Vaccination rates for preventable conditions have dropped across all age groups, causing as much concern as it has risk to public health. There’s an important role for the pharmaceutical industry to play in helping restore pre-pandemic vaccination levels and protect populations worldwide
Words by Isabel O’Brien
In the summer of 2021, routine vaccination rates were discovered to be another casualty of COVID-19, joining a long line of wounded healthcare delivery services that were derailed by lockdowns and reprioritisations due to the virus.
At the time, concern spread rapidly throughout the industry as leaders in the vaccine arena warned that the world could be heading for outbreaks of entirely preventable, or even eradicated, diseases. As one virus was brought under control, others were given a gateway back into the immune system of society.
“Diseases that are completely preventable should not be circulating in our communities, but they will come back if we don’t do our jobs,” says Judy Stewart, Senior Vice President and Head of US Vaccines, GSK. Her willingness to assume ownership of this complex task has been reflected across the industry, as well as by governments and healthcare systems. Ever since vaccination levels first dropped, the pharma network has been working together to prevent the immunisation gap leading to escalating disease rates, but to what end?
Childhood vaccination rates improving
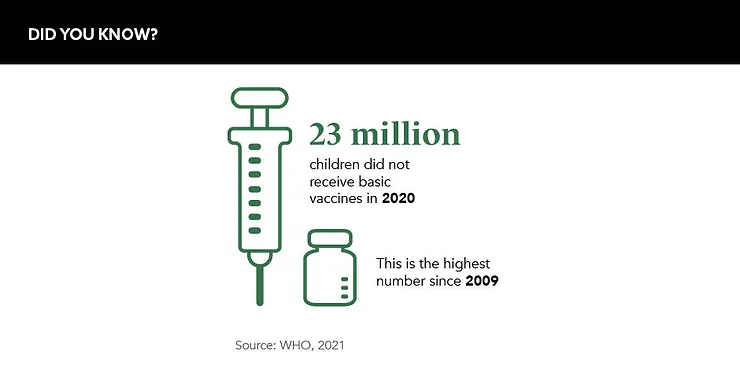
According to the World Health Organization (WHO) and UNICEF, 23 million children under the age of one year did not receive basic vaccines in 2020 – the highest number since 2009. This follows already sub-optimal pre-pandemic levels, with even the US failing to hit the WHO’s childhood vaccinations target of 95% in 2019.
Thankfully, the particularly alarming rates of unvaccinated children began to recover once virtual classrooms closed and physical ones re-opened. “We’ve caught up in the paediatric space as the kids went back to school,” explains Stewart. “It’s not quite there yet, but it is improving at a good pace.” Non-school aged children, however, remain at a disadvantage.
Additionally, in the US, there has been a decrease in well-child visits for this age group – appointments that offer an opportunity for healthcare professionals to remind parents about recommended vaccines and address concerns that may lead to vaccine hesitancy. The annual America’s Health Ranking from the United Health Foundation found that in 2021, well-child visits fell to roughly 80% compared to a pre-pandemic rate of more than 90%. And, worryingly, children from low-income families were found to be the least likely to attend.
Diseases that are completely preventable should not be circulating in our communities
Any disparity in those attending these visits, and any like them in other countries, could lead to a widening of health inequities between a nation’s children, with areas that house lower-income families becoming more vulnerable to the emergence of disease than wealthier ones.
While children around the world have evaded large-scale outbreaks of diseases like measles, mumps or whooping cough so far, countries are issuing warnings to parents urging them to get their children vaccinated against preventable conditions. “There have been outbreaks of measles in recent years in the US, especially in communities with low vaccination rates,” warns Dr Georgina Peacock, Acting Director, CDC Immunization Services Division.
Emphasising that a gap of any size can create unnecessary risk, Dr Vanessa Saliba, Consultant Epidemiologist, UK Health Security Agency, adds: “Even a small drop in vaccine coverage can have a big impact on population immunity levels and lead to an outbreak.” This comment follows the discovery in February 2022 that one in 10 school-age-starting children in the UK are at risk of contracting measles.
Gaps remain for adults and adolescents
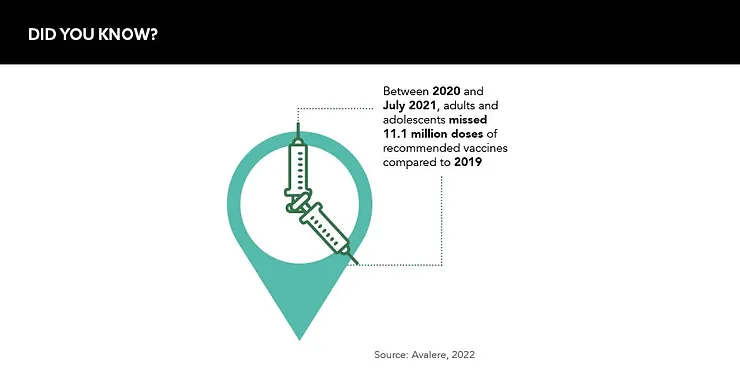
Vaccination rates for adolescents and adults were also knocked down to dangerous levels during the pandemic. A 2021 study by Avalere revealed that 11.1 million doses of recommended vaccines were missed between 2020 and mid-2021 compared to 2019. But while rates in children are starting to recover, Stewart admits: “That’s not happening with adolescents, and it is really not happening with adults.”
For example, in the UK, the uptake of the HPV vaccine improved between 2020 and 2021 compared to their level in 2019, but they are still not back up to the levels seen pre-pandemic.
Even a small drop in vaccine coverage can have a big impact on population immunity levels and lead to an outbreak
Theories for why vaccine rates in these age groups have sharply fallen and stagnated include the disruptive nature of COVID-19. During the peak of the pandemic, many adults acquired extra burdens, such as childcare, alongside their professional responsibilities, leaving less time to focus on their own wellbeing, and there are fears that this has stuck.
“COVID-19 has had a profound impact on daily lives and, as a result of that, many people have had to delay non-emergent healthcare, including routine preventive services such as vaccines,” affirms Christine Liow, Associated Principal, Avalere Health.
In addition, the multiple-dose COVID-19 cycles may have led to vaccine fatigue, and the swelling of disinformation around vaccines for the virus could be acting as a dangerous deterrent. “There are some analyses that show vaccine hesitancy is a factor,” reasons Peacock. But agreeing with Liow, she adds: “The biggest factor is likely the disruption of the pandemic on our daily lives.”
What next?
For the pharma industry, a solution to declining routine vaccine rates could be to make better use of existing vaccination seasons, adding in more vaccines around the typical flu season shots, but Stewart warns: “We can’t keep trying to jam all the adult vaccinations that are needed and recommended into a three- or four-month period. It’s just not operational; people aren’t going to want to do that.” This would also do little for solving the gap in adolescents who are not traditionally entitled to a flu vaccination.
What is certain is that the entire health ecosystem must collaborate on public health awareness campaigns, injecting a sense of urgency into adults and young people to get themselves, and those in their care, vaccinated. Otherwise, recovery rates will be too incremental, and the risk of outbreaks will continue to rise with potentially devastating consequences. It is time to heal this particularly deep wound of the pandemic and focus on restoring the world’s defences against preventable conditions before it is too late.
The competitive edge
One of the biggest challenges facing the routine vaccination space is a lack of competition within approved vaccines for many preventable diseases. For example, in the US, Merck & Co. is the sole manufacturer of an approved vaccine for measles, mumps and rubella.
The issue is twofold: economic and a matter of public safety. Judy Stewart, Senior Vice President and Head of US Vaccines, GSK, says: “The safest place for a government and market to be is when they have options to choose from.” Indeed, from a safety perspective, having a range of vaccine manufacturers for every disease area can prevent supply and capacity issues that could lead to a drop or even cessation in vaccine access.
As money is poured into vaccine development in the wake of COVID-19, it will be critical for companies to not only develop solutions for currently incurable diseases, but also focus on those for which solutions already exist. To this end, Stewart adds: “That’s what’s best for communities and public health – when you have choice.”









