Meeting Summary
Psoriatic arthritis (PsA) and hidradenitis suppurativa (HS) are both immune-mediated diseases with common cellular and cytokine pathways involved in their pathogenesis.1 Both are characterised by chronic and systemic inflammation and both involve elevated levels of the cytokines tumour necrosis factor-α (TNF-α), interleukin-17, and interleukin-23.1-5 PsA and HS are associated with substantial unmet needs and are sub-optimally managed. This educational session discussed ways to improve the quality of care and patient outcomes in PsA and HS.
Dr Kim Papp opened the symposium with an overview of the current unmet needs in PsA and HS and the key barriers to improving the management of both diseases. Prof Hilary Thomas discussed the Quantum initiative and how it could assist dermatologists in the treatment of PsA and HS. Dr Papp and Prof Christos C. Zouboulis then discussed the challenges of achieving optimal management in PsA and HS, as well as the solutions.
Unmet Needs in Psoriatic Arthritis and Hidradenitis Suppurativa
Doctor Kim Papp
In his overview, Dr Papp pointed to misdiagnosis, delays in diagnosis, the lack of awareness among physicians and patients of either condition,6 and undertreatment of patients as the main unmet needs in PsA and HS. He also cited the lack of evidence-based treatment and guidelines as a barrier to effective disease management in HS. Both PsA and HS are associated with a high prevalence of comorbidities such as cardiovascular comorbidities and impaired quality of life, where patients’ physical function and ability to work and socialise are adversely affected. The financial burden associated with both diseases is substantial both to the patient, due to lost productivity arising from impaired physical function, and to the healthcare system, in which patients fail to receive optimal treatment due to misdiagnosis. Thus, there are hospitalisations and vast amounts of resources expended for inappropriate treatments over time. Dr Papp observed, based on the literature and his own experience, that some patients have symptoms for up to 10–15 years before they receive a diagnosis for HS.
How Quantum Can Help Dermatologists
Professor Hilary Thomas
The goal of the AbbVie Quantum initiative is to improve quality of care and, ultimately, patient outcomes, through the following:
- Raising awareness of the current challenges in identification and management
- Increasing levels of active patient participation in the management of disease
- Reducing the level of misdiagnosis and delays in diagnosis
- Promoting dialogue between centres of care to enable sharing of good practices
- Encouraging greater collaboration between specialties
- Delivering consistent care across geographic regions and hospitals
KPMG has supported AbbVie for the past 2 years in the development of Quantum across a range of therapeutic areas, including PsA and HS. The Quantum reports capture key learning on best-in-class care from selected centres, and are then disseminated for the purpose of sharing those insights and promoting improvement in the quality of care.
The process of developing and disseminating Quantum reports comprises four phases:
1) Selecting and engaging centres: In the first phase, KPMG selects and engages centres worldwide to cover a broad spectrum of healthcare systems and patient demographics. Centres of particular interest are those with individuals or groups of individuals who are experts in the field under investigation.
2) Learning from the centres: In the second phase, KPMG seeks to interview the full range of stakeholders involved in the management of the disease. Typically, KPMG would speak with as many healthcare professionals and staff at the selected centres as possible, from specialists and general practitioners to nurses, social workers, and pharmacists, to gain a first-hand understanding of the key challenges they face and the interventions that have been put in place to address them. The outreach is also extended to patients and patient associations to enhance KPMG’s understanding of the personal impact of current standards of care.
3) Synthesising the findings in a global report on good practice: In the third phase, these findings are synthesised first into a centre-specific report on good practice and then into a global report drawing out the main themes and conclusions on good practice from the various centres.
4) Sharing the report and facilitating peer learning: In the fourth phase, the report is shared with the wider scientific, medical, and patient communities with the aim of helping other centres achieve best-in-class care and improvement in outcomes.
The KPMG report on PsA, entitled ‘Improvement in the Management of Psoriatic Arthritis’, was the result of visits to seven centres in the USA, Canada, UK, Germany, South Africa, Hong Kong, and Argentina.7 The report was reviewed and validated by the Group for Research and Assessment of Psoriasis and Psoriasis Arthritis (GRAPPA) and was presented at their Annual Meeting in Miami, Florida, USA, in July 2016.
The KPMG report on HS, entitled ‘Guiding Principles in Hidradenitis Suppurativa Care’, captures the insights gained from visits to eight centres in Western Europe, Canada, and the Middle East.8 It has been reviewed and validated by Prof Zouboulis as President of the European Hidradenitis Suppurativa Foundation (EHSF) in 2016.
Prof Thomas believed that Quantum would help reduce the rates of misdiagnosis and delays in diagnosis in PsA and HS as well as encourage increased collaboration between specialties. She underscored the fact that one of the themes that had emerged from her work was the importance of care networks. She pointed to Canada as an example of a vast country with widely distributed population centres where community networks have given patients greater access to care, reducing their need to travel distances ≤200 miles each way to receive treatment in a major urban centre. Furthermore, Prof Thomas expected care networks to help raise the level of patient involvement in their own disease management, increase dialogue and the sharing of good practices between centres, and contribute to the delivery of consistent care across geographic regions and hospitals.
In Prof Thomas’ view, the Quantum initiative is helpful to dermatologists in the following ways:
- Provides insights on the management of PsA and HS from leading specialist reference centres, secondary and tertiary care centres, and community clinics
- Maps the common challenges in the management of PsA and HS
- Provides insights on how challenges are addressed in specialist centres
- Provides guidance on the implementation of solutions to common clinical challenges in a wider group of clinics across the network, and where appropriate, across communities
Achieving Optimal Management of Psoriatic Arthritis: The Challenges and the Solutions
Doctor Kim Papp
The patient pathway in PsA comprises four stages:
- Pre-diagnosis (patient experiences symptoms)
- Referral and diagnosis (patient receives a referral to a dermatologist or rheumatologist and receives a diagnosis)
- Treatment initiation and management (patient begins treatment)
- Follow-up (long-term management with regular monitoring)
The challenges associated with each phase and their solutions are described in Table 1.7
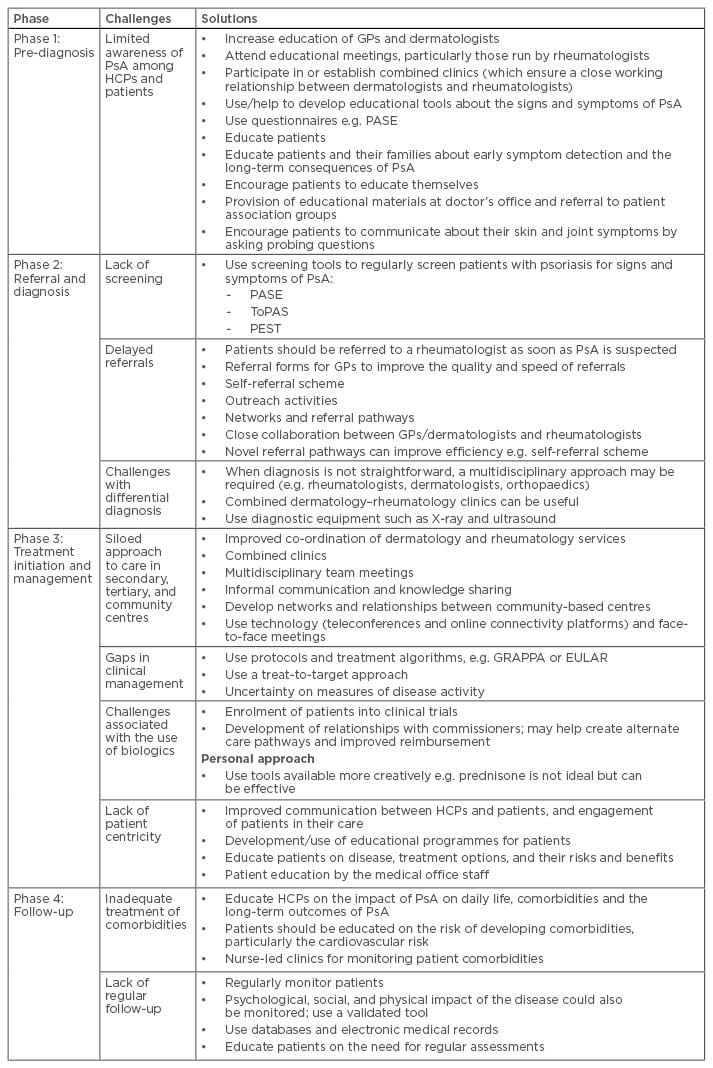
Table 1: Patient pathway in psoriatic arthritis: challenges and solutions.7
EULAR: European League Against Rheumatism; GP: general practitioner; GRAPPA: Group for Research and Assessment of Psoriasis and Psoriatic Arthritis; HCP: healthcare professional; PASE: Psoriatic Arthritis Screening and Evaluation; PEST: Psoriasis Epidemiology Screening Tool; PsA: psoriatic arthritis; ToPAS: Toronto Psoriatic Arthritis Screening.
Achieving Optimal Management of Hidradenitis Suppurativa: The Challenges and the Solutions
Professor Christos C. Zouboulis
Low clinician awareness of HS is the leading cause of delayed diagnosis, misdiagnosis, and lack of or misdirected referrals in HS, and it represents the principal challenge to achieving improvement in HS management and outcomes.8 These challenges are present at each stage of HS management (presentation of first symptoms, diagnosis, referral to a dermatologist or rheumatologist, initiation of treatment, long-term follow-up, and ongoing care).8 The challenges faced at each of these stages of HS management, along with their solutions, are outlined in Table 2.
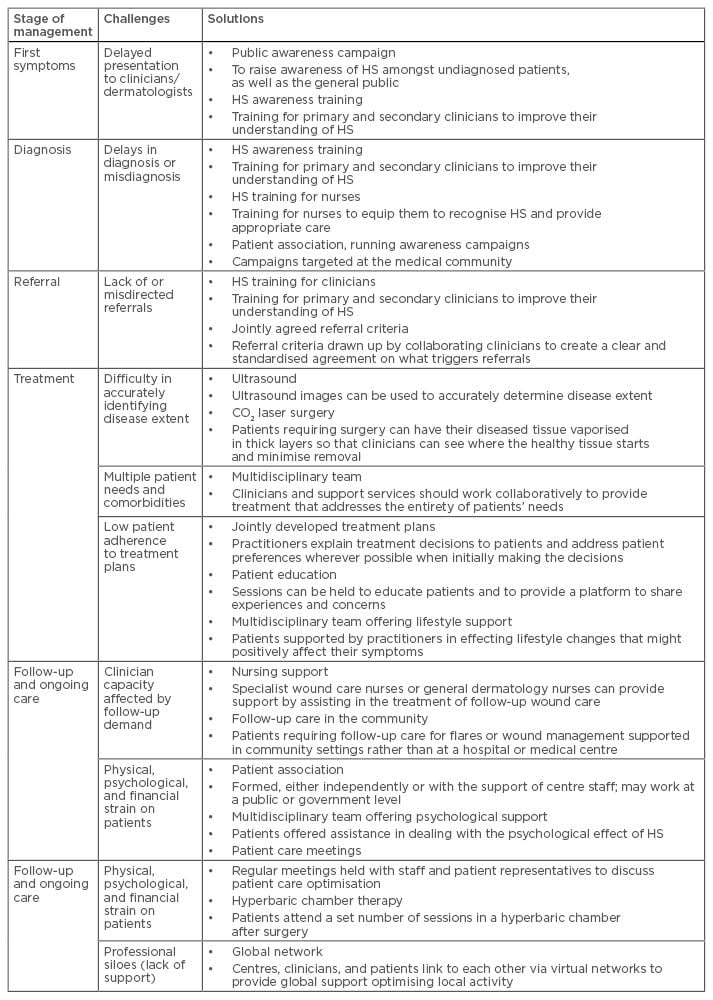
Table 2: Patient management in hidradenitis suppurativa: challenges and solutions.8
HS: hidradenitis suppurativa.
Professional scientific associations that are relevant to HS include the EHSF, which has published diagnostic criteria for HS as well as the European and evidence-based guidelines for the treatment of HS, and the World Union of Wound Healing Societies (WUWHS), which has issued a position document on HS entitled ‘Understanding Hidradenitis Suppurativa’.9 AbbVie indirectly supports the HS Alliance, whose mission is to generate clear and credible guidance on the treatment and management of HS through the development of evidence statements. Initiatives sponsored by AbbVie include ‘What’s Your Sore Spot?’, a patient-focussed website with information about HS;10 and EIDON (Expertise in Delivering Optimal Care in HS), a medical education programme aimed at improving HS management through the establishment of a European network of specialist reference centres and sharing of best practices between the centres.
Discussion: Practical Solutions in Psoriatic Arthritis and Hidradenitis Suppurativa
Doctor Kim Papp
Symposium participants were asked to propose high-impact short-term (≤6 months) action plans for PsA and HS that would be simple to implement. Table 3 shows an example of a proposed action plan.
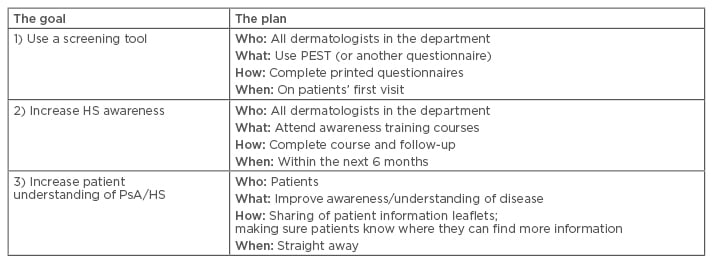
Table 3: Proposed action plan for psoriatic arthritis and hidradenitis suppurativa.
HS: hidradenitis suppurativa; PEST: Psoriasis Epidemiology Screening Tool; PsA: psoriatic arthritis.
As highlighted in this symposium, PsA and HS are associated with substantial unmet needs including delayed diagnoses or misdiagnoses, lack of or misdirected referrals and undertreatment of patients. Low clinician awareness is the leading cause of delayed diagnoses and misdiagnoses. Therefore, increasing healthcare professionals’ education and awareness is critical for improving the management of, and outcomes in, both diseases.







