BACKGROUND AND AIMS
Females with Type 1 diabetes mellitus (T1DM) are at increased risk of adverse pregnancy outcomes.1 Compared to the general population, there is a higher prevalence of congenital malformations, caesarean delivery, fetal macrosomia, large for gestational age (LGA) infants, pre-eclampsia, preterm delivery, and neonatal mortality.2-4 Insulin regimens in pregnancy include multiple daily insulin (MDI) injections and continuous subcutaneous insulin infusion (CSII) via insulin pumps.5-7 With advancing technologies, continuous glucose monitoring (CGM) is increasingly used in antenatal care at the expense of self-monitoring of blood glucose (SMBG).8-10 The aim of the authors’ study was to evaluate the effectiveness of different management options on perinatal and neonatal health outcomes.
MATERIALS AND METHODS
The authors performed a retrospective cohort study of 232 pregnant females with T1DM from a single university-affiliated perinatal centre in the Czech Republic. Females were divided into four groups, according to the mode of glucose monitoring and treatment: SMBG with MDI injections (SMBG+MDI), SMBG with CSII (SMBG+CSII), CGM with MDI injections (CGM+MDI), CGM with CSII (CGM+CSII). Data were retrieved from the electronic
medical records.
RESULTS
Overall, 35.3% of females attended preconception counselling, with more females in CGM+CSII and less in the SMBG+MDI group (52.7% versus 18.2%; p=0.002). The authors observed lower mean HbA1c concentrations prior to conception in CGM+MDI and CGM+CSII groups (55.1±15.3 and 54.3±12.4, respectively; p=0.005). On univariate analysis, a higher rate of liveborn infants (97.0%; p=0.031) was observed in the CGM+MDI group. There was a higher incidence of operative delivery (caesarean section or instrumental vaginal delivery) in the SMBG+CSII (81.3%; p=0.048) group and fewer cases of LGA infants among females with CGM+MDI, but more in the CGM+CSII group (18.8% versus 48.1%; p=0.039). There were no cases of umbilical artery pH <7.15 in the CGM+MDI group (0; p=0.006). Perinatal results are summarised in (Table 1). Logistic regression showed that CGM+MDI decreases the odds of operative delivery (odds ratio [OR]: 0.29; 95% confidence interval [CI]: 0.116–0.707; p=0.007), LGA (OR: 0.34; 95% CI: 0.124–0.923; p=0.034), and umbilical artery pH <7.15 (OR: 0.04; 95% CI: 0.002–0.790; p=0.034). The results did not reach statistical significance after adjusting for maternal age, BMI, diabetes compensation, and morbidity.
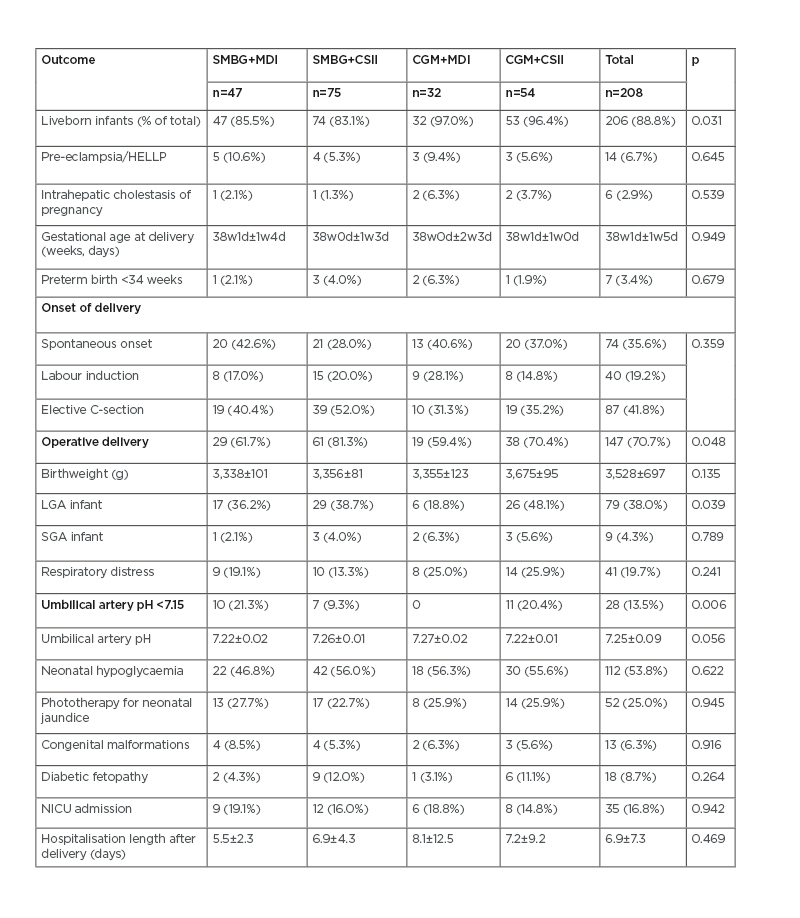
Table 1: Perinatal results for operative delivery, caesarean section, or instrumental vaginal delivery.
CGM: continuous glucose monitoring; C-section: caesarean section; CSII: continuous subcutaneous insulin infusion; d: days; HELLP: haemolysis, elevated liver enzymes, and low platelet count syndrome; LGA: large for gestational age; MDI: multiple daily insulin; NICU: neonatal intensive care unit; SGA: small for gestational age; SMBG: self-monitoring of blood glucose; w: weeks.
CONCLUSION
The authors’ study suggests that perinatal outcomes of females with T1DM are affected by the modality of glucose monitoring and insulin regimen. CGM together with MDI injections are associated with lower rates of operative delivery, LGA infants, and fetal hypoxia.








