BACKGROUND AND AIMS
Females with gestational diabetes mellitus (GDM) are at an increased risk of complication during delivery (adverse perinatal outcomes) and having abnormalities in glucose metabolism postpartum. They are also seven times more likely to develop prediabetes or Type 2 diabetes mellitus.1,2 At the same time, GDM represents a risk for the offspring as children of mothers with GDM are more prone to develop childhood obesity, cardiovascular diseases, or Type 2 diabetes mellitus.3
The aims of this study were to ascertain possible anthropometric and psychomotor development abnormalities and/or morbidity in the offspring of GDM mothers versus controls in a 5-year follow-up; and to describe the consequences of perinatal morbidity (adverse perinatal outcomes) with childhood morbidity or psychomotor development in a cohort of offspring of GDM mothers versus controls. The secondary aim was to investigate whether the mother’s obesity plays a role in the development of the offspring independent of GDM.
MATERIALS AND METHODS
The baseline study population comprised a total of 432 participants. Of those, 68 had a physiological pregnancy without GDM and 364 had GDM, previously described in another study.4 All follow-up participants were contacted electronically through a questionnaire designed according to the ‘child health card’, which is available to all children in the Czech Republic healthcare system. The evaluated parameters can be seen in Table 1. A subset of n=89 (20.6% of females at baseline; 26 with GDM and 63 controls) participated in the prospective study.
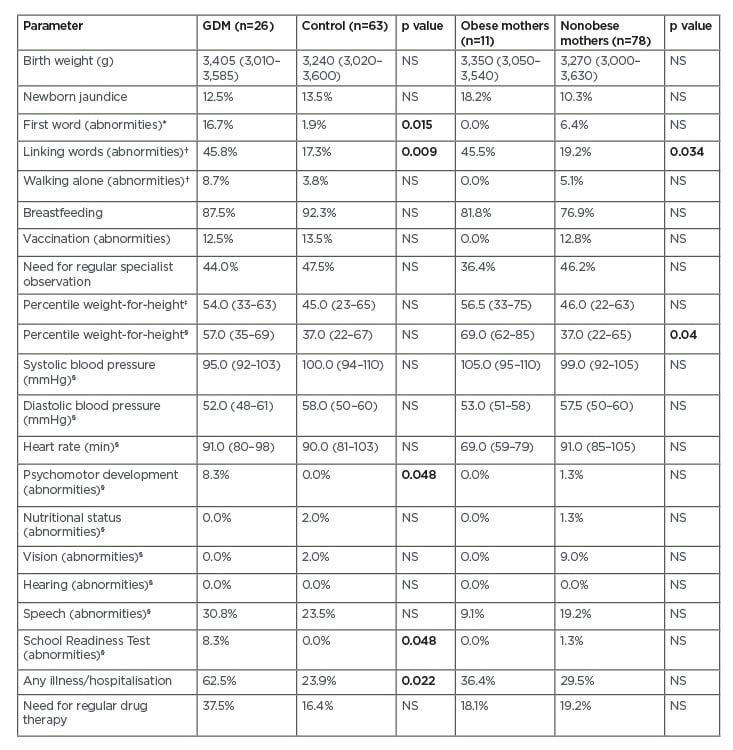
Table 1: Offspring data.
Data expressed as median interquartile range, Mann-Whitney test or frequency (%), and Chi-square test. Bold number indicate statistically significant results.
*evaluated at 12 months of age.
†evaluated at 18 months of age.
‡evaluated at 3 years of age.
§evaluated at 5 years of age.
GDM: gestational diabetes mellitus; NS: nonsignificant.
RESULTS
Mothers with GDM in the second trimester of pregnancy had a significantly higher BMI (p=0.019, Mann-Whitney test); obesity was also higher in the GDM group, but this was not statistically significant. Those with GDM also smoked actively or were former smokers (p=0.012, Chi-square test). Offspring in the control group were breast-fed for longer periods (12 months; interquartile range: 8–17) compared those in the GDM group (6 months; interquartile range: 3–22), but the difference was not statistically significant.
Perinatal parameters of both groups (GDM versus controls) were comparable. Adverse perinatal outcomes (macrosomia, length of delivery, and necessity of instrumental delivery) had no significant influence on the psychomotor development or morbidity of the offspring ≤5 years, in both groups.
Offspring data were compared at 3 years and 5 years. At the age of 12 and 18 months, offspring of GDM mothers had significantly worse speech abilities: they did not say any words at 12 months of age and did not link words at 18 months of age (p=0.015 and p=0.009, respectively, Chi-square test). The speech abilities at the age of 5 years were better in the control group, but the difference was not statistically significant. The Psychomotor Development Screening Test and School Readiness Test (SRT) were borderline worse in the GDM group at 5 years of age (p=0.048 for both, Chi-square test). Offspring of GDM mothers were ill more in their first 5 years of life and required hospitalisation (p=0.022, Chi-square test), with upper respiratory tract illnesses and allergies arising most frequently (Table 1).
CONCLUSION
The authors presented a unique prospective study focussing on the children of mothers with GDM ≤5 years of age and found several differences in selected parameters in the offspring, primarily in their speech abilities and total morbidity. Moreover, a significant link to the mother’s obesity and the offspring’s increased adiposity was noted, independent of GDM.








