Abstract
Context: Non-communicable diseases (cardiovascular diseases, hypertension, and diabetes) and comorbid common mental disorders are of public health concern because of their high morbidity and mortality rates. The authors undertook a systematic review of studies that reported the prevalence of common mental disorders among non-communicable diseases, specifically in India.
Evidence acquisition: Relevant databases (Medline, Google Scholar, EBSCO, and ProQuest) were searched until May 2021. Descriptive and observational studies from the mentioned databases were included.
Evidence synthesis: Of the total 6,515 studies, the electronic literature search identified 4,307 studies. Manual cross-referencing identified an additional 2,208 studies. Only 17 studies met the criteria and were included for the review.
Findings: Twelve studies focused on the prevalence of anxiety and depression in patients with diabetes, four studies focused on cardiovascular disease, and one on the prevalence of depression in hypertension. The prevalence of anxiety disorder and depression was 3.9–44% and 8–44%, respectively.
Conclusion: High prevalence of anxiety and depression is seen in people with diabetes, indicating these are of serious public health concerns in India.
Key Points
1. Common mental disorders and non-communicable diseases (NCD) are interlinked, and the pathways of comorbidity have been described to be reciprocal.
2. This systematic review of Indian studies illustrates the high prevalence of anxiety and depression in NCDs, specifically in diabetes.
3. The findings of the review highlight the need to focus on the integration of services in healthcare to improve the screening and identification of common mental disorders in people with NCDs.
INTRODUCTION
Non-communicable diseases (NCD) are defined as medical conditions that cannot be transmitted.1 They are characterised by a chronicity of at least 3 months and are progressive in nature. The conditions categorised as NCDs are cardiovascular diseases (CVD), respiratory diseases, obesity, gastrointestinal disorders, diabetes, cancer, and endocrine and metabolic disorders.2 NCDs such as heart diseases, cancer, stroke, and diabetes are the leading cause of mortality in the world.3 The combined burden of these diseases is rising fast among lower-income countries.
According to the Global Status Report on NCDs (2010), 80% of CVD and diabetes, and 90% of deaths from chronic obstructive pulmonary disease, occur in low- and middle-income countries.4 The recent edition (2020) indicates that 70% of deaths worldwide are due to NCDs.4
The modifiable risk factors associated with NCDs are tobacco use, physical inactivity, unhealthy diet, and the harmful use of alcohol.4 Tobacco accounts for 7.2 million deaths every year, more than 3.3 million annual deaths have been attributed to alcohol use from NCDs, including cancer, and 1.6 million deaths can be attributed to insufficient physical activity.5 These risk factors lead to metabolic and psychological changes in the body, such as raised blood pressure, overweight/obesity, hyperglycaemia, and hyperlipidaemia.4
There have been increasing calls to include common mental disorders (CMD) such as depression and anxiety under the umbrella of NCDs. However, the prevention and control of both diseases remain separate and independent. CMDs typically include anxiety, depression, and somatic complaints and cause limitations in daily activities.6 CMDs are identified as the leading contributors of disability globally, but they are less likely to receive treatment.7 This reflects stigmatisation, and they are undetected most of the time.7,8 The aetiological factors for CMDs can be psychological, social, and biological. The causal mechanism of the risk factors of NCDs and CMDs also operate at the individual level (genetic factor), psychological level, and societal level (social determinants). Thus, CMDs and NCDs are interlinked and highly comorbid. The pathways of comorbidity have been described to be bidirectional in nature.9,10 For example, diabetes elevates the risk of depression and vice versa.11 These conditions share common diathesis contributing to the onset of other comorbid conditions.12 The psychological burden of being ill and associated health factors can act as triggering factors in the development of depression and anxiety among patients with diabetes.13 Similarly, depression leads to unhealthy dietary practices, less physical activity, tobacco use, harmful use of alcohol, and weight gain, which are risk factors for diabetes. Risk factors for NCDs tend to cluster together.8
Depression and anxiety have also been recognised as systemic illnesses that negatively affect physical health.14,15 People with CMDs may use nicotine and alcohol, which can further affect their physical health. This not only contributes to NCDs but also increases the burden of depression and anxiety. Tobacco and alcohol use are also linked with common and severe mental illness. Along with NCDs, from a societal perspective, tobacco use in mental disorders might be a significant contributor to premature mortality.16
The likelihood of depression tends to double for patients with diabetes, when compared with the general population without diabetes.17,18 Patients with diabetes may have excessive fear and worry about the disease, which can result in anxiety, and anxiety disorders are associated with hypertension.19,20 Hypertension may trigger an anxiety disorder and, conversely, an anxiety disorder may lead to hypertension.21 Studies suggest that individuals experiencing depression are at risk of developing hypertension, and are predisposed to stroke and ischaemic heart disease (IHD).22,23 They are more likely to develop CVD and have a higher mortality rate. Hypertension is also an important risk factor for the development of coronary heart disease.24 There exists a graded relationship among both: the more severe the depression, the higher the risk of mortality and other cardiovascular events. The economic indicators relating to CVD and depression are high medical cost, increased health service utilisation, and less productivity. These factors contribute to poor quality of life (QoL).25
There is also evidence that lifestyle risk factors such as diet, physical inactivity, smoking, and alcohol use, besides non-modifiable risk factors such as age, poverty, and gender, contribute to comorbidity.12 It is also evident that depression and anxiety are prevalent in people with physical comorbidities, specifically in South Asia.26 There is an increasing trend in the prevalence of both CMDs and NCDs in developing countries such as India.26 Major risk factors of NCDs in India are high systolic blood pressure, high fasting plasma glucose, and high BMI.27 In 2013, there were an estimated 65.1 million diabetes cases; this is expected to increase up to 109.0 million in 2035.28 The World Economic Forum (WEF) estimated that countries such as Brazil, China, India, and the Russian Federation lose more than 20 million productive life years annually to NCDs.3
Most of the time, depression goes undetected despite its high prevalence in NCDs. Patients do not receive adequate treatment, which further deteriorates their physical health. This suggests addressing the risk factors and integrated management of mental disorders and NCDs. In view of this, it is important to screen patients for NCDs and CMDs. Thus, this study aimed to review the literature from India on the prevalence of CMDs in NCDs and vice versa.
OBJECTIVES
- To study the prevalence of anxiety and depression in hypertension, diabetes, and CVD in India; and
- To study the prevalence of hypertension, diabetes, and CVD in anxiety and depression in India.
METHODS
Evidence
Electronic databases such as PubMed, Medline, EBSCO, CINAHL, ProQuest, and Google Scholar were searched for the time period of 1980 to May 2021. The keywords used for the search strategy were “prevalence,” “anxiety,” “depression,” and “hypertension;” “prevalence,” “anxiety,” “depression,” and “diabetes mellitus;” and “prevalence,” “anxiety,” “depression,” and “cardiovascular diseases.” The evidence was screened for inclusion criteria using a three-stage approach: reviewing the title, abstract, and full text. The authors included studies that were published between 1980 and May 2021 in indexed and non-indexed journals, and descriptive and observational studies that allowed an estimation of the prevalence of CMDs and NCDs. For this review, NCDs included hypertension, diabetes, and CVD, whereas CMDs included anxiety and depression. The authors included studies from inpatient, outpatient, and community settings, and whose participants were adults (age >18 years) from India. Studies that did not relate to NCDs and CMDs, and those that were randomised control trials or reviews (systematic or non-systematic), were excluded. Studies conducted only amongst the elderly or adolescents were also excluded.
Data Extraction
Microsoft Excel was used to enter the extracted information for the review. The data extraction form included authors’ names, publication year, study design, participants’ profile, sample size, measurements, and outcomes. One author (Rajan) conducted the screening independently by reviewing articles and abstracts. Full-text articles of the abstracts that met the inclusion criteria were then reviewed by two independent authors (Rajan and Chaturvedi). Data of these studies were extracted by two independent authors (Rajan and Krishna). Discrepancies in article inclusion, data extraction, and bias assessment were resolved by consensus or by referring to the third author (Muliyala).
Risk of Bias
The quality of the included studies was assessed by the National Institutes of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies.29 Three independent authors (Muliyala, Krishna, and Rajan) assessed the quality of studies, and disparities were resolved by consensus. The quality rating was based on the total number of “yes” responses and was rated as follows: poor: <50%; fair: 50–75%; and good: ≥75%.
RESULTS
A total of 17 studies that met the inclusion criteria were reviewed. Figure 1 illustrates the screening and selection process in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. Of the total 6,515 studies, the electronic literature search identified 4,307 studies. Manual cross-referencing additionally identified 2,208 studies. After removing 100 duplicate studies, 6,415 were screened and 6,397 were excluded as they did not meet the inclusion criteria. The full text was only reviewed in the remaining 25 studies. Further, eight studies were excluded as they did not concur with the inclusion criteria, resulting in 17 studies for the review.
The characteristics of the included studies are provided in Table 1.
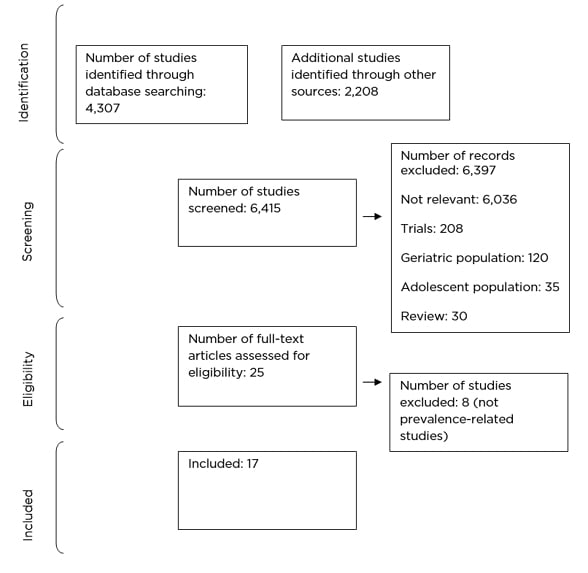
Figure 1: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart
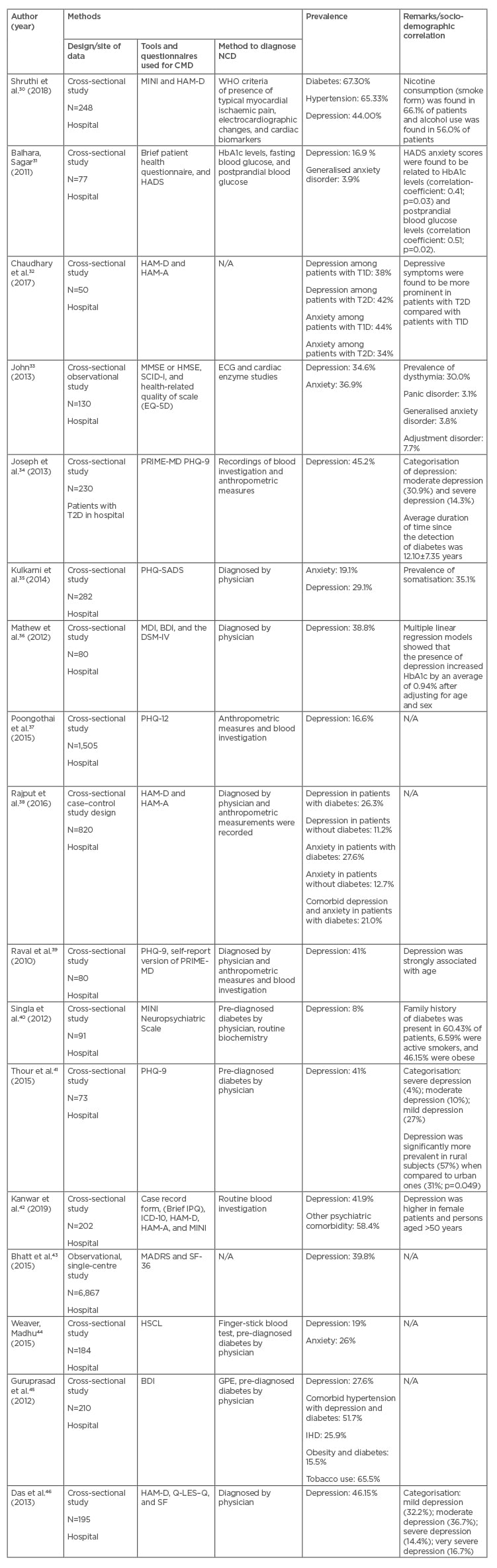
Table 1: Characteristics of studies included in the review.
REVIEW OF THE INCLUDED STUDIES
All the studies included in this review were conducted in hospital settings and were observational studies. Out of the 17 studies, only one had respondents enrolled from an inpatient setting. Overall, 12 studies assessed the prevalence of depression and/or anxiety in NCDs, particularly in diabetes. Three studies evaluated the prevalence of depression in CVD. Only one study looked into the prevalence of CMD in NCD (diabetes, hypertension, and CVD).
Despite the aetiological differences, many studies have not distinguished between different types of diabetes. Only one study focused on Type 1 diabetes (T1D) and Type 2 diabetes (T2D) separately;32 11 studies have focused only on T2D.
Studies That Assessed Depression and Anxiety Disorders in Diabetes
The prevalence of depression in patients with diabetes ranged from 8% to 46%. Risk factors of NCDs such as smoking and alcohol use were also reported in three studies. The sample size varied from 50 to 10,450. Depression was identified by diagnostic interview: International Classification of Diseases (ICD) and Diagnostic and Statistical Manual of Mental Disorder (DSM-IV) in two studies; Physical Health Questionnaire-9 (PHQ-9) in five studies; Hamilton Rating Scale for Depression-17 (HAM-D-17) in three studies; Hamilton Depression Rating Scale (HDRS-21) in one study; Beck Depression Inventory (BDI) in one study; Primary Care Evaluation of Mental Disorders (PRIME-D) in one study; and Hopkins Symptom Checklist (HSCL) in one study. Studies were from Northern (10), Southern (six), and Western (two) regions of India. The prevalence of anxiety disorder and depression in any NCD were 3.9–44.0% and 8.0–46.0%, respectively.
Four studies reported an association between the duration of diabetes and the prevalence of depression, as the incidence of diabetic complications increased with illness duration.31,41,42,45 A higher prevalence of depression was reported in one of the studies among patients having uncontrolled diabetes (glycated haemoglobin test: HbA1c).45 Two studies concluded that patients diagnosed with T2D and depression had poor QoL compared with those without depression. Health-related QoL was adversely affected by the presence of depression.46 Negative correlation was reported between HbA1c and QoL in one of the studies. This supports the view that patients with poor control of blood glucose levels have a worse QoL. One of the studies reported that 67% of patients with diabetes were overweight or obese.45 Two studies indicated that depression was significantly associated with older age,34,39 female gender,34 and complications due to T2D or other comorbidities such as hypertension and being overweight.34,38,39 Conversely, two studies reported that gender was not associated with depression.38,39 One of the studies indicated that depression was more prevalent in rural populations than urban.41 One of the studies showed that depression was significantly associated with retinopathy, nephropathy, and IHD.38 Another study reported that depression was strongly associated with age, central obesity, neuropathy, and nephropathy; however, it also found that depression was not significantly associated with gender.39
Studies That Assess Depression and Anxiety Disorders in Hypertension
Out of 17 studies, only one, conducted in a hospital in Mangalore, India, reported a prevalence of depression in patients with hypertension as 28%.35
Studies That Assess Depression and Anxiety Disorders in Cardiovascular Diseases
Among the four studies that assessed the prevalence of depression in CVD, one focused on IHD in general, two focused on acute coronary artery disease, and one focused on carotid artery intima-media thickness. One study assessed the relationship between IHD and QoL. Poor QoL was reported among patients with IHD and comorbid anxiety and depression.33 In one of the studies, depressive symptoms were associated with functional and structural markers of atherosclerosis, common carotid intima-media thickness, and augmentation index.37
DISCUSSION
In this review, the authors have presented a comprehensive summary of existing research on the comorbidity of CMDs (anxiety and depression) and NCDs (hypertension, CVD, and diabetes) in India. The data presented in this review reflects the high prevalence of anxiety and depression in NCDs, specifically diabetes. The prevalence of depression in patients with diabetes in the present study was 8–46%. Studies that were based in the USA and the Netherlands, which were included in a systematic review on the epidemiology of diabetes and depression, conducted among patients with diabetes, reported the prevalence rate of depression as 32.1% and 19.3%, respectively. Though these are from high-income countries, they are within the range of the present study.47 The estimated prevalence of depression in patients with hypertension in one of the meta-analyses was reported to be 21.3%, and the range of point prevalence of 41 studies was observed to be between 0.5% and 73%.48
Twelve studies included in the review examined the prevalence of CMDs in diabetes. Diabetes and psychiatric disorders share a bidirectional association, both influencing each other in multiple ways.49 People with diabetes are two-times more likely to develop depression relative to people without depression, and patients with depression have poorer clinical parameters and outcomes of diabetes because of poor medication compliance and dietary practices.50 It has also been reported that comorbid anxiety and depression in people with diabetes also leads to medical complications of diabetes, work disability, and poor QoL.51 Patients with diabetes are likely to face challenges at physical, emotional, psychological, social, occupational, and interpersonal levels.52 The complications associated with the management (medication dosing, monitoring blood glucose, eating patterns, and physical activity)53 of diabetes can lead to negative emotions such as worry, fear, and anger, which result in poor QoL.50 Among the studies reviewed, 11 have focused on T2D despite the aetiological differences. T1D is an autoimmune condition, whereas T2D is linked with genetic and lifestyle choices.54 Both types of diabetes lead to health complications. Depressive symptoms seem to be slightly more prevalent in T2D compared with T1D.11
The co-occurrence of NCDs and CMDs has been associated with elevated symptom burden, functional impairment, and a decrease in QoL.9 The authors found that the prevalence of anxiety and depression was higher in females compared with males, similar to the studies done elsewhere.55 Depression was identified either by diagnostic interviews or diagnosis by a general practitioner (n=2). The tools used in the studies were PHQ-9, HAM-D, and BDI, which are widely used in clinical practice and research. PHQ is a screening tool commonly used in primary care, HAM-D is a widely used clinician-administered depression assessment scale, and BDI is a self-reported inventory to measure the severity of depression. It is reported that the estimate of depression prevalence depends upon the assessment tools (standardised interview or self-report questionnaires, classification of depression, and diabetes type).11 Depression assessed with self-report questionnaires is found at a rate two-times higher than when assessed with standardised interviews.17,53 The overall quality of the studies included in the systematic review was good. In the risk of bias assessment, most studies were categorised as good (n=14). All the studies used standardised tools that were reliable and valid for assessment.
CMDs, particularly depression and anxiety, often go undetected, and systematic screening, even in high-income countries, is not satisfactory.9 Thus, the screening of CMDs in primary care by using a brief instrument should be made mandatory in routine clinical encounters. This integration has also been reported as an evidence-based approach for collaborative care.16
Addressing the overlapping risk factors and integrating the management of CMDs and NCDs can improve clinical outcomes.56 Management of NCDs and CMDs can be made by adopting existing integrated models of care. The inter-related causal mechanism of CMD and NCD argue for an integrated approach to care.16 The management of T2D and depression in the primary setting has been effective using the educative model, where healthcare professionals are trained to identify, refer, and communicate with the patient about the symptoms of CMD.57 The efficiencies of integrated care have proven beneficial for both high-income and low- and middle-income countries.16
Several policies and programmes have been adopted in India to tackle the rising burden of NCDs and mental illnesses.58 These include the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) and District Mental Health Programme (DMHP). It has been reported that the major challenges are in terms of inadequate resources and ineffective implementation of the programmes.58 To overcome these challenges, health and wellness centres have been envisaged under the Ayushman Bharat programme of the Government of India, encompassing a range of services for NCDs and mental health closer to the community.59 Health and wellness centres focus on wellness and lifestyle modification through various activities such as yoga, local sports, and other activities. The screening of NCDs is done by accredited social health activists or auxiliary nurse midwifes through the Community Based Assessment Checklist (CBAC). Identified individuals are then referred for necessary treatment. According to the recent statistics, approximately 9.1 crore screenings for hypertension, and 7.4 crore screenings for diabetes have been carried out.60
In addition, for effective management, social workers, accredited social health activists, auxiliary nurse midwifes, and NCD counsellors can be trained for population-based screening of CMDs in NCDs and vice versa, basic counselling skills, brief intervention for lifestyle modification, and behavioural activation.
STRENGTHS AND LIMITATIONS
The search strategy adopted was extensive and comprehensive in nature. The studies were limited to those conducted in India. This review included only the prevalence of anxiety and depression in NCDs and excluded other CMDs (somatisation) and substance use disorders. The pooled prevalence of anxiety and depression has not been provided because meta-analysis was not conducted. Small sample sizes in some of the studies may have contributed to sampling errors. All the studies were hospital-based and, therefore, the findings are not generalisable to the community. There were insufficient data to draw firm conclusions about the prevalence of anxiety and depression in hypertension and CVD, as only three studies evaluated the prevalence of depression in CVD and only one study examined the prevalence of CMD in hypertension. The broad range of prevalence can be explained by the following four factors: use of different tools to screen and assess anxiety and/or depression; the studies were conducted in geographic or cultural settings; sample sizes were disparate; and true variation across the different conditions that have been included as NCDs.
CONCLUSIONS
In summary, the authors found that NCDs and CMDs are underdiagnosed in India. The data related to the prevalence rates of both NCDs and CMDs is limited. Based on studies carried out in India, the prevalence of anxiety disorder and depression in individuals with NCD was 3.9–44.0% and 8.0–46.0%, respectively. The results of the included studies point to disadvantages for people with CMDs and NCDs with respect to risk factors and outcome. Depressive and anxiety symptoms have been strongly associated with poor QoL, health status, and physical function. Thus, future efforts should focus on integrated healthcare, which may help improve screening and identification of NCDs and CMDs; this in turn can improve outcomes.








