The launch of Novo Nordisk’s Wegovy appetite suppressant is giving new hope to people living with obesity, as well as encouraging other players to the market. Still, what barriers stand in the way of wider adoption, and how can pharma marketing teams approach them?
Words by Saša Janković
If you wanted to sum up the content of most diet books from the last few decades, you’d be hard pressed to come up with anything more succinct than “eat less and move more”. Yet if this approach to weight loss actually worked then, surely, we’d have overcome the obesity crisis, even with the additional option of surgical interventions for people living with obesity who most needed them. The data shows this isn’t the case: the World Health Organization estimates that more than 650 million people are living with obesity, which is responsible for 5% of all global deaths.
So, what’s the solution? From a clinical intervention point of view, prescription weight loss drugs are now considered a frontline treatment for people with a body mass index (BMI) of 30 or higher, or a BMI of 27 alongside a metabolic condition such as type 2 diabetes or high blood pressure. Their use is on the rise. Research by financial services company Morgan Stanley claims that obesity is “on the cusp of moving into mainstream primary care management” and, as a result, global obesity drug sales could reach 54bn USD by 2030, propelling obesity from a 2.4bn USD category to a top-12 therapy area by global spending.
Obesity is on the cusp of moving into mainstream primary care management
The latest tool in this obesity medicines armoury is Novo Nordisk’s semaglutide appetite suppressant, which works by imitating an intestinal hormone that stimulates insulin production, lowering appetite and inducing feelings of satiety. Initially approved as a treatment for type 2 diabetes, and prescribed under the names Ozempic and Rybelsus, in 2021 it received FDA, EMA and MHRA approval as a treatment for obesity as Wegovy – a 2.4mg injection indicated as an adjunct to a reduced calorie diet and increased physical activity for chronic weight management in adults with obesity or excess weight.

Adoption issues
Despite some initial manufacturing and supply chain issues, Novo Nordisk says by February 2023 the number of physicians prescribing Wegovy will have already surpassed its other injectable appetite suppressant weight loss product Saxenda. However, the company admits that, notwithstanding the early success of Wegovy, activating patients remains its focus, since “only a fraction of people with obesity visit the doctor, let alone are treated with a pharmacotherapy”.
This is not a new issue. In 2019, Novo Nordisk’s ACTION-IO survey of 14,502 people with obesity and 2,785 healthcare professionals across 11 countries found there was an average of six years between the time a person began struggling with excess weight or obesity and when they first discussed their weight with an HCP.
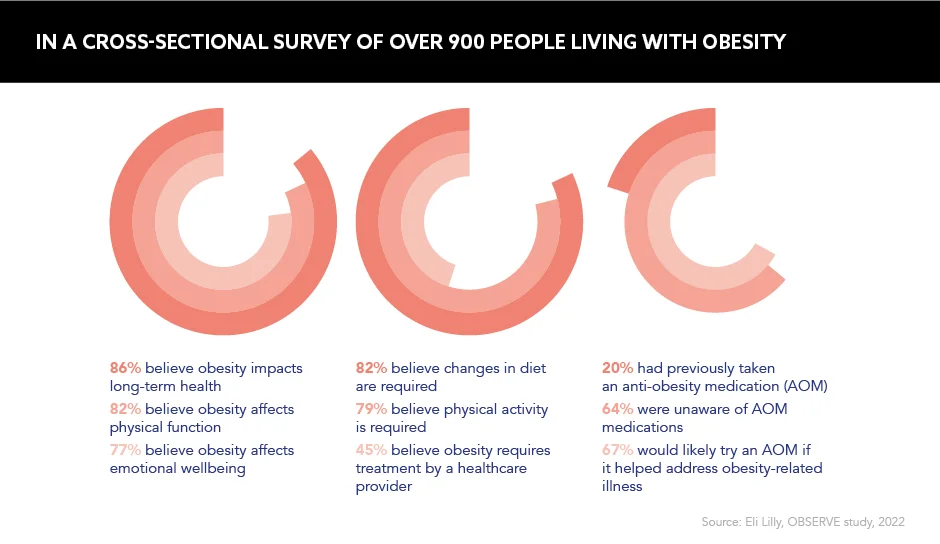
In 2022, Eli Lilly’s OBSERVE study examining the underlying reasons for limitations in obesity care and the slow uptake of anti-obesity medications (AOMs) also revealed that when participants – including people living with obesity, HCPs and employers that make coverage decisions – were asked about obesity treatments, almost three-quarters believed lifestyle and behavioural changes are the best options for long-term weight loss, with 64% unaware of prescription AOMs.
Inspiring behaviour change
Obesity management requires education to support physicians in understanding that obesity is a chronic disease, and to help patients understand the benefits of weight loss and inspire behaviour change to ensure they live healthier and more fulfilling lives.
“Very few people ever present even to get help from an HCP for their obesity and by time they do they have tried things, often for decades, and have been unsuccessful because of the lapsing nature of the disease,” says Julia Dunn, Senior Medical Adviser, Obesity, Medical Affairs, Eli Lilly. “If we can provide effective treatment, we are going to decrease that burden and people are going to be able to live the life they want to live.”
Obesity management requires education to support physicians
Indeed, data from Morgan Stanley shows once people are diagnosed with obesity and recommended for medical treatment around 40% are treated, which is similar to hypertension and slightly behind high cholesterol at approximately 55%. Analysts say the key problem is that only around 7% of people with obesity are diagnosed and recommended for medical treatment compared to some 80-90% with downstream chronic complications including diabetes, high blood pressure and elevated cholesterol levels.
Thankfully, pharma companies are leading the charge when it comes to public awareness. “It is important that we recognise that weight loss is much more than eating less and moving more: a weight loss journey is a unique challenge for every individual”, says George Hampton, President and CEO, Currax – the supplier of another obesity treatment Contrave.
And Adam Burt, Business Unit Director, Obesity, Novo Nordisk UK, agrees, adding that changing the ‘eat less, move more’ mindset is an ongoing challenge. “There is a need for education about obesity and the factors that can influence a person’s weight, as well as resources to support patients on their weight management journey,” he says. As such, Burt recommends empowering patients to gain “a deeper understanding of their condition”, so they can identify triggers and solutions with their HCPs.
Tackling stigma is another challenge. “The culture around obesity continues to perpetuate stigma, forcing people living with obesity to feel ashamed and unable to seek support,” Burt highlights. “Weight stigma is a part of everyday life, however education within the school curriculum about obesity and the affecting factors could encourage families to adopt healthy habits and kinder mindsets.” Obesity can strike at any age, and early touchpoints are crucial.
A holistic approach
It is evident that more education and awareness is needed among HCPs, patients and wider society to understand that obesity is a disease requiring not only lifestyle changes, but medical interventions, too.
It’s not as simple as ‘eat less, move more’, but changing this mindset is an ongoing challenge
Prof. Matthias Blüher, Director, Helmholtz Institute for Metabolic and Vascular Research, and Head of Research Group Clinical Obesity Research, says defining obesity as a disease “would have a strong impact both on the individual in terms of improving self-esteem and reducing stigma, and on wider society in terms of increasing awareness amongst both healthcare professionals and politicians”.
Since eating less and moving more is not the answer on its own, surely now is the time to capitalise on the medical developments that are proving their worth for people living with obesity. Ultimately, in this disease, Burt says, a one-size-fits-all approach will not stack up, and pharma must throw its net far and wide to support patients to live healthier lives.