Meeting Summary
During this symposium, global experts in dermatology gave a series of lectures focused on skin treatments and their benefits for patients. Giuseppe Micali, University of Catania, Italy, provided a non-invasive skin imaging perspective on the skin journey over time, exploring the changes in the functional integrity of ageing skin, and associated dermatological needs. Positive findings from a clinical study evaluating U-Life™ 10 (Relife Menarini Group, Florence, Italy), a 10% urea cream, in the treatment of senile xerosis were also presented. The second lecture, presented by Giovanni Pellacani, Sapienza University, Rome, Italy, reviewed the pathogenesis of eczema, and the key role of oxidation in skin barrier impairment and inflammation. A recent study evaluating the clinical performance of Relizema™ cream (Menarini Group), a steroid-free medical device, for topical use demonstrated that it effectively reduced the severity of symptoms in adults with atopic and contact dermatitis, and was well-tolerated. The final presentation by Micali focused on salicylic acid-based products containing active ingredients that target multiple pathogenetic factors of acne. Findings from a multicentre, prospective, observational study of this new salicylic acid-based acne daily regimen showed promising improvements in patients with mild acne.
The Skin Journey Over Time: Changes in the Functional Integrity of Ageing Skin and Dermatological Needs. A Non-invasive Skin Imaging Perspective
Giuseppe Micali
Micali began by outlining the processes of intrinsic (chronological) ageing and extrinsic ageing (photoageing), both of which can combine to increase the risk of photocarcinogenesis, and provided images in support of the key characteristics of skin ageing.
Intrinsic or chronological ageing is a natural process characterised by skin thinning, pigmentation, laxity, fine wrinkles, xerosis, and seborrhoeic keratoses (also known as cherry angiomas). It is influenced by factors such as ethnicity, anatomical variations, and hormonal changes.1 At the underlying histopathological level, key differences can be seen between ‘young’ and ‘old’ skin. During intrinsic ageing in young skin, flattening of the dermal-epidermal junction occurs; the rate of epidermal turnover halves; and there is a decrease in sebaceous production, leading to xerosis. Other changes include a reduction in epidermal filaggrin, an increase in transepidermal water loss, and an approximate drop of 20% in the number of melanocytes, resulting in a paler skin appearance. In old skin, in the dermis itself, there is decreased synthesis and increased degradation of collagen, which can impair the wound healing process. Elasticity is also reduced as elastic fibres decrease in both number and size. Dermal bulk and accumulation of lipofuscin in the ageing skin contribute to wrinkling, and skin turgor is negatively impacted by age-related changes in mucopolysaccharide levels.1
In contrast to the natural chronological ageing process, photoageing of the skin is triggered by extrinsic exposure to ultraviolet (UV) radiation. Key characteristics include thick, dry, and rough skin; deep wrinkles; actinic keratoses; irregular freckling/lentigines/guttate hypomelanosis; telangiectasias; comedones (Favre–Racouchot syndrome); Milian’s citrine skin; and cutis rhomboidalis nuchae (Jadassohn).1 When we talk about extrinsic factors related to photoageing, we refer to the phototype, the degree, and the extent of UV exposure and lifestyle factors, such as smoking.1 Micali reiterated that both chronological ageing and photoageing may result in photocarcinogenesis, subtypes of which include actinic keratosis, squamous cell carcinoma, and basal cell carcinoma.
Micali then went on to review some of the main techniques employed in the non-invasive imaging of skin ageing. Dermoscopy and videodermatoscopy, affording magnifications of x10 and x100, respectively, are useful in the evaluation of xerosis in intrinsic ageing, and for monitoring the effect of treatments (e.g., emollients) on the skin. In photoageing, dermoscopy/videodermatoscopy are valuable tools for the diagnosis of pigmented lesions, and, in particular, the differentiation of benign versus malignant lesions. Important differences were observed through dermoscopy and videodermatoscopy between the baseline and after emollient treatment, notably the disappearance of scales.
High-frequency ultrasound, which provides axial resolution in the range 16–80 mm and lateral resolution between 32–200 mm, is another technique which can be used to visualise and quantify age-related dermal changes, allowing for high-resolution imaging of the skin from the stratum corneum to the deep fascia. The subepidermal low-echogenic band (SLEB), visualisable on high-frequency ultrasound, represents a key marker of photoageing that appears to be related to dermal elastosis and basophilic degradation of collagen, as well as accumulation of glycosaminoglycans and water in the papillary dermis. Assessment by high frequency ultrasound has shown that the SLEB grade is higher in sun-exposed skin as compared to sun-protected skin.2 Normalisation of SLEB has also provided objective data on the impact of mesotherapy for skin rejuvenation.2
Another sophisticated and non-invasive technique for skin imaging is VISIA-CR (Canfield, Parsippany, New Jersey, USA), the advanced digital imaging system that produces high quality, reproducible facial images. Photographs are taken, positioning the head of the subject in a standard position, and multiple lightening modes can be applied, including standard light, UV light, and cross-polarised light, each of which provides a different visual perspective on skin ageing. Standard light analyses texture, wrinkles, and pores. In the UV light mode, UV spot reveals underlying photodamage by providing a sensitive evaluation of epidermal melanin distribution, which appear as dark spots, and dermal changes in collagen and elastin fibres, which appear as light areas. In the cross-polarised light mode, brown spot provides an effective evaluation of dermal melanin, while red areas enable a clear visualisation of vascular patterns. Advanced digital photography also plays a key role in assessing the effects of anti-ageing therapy, with a positive impact seen from treatments, such as chemical peel and mesotherapy.
Reflectance confocal microscopy is a diagnostic technique used in the evaluation of intrinsic ageing, which enables a real-time, non-invasive, cytological, and architectural study of the skin at histological resolution. Xerotic skin shows the presence of medium-to-large-sized furrows, and bright amorphous structures related to microscales and detached keratinocytes in the stratum corneum. Reflectance confocal microscopy is a useful technique for treatment monitoring that shows how, with emollient therapy, there is a normalisation of skin furrow size and morphology.3
The final non-invasive skin imaging technology reviewed was line-field confocal optical coherence tomography, which Micali described as a ”revolutionary system” for evaluating intrinsic skin ageing, that can measure thickness of the epidermis, and evaluate changes after anti-ageing treatment. Line-field confocal optical coherence tomography employs a new technology, the high-resolution supercontinuum laser (600–900 nm), which delivers real-time navigation within a skin volume of 1,200x500x500 μm from the skin surface to the dermis, thereby achieving the effect of a ‘virtual biopsy’.4
For the concluding part of this lecture, Micali presented results from an open-label clinical study that evaluated the efficacy and tolerability of U-Life™ 10, a 10% urea cream, for the treatment of senile xerosis.5 This study included 20 patients, ranging in age from 65–82 years, who were affected by moderate-to-severe xerosis of the upper or lower extremities. Those with a history for diabetes, or who had used topical moisturisers and/or other treatments for xerosis in the previous 30 days, were excluded from the study. U-Life™ 10 was applied twice daily for 2 weeks, and patients underwent skin assessment at baseline, 7 days, and 14 days. Efficacy assessments included: the degree of skin dryness by clinical evaluation, with a score from 0 (normal skin) to 3 (severe xerosis); degree of surface scaling by x10 dermoscopy, using a 4‐grade severity score: 0 (absent scales) to 3 (severe scales); and pruritus by visual analogue scale (VAS) from 0 (no itch) to 3 (severe itch). Scores obtained from each assessment were then totalled to achieve an overall score ranging from 0–9 for each patient. The treatment response was deemed excellent when the total score was reduced by more than 70%; good when it was reduced by 40–69%; moderate if reduced by 20–39%; and poor when reduced by less than 20%. Tolerability and cosmetic acceptability (encompassing spreadability, absorbency, odour, pleasantness, and ease of application) were also assessed at Day 14 on a 4-grade score, ranging from poor (0) to excellent (3).
All patients completed the study and scores for all key efficacy measures (clinical evaluation, dermoscopy, and VAS) showed a statistically significant improvement (p<0.05; Table 1).5 Furthermore, a correlation between clinical and dermoscopy evaluation of the skin was demonstrated using the Pearson’s test. The response to U-Life™ 10 was found to be excellent in 16 cases, and good in the remaining four cases. No side effects were recorded, and all patients gave a positive response regarding acceptability, with 14 patients judging the product as excellent, and six as good.5 In confirmation of these positive study findings, Micali also showed some real-world clinical cases of elderly patients with xerosis, where excellent responses and clinical resolution of symptoms were achieved using the 10% urea cream.
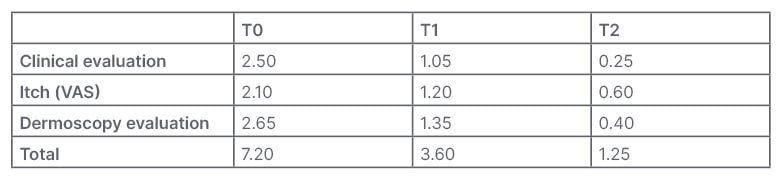
Table 1: 10% urea cream for senile xerosis: results.5
T0: baseline; T1: Day 7; T2: Day 14; VAS: visual analogue scale.
Overall, these results indicate that the tested 10% urea cream, U-Life™ 10, showed progressive clinical improvement and related pruritus in all patients, representing a promising approach in mild-to-moderate senile xerosis, Micali concluded. The 10% urea cream has proven to be well-tolerated, with no reports of stinging, burning, or other side effects, suggesting its suitability for long-term use. This is important, Micali highlighted, as contact dermatitis is common in elderly patients who will often have used multiple treatments for xerosis.
Micali concluded his presentation by highlighting the main clinical indications for urea-based topical products, noting that this is a very versatile compound that can be used at a range of concentrations. Low concentration (2–12%) products are suitable for the treatment of xerosis in ichthyosis, atopic dermatitis, and psoriasis, as well as xerosis of the elderly.6
Clinical Trial on Subjects with Dermatitis with a Steroid-Free Medical Device
Giovanni Pellacani
Eczema is a widespread skin condition, comprising a family of diseases with different presentations, including allergic and irritant contact dermatitis, atopic dermatitis, and other eczema types. Pellacani explained that the natural evolution of eczema can be separated into two phases: acute and chronic, each characterised by different histopathological patterns of cutaneous inflammation. With eczema, it is always important to keep in mind what is happening at the biological level, Pellacani stressed. The critical first stage of eczema pathogenesis is a skin barrier defect, which is characterised by alterations in lipid content, loss of natural moisturising factors, and increased barrier permeability, leading to higher transepidermal water loss and decreased hydration. Barrier damage enables antigens and irritants to penetrate the skin, which, in turn, activates inflammatory and immune system responses. A barrier defect is also seen in the chronic phase of eczema, and helps to perpetuate the inflammatory stimuli in the skin.
Pellacani emphasised that oxidation plays an important role in both the acute and chronic phases of eczema, with the generation of reactive O2 and reactive nitrogen species that overwhelm the antioxidant capabilities of cells. The oxidative state leads to skin barrier damage, and further drives inflammatory and chronic immune responses. In this way, oxidative stress generates a “vicious cycle” that keeps the disease going on, Pellacani summarised. In confirmation of the important role of oxidation, studies have shown that non-pharmacological treatments containing the antioxidant agent furfuryl palmitate are effective against the signs and symptoms of atopic dermatitis and related skin conditions.7
Emollients are the current mainstay of treatment for eczema, and are the recommended baseline therapies, alongside lifestyle measures, in consensus-based European guidelines.8 Pellacani explained that emollients should be used in abundance to keep skin hydrated, and to maintain the barrier. The European Academy of Dermatology and Venereology (EADV) guidelines also advocate liberal and frequent use of emollients, applied in a minimum amount of 250 g per week for adults.8 Non-irritant and hypoallergenic formulations of emollients are available for basic treatment, but may not be well-tolerated on damaged skin in the acute phase of eczema. Emollient plus products consist of topical formulations with vehicle and active non-drug ingredients, such as vitamins, bacterial lysate, and antioxidants, to improve skin barrier repair, improve the cutaneous environment, and reduce inflammation processes in the skin.
Having set the scene, Pellacani went on to present results from a recent open-label study, which aimed to examine the clinical performance and safety of a medical device (Relizema™ cream), containing the antioxidant furfuryl palmitate, for topical use in adults with mild-to-moderate dermatitis.9 This study enrolled 40 adults aged between 18–65 years with mild‐to‐moderate atopic or contact dermatitis (50:50 split). Relizema™ cream was applied twice daily for 28 consecutive days, and changes in disease severity from baseline were assessed on Days 14 and 28. These efficacy evaluations included Investigator’s Global Assessment (IGA) and Eczema Area and Severity Index (EASI) scores; pruritus scores; and quality of life, based on the Dermatology Life Quality Index (DLQI). Patients’ satisfaction with the product was also assessed, and global evaluation of the performance carried out.9
Figure 1 shows the changes in mean IGA score from baseline in patients treated with Relizema™ cream in this study. As Pellacani highlighted, a greater than 1-point reduction in mean IGA score was achieved after 4 weeks of product use. This means you move the disease from a range between zero (no disease) to very mild disease in most cases, Pellacani remarked. Similar results were seen with mean EASI scores, with an almost 50% reduction in EASI score by Week 2, and further improvements by Week 4 of treatment with Relizema™ cream. From a mean EASI of 4.49 at Day 1, scores were improved to 2.59 at Day 14, and 1.08 at Day 28. Pellacani explained that mean baseline EASI score was low among subjects in the study (as expected), due to the inclusion of 50% patients with contact dermatitis who tend to have limited disease, irrespective of severity. Relizema™ cream also delivered significant improvements in patients’ mean pruritis score and quality of life. From high levels of itch at the beginning of the study, mean pruritis score was reduced from 50 to around 10 by Day 28, which is equivalent to very mild pruritis, Pellacani noted. Similarly, DLQI scores improved from an average of 7 at baseline to around 2 by Day 28 of therapy.9 Overall, this study has shown that the medical device Relizema™ cream for topical use is safe, and reduces the severity of symptoms in adults with atopic and contact dermatitis, Pellacani concluded. Relizema™ cream performs the dual role of an emollient and an antioxidant, with the two agents working together to exert beneficial effects. As an emollient, it helps restore impaired barrier function in patients with eczema, thereby blocking the penetration of allergens or irritants. As an antioxidant, it helps to reduce oxidative stress within skin cells, which further combats barrier damage, and also reduces inflammation. The overall result of the combined emollient and antioxidant is an improvement in epidermal repair and skin barrier restoration, as well as a reduction of inflammation within the skin. This product, therefore, represents a good companion to your practice when treating patients with eczematous disease, Pellacani concluded.
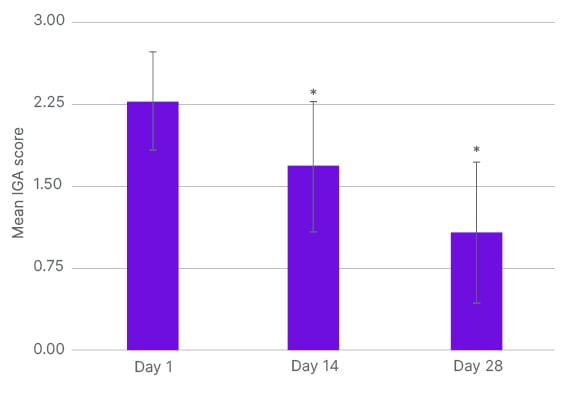
Figure 1: Relizema™ cream for dermatitis: change in mean Investigator’s Global Assessment score from baseline.9
IGA: Investigator’s Global Assessment.
Acne Multifactor Targeting Approach: Favouring Patient Compliance
Giuseppe Micali
The final lecture of the symposium shifted the focus to acne, which Micali described as a chronic inflammatory disease, most common in early adolescence (>80% of teenagers), and rare in paediatric (8–13%) or adult patients (5% female; 1% male). The underlying disease pathogenesis of acne is complex and multifactorial, but appears to be driven primarily by androgens, which act on sebocytes and keratinocytes, leading to seborrhoea and follicular desquamation, respectively. This results in alteration of follicular activity, which promotes colonisation of the culprit bacteria Cutibacterium acnes, thereby generating ongoing inflammation within the skin.10 From an epidemiological perspective, acne is most common in early adolescence, with teenagers representing over 80% of cases, and comparatively rare in adults and paediatric patients. Acne has a polymorphic clinical presentation characterised by closed/open comedones, papules, pustules, and nodules.11
Micali explained that the ideal treatment for acne should target multiple pathogenic factors, be effective with minimal side effects, limit the risk of C. acnes antibiotic resistance, and improve patient compliance, with the overall goal of achieving a positive clinical outcome. The current armamentarium for acne management consists of both topical and systemic agents, notably retinoids, antibiotics, and antimicrobials.12 Although these pharmacological agents remain the main therapeutic approach for all clinical types of acne, their use may be associated with adverse reactions. Common side effects, such as erythema, scaling, burning, and photosensitivity, can in turn have a negative impact on patient compliance and adherence to treatment.13 Teenagers especially may, therefore, ask for a mild treatment option to start. Cosmetics can, therefore, play an important role in acne treatment, and help to minimise the common side effects of systemic/topical retinoids, benzoyl peroxide, and antibiotics.14 If correctly prescribed and used, cosmetics may have a synergistic effect with pharmacological agents, and some may also be effective in mild forms of acne, Micali noted.
To this end, a recent multicentre, prospective, observational study set out to evaluate the safety and efficacy of a new salicylic-acid based acne daily regimen for the treatment of mild acne.15 This regimen consisted of three separate products, each containing salicylic acid in combination with other key acne-targeting active ingredients: PapiX™ cleanser (Relife Menarini Group) with salicylic acid (2%), urea peroxide, and glycolic acid, applied twice daily; PapiX™ long (Relife Menarini Group), a moisturising gel (medical device) of salicylic acid (2.5%), nicotinamide, saccharide isomerate, and vitamin E, applied in the morning; and PapiX™ high (Relife Menarini Group), a purifying gel (medical device) of salicylic acid (2.5%), zinc gluconate, taurine, urea peroxide, and vitamin E, applied at bedtime.
The study was conducted across four centres, and enrolled 41 adults with mild comedonal-papular acne. The mean age of patients participating in this study was 20.5±5.0 years, and subjects had an average of 16.1 (±16.6) comedones, and 7.9 (±4.5) inflammatory lesions at baseline. In order to be eligible to participate in the study, patients were required to undergo a wash-out period of at least 4 weeks for topical pharmacological agents and/or oral antibiotics, and at least 3 months for oral isotretinoin. Key exclusion criteria for the study were severe underlying diseases; concurrent exposure to sunlight and/or artificial UV sources; pregnancy/breastfeeding; and use of other topical products or drugs (except make-up and oil-free sun protection factor 50+ sunscreens). Clinical assessment was based on total lesion count at baseline and Weeks 4 and 8, together with an IGA evaluation of efficacy at 8 weeks. Instrumental assessment consisted of erythema-directed digital photography by the VISIA-CR (Canfield) system to investigate inflammation, response to therapy, and associated side effects over time. The VAS was used to assess patient discomfort at all time points, and tolerability and acceptability were documented at Weeks 4 and 8.
Micali presented the key results from this study, which demonstrated statistically significant reductions in both non-inflammatory and inflammatory lesions compared to baseline at Weeks 4 and 8 (Figure 2).15 Comedone count was reduced from 16.1 at baseline to 14.0 at Week 4, and 8.1 by Week 8 (p<0.0001). Study subjects also experienced an improvement in their inflammatory lesions score from 7.9 at baseline to 6.4 at Week 4, and 4.4 at Week 8 (p<0.0001). According to the IGA assessment of efficacy at 8 weeks, 40% of patients (12 out of 30) achieved a ‘great improvement’, 26.6% (eight out of 30) an ‘improvement’, and 20% (six out of 30) a ‘mild improvement’. Clinical outcomes remained ‘unchanged’ in three patients (10%), and only one patient experienced worsening acne (3.4%). In terms of patient discomfort, a significant reduction of VAS score was recorded from baseline to Weeks 4 and 8: 6.2 versus 5.2 versus 4.2, respectively (p<0.0001). At Week 8, the majority (90.0%) of patients rated the tolerability of the salicylic acid-based daily routine as excellent, and the score for acceptability was near perfect (97.5%).15 Micali reinforced these clinical outcome data with patient images visually, illustrating the improvements in acne achieved over the course of this study.
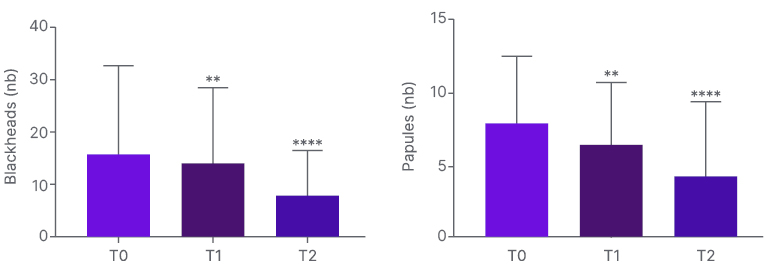
Figure 2: Salicylic acid-based daily routine for mild acne: total lesion count.15
T0: baseline; T1: Day 7; T2: Day 14.
The efficacy of the PapiX™ salicylic-acid based acne regimen is due to a synergistic mechanism of action of all the active ingredients.10 The salicylic acid itself (2.0–2.5%) works to reduce inflammation, and is also a keratolytic agent. Nicotinamide helps with sebum control and also reduces inflammation, while urea peroxide is an antiseptic agent targeting the causative C. acnes bacteria. Glycolic acid is another keratolytic ingredient, while the zinc/taurine component of the product works to tackle inflammation. Finally, saccharide isomerate acts as a moisturising agent. Together, the main ingredients in this new salicyclic-acid based acne regimen therefore target all the key pathogenetic factors of acne, Micali highlighted.10
Overall, these results indicate that the tested salicylic-acid based daily routine represents an interesting approach that deserves attention. It can be used for mild inflammatory acne in patients who prefer to start with a non-aggressive treatment, and avoid the potential side effects of pharmacological therapy, which may account for a substantial proportion of patients. The PapiX™ salicylic-acid based acne regimen can also be used in association with conventional therapy in patients with a good tolerability, and/or as a maintenance treatment. Importantly, it is not photosensitising, and so can continue to be used during the summertime.






