Patients are more interested than ever in taking control of their own care, but how can the pharmaceutical industry protect them from the maze of misinformation?
Words by Saša Janković
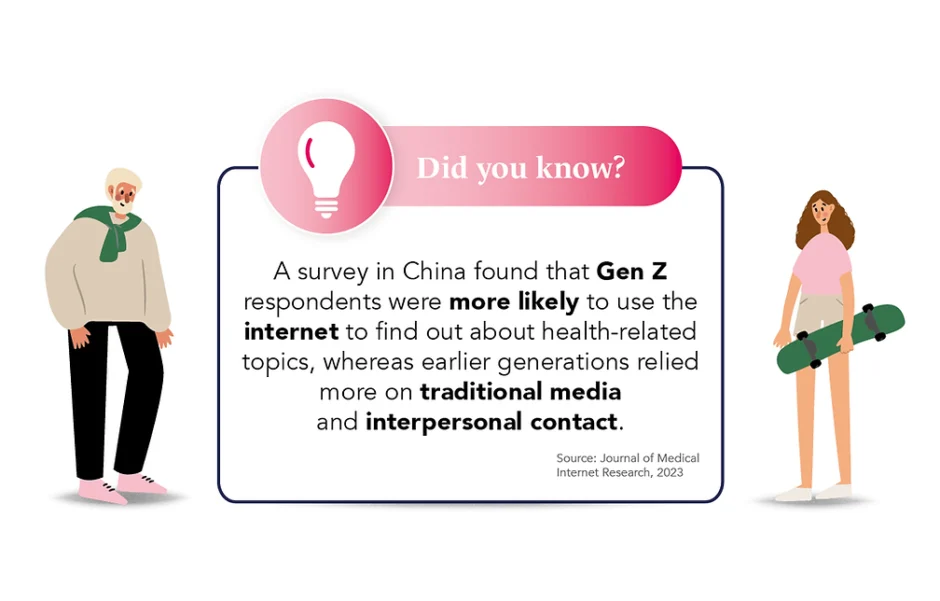
The power of the internet coupled with the air of connectedness that social media creates means finding out information about medical conditions – and medicines – has never been so straightforward, positioning us well and truly in the era of the ‘informed patient’.
In times gone by it was healthcare professionals – and primarily doctors – who were the first port of call for trusted health information, but the last couple of decades have seen this role increasingly usurped by medical information websites (both reliable and bogus), as well as health apps and social media.
However, since not all these sources of information are correct, or even well-intentioned, the result is an increasing potential of risk to individual patients and wider public health. So, what can the pharmaceutical industry do to help protect the safety of the informed patient?
Dangers of misinformation
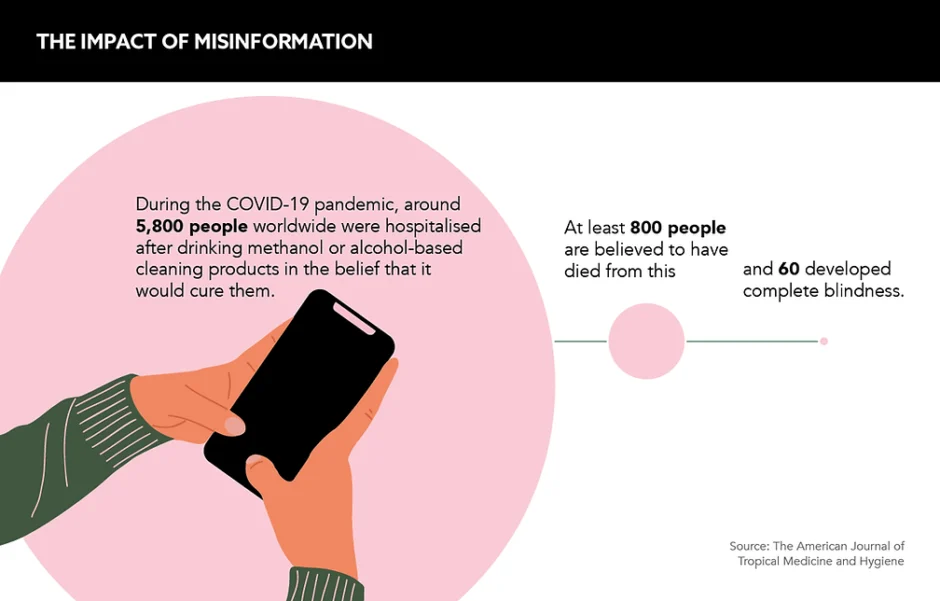
While it is great that patients are becoming more proactive in their care, they can also fall victim to healthcare misinformation, with the COVID-19 pandemic a prime example of this.
Researchers from the Missouri State Medical Association have found that questions raised during the early days of the pandemic around whether or not cleaning products could treat COVID-19 led to a steep increase in calls to poison centres about exposure to household disinfectants.
Anca Toma, Executive Director, European Patients’ Forum (EPF) Belgium, and board member, Patients Focused Medicine Development, says there is “no doubt” that the exponential development of social media and other technology platforms in recent years is playing an important role in the spread of misinformation.
“All patients have a fundamental and legitimate right to access information about their health, their medical condition and treatment, including the different options that are available,” argues Toma. However, she cautions that information must be objective and unbiased, patient-centred and accessible to be truly useful. “If patients don’t receive the information they need from trusted sources, they will look for it elsewhere,” she adds.
On the plus side, studies have shown that there is a positive association between patients seeking health information on the internet and physician visits. Researchers at the Norwegian Centre for E-health Research looked at the association between health information seeking on the internet and physician visits and found that it was positively associated with both the decision to, and not to visit a physician.
Turning the informed into the empowered
While no one is questioning the importance of the informed patient, the role for pharma companies in meeting patient demand for health information must walk a fine line.
On the one hand, patients need better information on disease prevention, diagnosis and treatment, including from pharma companies. On the other hand, is the industry best placed to offer it? Especially as they need to be careful not to tread on the toes of HCPs.
While there is a balance to be struck, Toma believes there are ways in which pharma companies can provide information to patients without interfering with the HCP-patient relationship. For example, she believes it could provide “increased transparency of clinical trial data” to help patients to understand why a drug has been approved for their condition.
In fact, Toma is in favour of “ongoing initiatives” in this area to build patient confidence in medicines and the decision-making processes of regulators. The ongoing review of legislation on patient information leaflets to make them “more readable and accessible” is one such opportunity, she adds.
A helping hand
Patient organisations also play a key role in developing materials and tools for health literacy. Often in partnership with HCPs, patient organisations can support public health and industry efforts to combat misinformation. A role which Toma says “should be better recognised and supported” by the pharma industry.
All patients have a fundamental and legitimate right to access information about their health
“Listening to patient experiences and challenges leads to better clinical trials, better communication and ultimately better products that truly meet their needs,” Toma says. The industry can and should offer more information to patients, but listening has its benefits too.
By exchanging ideas within this “ethical framework”, she concludes, companies can “co-create, co-educate and ultimately improve public health”. Not only will this lead to more informed and empowered patients, it will also take the industry’s knowledge to new levels.