporine), and biologics (e.g., anti-TNF agents). With regard to anti-TNF agents specifically, Marchioni and Lichtenstein24 conducted a systematic review of studies reporting on birth outcomes following maternal exposure to infliximab (IFX), adalimumab (ADA), or certolizumab pegol (CZP). They concluded that, although these therapies are promising, the benefits demonstrated in clinical trials must be weighed against the potential risks for the baby. When comparing the three agents in terms of their presence in newborns and the umbilical cord on the day of birth, IFX and ADA, but not CZP, were found to have higher concentrations than in the mothers.25 This was observed in a USA-based study of pregnant women (N=31) with inflammatory bowel disease (IBD).25 At birth, the median levels of IFX, ADA, and CZP in the umbilical cord were 160.0%, 153.0%, and 3.9% those of the mother, respectively.25 Although no serious congenital effects were reported, IFX and ADA were still present in the babies up to 6 months after their birth.25
The aforementioned results for CZP are corroborated by those reported by Mariette et al.26 in the CRIB study. This was a prospective, post-marketing, pharmacokinetic study of pregnant women (N=16) with autoimmune diseases, including rheumatoid arthritis, axial spondyloarthritis, psoriatic arthritis, and Crohn’s disease. It used blood sampling of mothers at delivery and of newborns and cords at delivery and 4 and 8 weeks after birth. Data for 14 mother–newborn pairs showed that blood CZP levels were within the expected therapeutic range in mothers at delivery (median [range]: 24.4 [5.0–49.4] μg/mL) and were below the level of quantification (0.032 µg/mL) in 13 out of the 14 babies at birth and in call baby samples at Week 4 and 8, indicating a lack of or minimal placental transfer during pregnancy.
Exposure to anti-TNF agents during pregnancy has an impact on immune system development in newborns. Recent research revealed that newborns of mothers with IBD who received IFX or ADA throughout pregnancy had a less mature immune system at the age of 6 months compared with healthy controls.27 The effect was no longer observed by 12 months of age;27 nonetheless, this result must be considered in terms of vaccine recommendations. EULAR advises delaying the use of live vaccines by 6 months in newborns exposed to biologic therapy during the late-second and third trimester of pregnancy.28 It also recommends that paediatricians should be informed of whether and when the mother received biologic therapy during treatment of their psoriasis.
Transfer of anti-TNF agents into breast milk has also been investigated. In two studies by Ben-Horin et al.,29,30 mothers exposed to IFX or ADA had detectable levels of the biologics in their breast milk. In nursing women (n=3) with IBD, IFX increased 12 hours after the first infusion, peaked at 90–105 ng/mL within 2–3 days, and plateaued thereafter.29 In one nursing woman with Crohn’s ileitis, ADA levels in milk reached 31 ng/mL within 6 days of the first infusion and declined thereafter.30 No relevant breast milk CZP concentrations were detected in a study of patients with chronic inflammatory diseases, including rheumatoid arthritis, psoriatic arthritis, and Crohn’s disease. All milk samples (N=137) collected from 17 nursing mothers were below the lower level of quantification (max: 0.076 µg/mL) and 56% had no measurable CZP.31
The audience were asked whether, based on the data presented, they would recommend patients with moderate-to-severe psoriasis who are trying to conceive or are pregnant to discontinue anti-TNF therapy. The majority said they would advise their patients to continue treatment. However, it was emphasised that this should be an informed decision made by the patient after discussions around the potential for placental transfer of anti-TNF agents.
Nurturing the Woman Through the Psoriasis Journey: From Burden to Empowerment
Professor Caitriona Ryan
The symposium continued with a panel discussion on ways to enable women of childbearing age with psoriasis to feel empowered to make decisions about family planning and pregnancy. The members of the panel were first invited to share their experience regarding the best time to introduce family planning to their patients. The majority indicated that this is generally at treatment initiation. This was considered important given the high rates of unplanned pregnancies. For example, in the USA alone an estimated 50% of all pregnancies are unplanned.13
Three additional clinical scenarios were then presented. The first was that of a 30-year-old woman whose psoriasis has had a significant impact on her life, resulting in a loss of confidence. The patient was stable on anti-TNF therapy and leading a normal life. She presented to the clinic to discuss her plan to start a family since she was concerned about discontinuing treatment and having her psoriasis uncontrolled.
The audience highlighted the importance of reaching a shared decision with the patient to remain on anti-TNF therapy. Discussions about lifestyle were said to be crucial because patients with psoriasis are often overweight, with comorbidities, including depression, that can potentially affect adherence to treatment. Education on the impact of psoriasis on fertility was also recommended. For example, there is little awareness that untreated psoriasis can impair fertility in males aged 18–55 years;32 however, the time to pregnancy >5 months is not increased in women with psoriasis versus those without.33
The second clinical scenario was a 24-year-old woman with psoriasis and psoriatic arthritis (PASI: 7.8; body surface area [BSA]: 8.0%; DLQI: 24). Currently on ADA plus methotrexate symptomatic treatment, she returned to the clinic for a regular follow-up appointment. Discussions with the patient about the potential for teratogenic effects of methotrexate and the need for contraception were said to be paramount. Identifying and addressing factors other than skin issues (e.g., depression) that may be responsible for the high DLQI, despite relatively low PASI and BSA, were also indicated as important.
For the third clinical scenario, the audience was asked to consider a 35-year-old woman with psoriasis 6 weeks after giving birth (BSA: 40%; DLQI: 27). The patient discontinued anti-TNF treatment after becoming pregnant and had postpartum flares but wanted to continue to breastfeed. There was consensus that treatment should be resumed and that, based on the data presented, in particular for CZP, biologic therapy can coexist with breastfeeding.
The audience was then asked whether they would initiate or delay anti-TNF therapy or recommend another systemic agent for a woman with severe psoriasis who is breastfeeding. Seventy percent said they would initiate treatment with an anti-TNF agent, 15% said they would delay therapy, and the remaining 15% said they would use a different systemic agent. On the last point, it was noted that the only feasible systemic alternative would be cyclosporine. However, this transfers into breast milk in elevated amounts and, therefore, regular monitoring of the baby would be required if cyclosporine was administered.
Smoothing the Patient’s Journey Towards Better Outcomes in Psoriasis
Professor Caitriona Ryan
When asked what strategies may help lessen the CLCI of psoriasis in women of reproductive age, the audience agreed on the need to inform patients about therapy options and encourage them to use available treatments. Recommended strategies also included providing reassurance that the potential risks of life-long treatment are minimal in most cases, establishing a relationship of trust and collaboration with the patient, asking them what they hope to gain from the therapy, being positive about disease outcomes, and discussing the risks and benefits of each treatment option. Early intervention was said to be crucial to improving outcomes in psoriasis.
The opinion of the audience was sought on whether they felt comfortable prescribing anti-TNF therapy for women with psoriasis who are trying to conceive or pregnant. Overall, 80% reported being comfortable with prescribing anti-TNF therapy for women who are trying to conceive, compared with 64% for women who are pregnant, based on the presentation.
Research has been conducted recently on the level of comfort among dermatologists in Europe and the USA with prescribing anti-TNF therapy for women of childbearing age with chronic inflammatory disease.34 The findings showed that more European than North American dermatologists believed that anti-TNF therapy should be avoided during breastfeeding and discontinued before conception and during pregnancy.34 Overall, 54% and 83% of dermatologists in Europe and the USA, respectively, said they were comfortable with prescribing anti-TNF agents to female patients of childbearing age; 10% and 21%, respectively, said they were comfortable with prescribing during pregnancy.34 Of note, only 15% of surveyed dermatologists in Europe and the USA strongly agreed that keeping the disease controlled was their primary goal; in addition, 23% and 48%, respectively, admitted being very concerned about adverse events when prescribing anti-TNF therapy to pregnant women with chronic inflammatory disease.34
Conclusion
For women of reproductive age with psoriasis, navigating the road to disease control can be challenging since symptom severity may fluctuate or be influenced by the different hormonal phases experienced throughout life. In addition, concerns surrounding pregnancy and breastfeeding often result in patients delaying the decision to start a family. Biologic therapies have demonstrated the ability to reduce the burden of psoriasis. Through careful evaluation of the risks and benefits of treatment, and the implementation of multidisciplinary management strategies and shared decision-making, dermatologists can empower women to change the trajectory of their life’s course and progress through their reproductive journey with confidence.
Click here to watch the full symposium and access related resources online.







