Abstract
The objective of this study is to assess obstetric complications, blood loss, blood transfusion requirement, and maternal and fetal outcomes associated with the authors’ approach of Caesarean hysterectomy for placenta accreta spectrum disorders. Data were collected from case records of all females who underwent Caesarean hysterectomy between August 2013–August 2023 at Lifeline Multispeciality Hospital, Adoor, Kerala, India. There were 19 cases of Caesarean hysterectomy. The mean age was 33.63±2.90 years. Mean blood loss during surgery was 1.11±0.16 L, and the mean packed red blood cells transfused was 2.00±0.38 units. The mean gestational age of termination was 33 weeks and 5 days, and mean birth weight was 2.28±0.21 kg. There were no maternal or neonatal deaths. Placenta accreta spectrum should be managed in a multidisciplinary setup with the involvement of a senior experienced obstetrician. Early, careful bladder dissection before proceeding with hysterectomy will help in reducing haemorrhage, and in accelerating hysterectomy.
Key Points
1. Whilst rare, the incidence of placenta accreta spectrum disorders (PAS) is rising. Life-threatening haemorrhage can occur as a result of PAS; therefore, optimised understanding and management is crucial for patient outcomes.2. This case series reviews records from patients with PAS who were managed with Caesarean hysterectomy, to review complications and maternal and fetal outcomes. The study highlights that correct pre-operative diagnosis by ultrasound or, if needed, MRI, is important for informed surgical planning, which should be performed in a multidisciplinary setting by an experienced team to reduce morbidity and mortality.
3. Intra-operative blood loss is a complication that can be greatly reduced by initial meticulous dissection of the bladder prior to hysterectomy. This also reduces the duration of procedure, especially in the region of the lower segment.
INTRODUCTION
Placenta accreta spectrum (PAS) is rare, but its incidence is increasing due to a rise in Caesarean section rates.1,2 PAS is an abnormal trophoblastic invasion into the myometrium, up to the serosa, or more.2 This condition can lead to life-threatening haemorrhage, and usually requires hysterectomy. The severity of invasion can be graded according to the International Federation of Gynaecology and Obstetrics (FIGO) classification.3 Primary risk factors include prior uterine surgery, prior surgical termination, and in vitro fertilisation.2 Caesarean hysterectomy (CH) is the definitive treatment, and should be performed in a multidisciplinary care centre by a senior experienced obstetrician. However, there are various methods to reduce blood loss, such as aortic balloon occlusion, aortic clamp, and pre-operative insertion of embolisation catheter.2,4 Even then, the blood loss and need for blood transfusions are found to be high. The objective of this study is to assess the demographic parameters, obstetric complications, blood loss, blood transfusion requirement, and maternal and fetal outcomes associated with the authors’ approach of CH for PAS disorders, in a single centre.
MATERIALS AND METHODS
This is a case series of all females who underwent CH between August 2013–August 2023 at Lifeline Multispeciality Hospital, Adoor, Kerala, India. The authors collected data from all case records of patients who had CH during this period. Nineteen cases of CH were retrieved, informed patient consent was taken from these females, and their data were analysed. Maternal demographic variables, comorbidities, gestational age, obstetric score, risk factors, pre-operative and post-operative haemoglobin levels, blood loss, blood transfusion details, surgery details, maternal outcome, fetal outcome, and maternal and fetal complications were collected from case records. A data abstraction sheet was used to extract details, and data was entered in an Excel sheet (Microsoft, Redmond, Washington, USA). Data were summarised as numbers and mean with standard deviation and percentages.
CH was performed by vertical midline skin incision (Figure 1A), followed by a vertical incision in the upper segment of the uterus, above the placental edge. After the fetus was delivered (Figure 1B), they were handed over to the paediatrician. The uterus was exteriorised, and uterotonics, including oxytocin and methergine, were used. Tranexamic acid was used to reduce bleeding.5 Methergine was not given to four patients who had hypertension. Since the edges did not bleed significantly after delivery of the fetus, they were not sutured. The maximum blood loss occurred when the uterus was severed in the region of the lower segment and cervix, where the placenta is attached. Hence, it was important to accomplish this suturing step as fast as possible. With this in mind, the authors routinely dissected the bladder in small steps, and brought the bladder below the lower edge of the placenta. In cases where bleeding was higher during bladder dissection, bilateral internal iliac artery ligation was performed (Figure 1F), followed by total hysterectomy (Figure 1A–H). Blood loss was assessed by weighing the mops used and measuring the amount of blood in the suction apparatus. All procedures were performed by the same senior obstetrician, in a multidisciplinary setup.
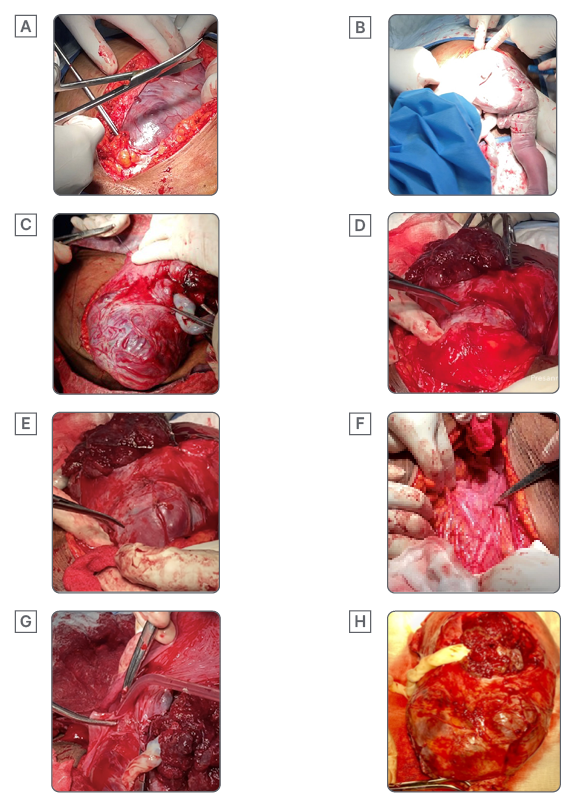
Figure 1: Caesarean hysterectomy steps.
A) Midline vertical incision. B) Delivery of fetus. C) Uterus after delivering the fetus, showing the lower segment bulged with placenta. D) Bladder dissection. E) Lower segment with bulging placenta after dissecting and pushing down the bladder. F) Exposed internal iliac artery. G) Hysterectomy. H) Hysterectomy specimen with placenta in situ.
RESULTS
Over the 10-year study period, there were 19 cases of CH performed for PAS disorders. There were four referred cases from other hospitals. Seventeen cases were diagnosed antenatally by ultrasound, and two cases were diagnosed intraoperatively, which were referred in labour without diagnosing PAS. These patients underwent CH in the authors’ centre, where PAS was diagnosed. The mean age of patients was 33.63±2.90 years. Other demographic variables are given in Table 1. Previous Caesarean sections, in vitro fertilisation, previous myomectomy, and curettage were the common risk factors. The mean gestational age of termination was 33 weeks and 5 days, and a total hysterectomy was performed for all cases. Internal iliac artery ligation was performed for eight cases (Table 2). One case was FIGO 3C, for which intraoperative stenting was performed. Two cases were FIGO 3A, and bladder injury occurred in these cases. Hysterotomy followed by hysterectomy was performed in one case at 23 weeks and 2 days, which was terminated for multiple congenital anomalies, and the fetus passed away soon after birth. Mean blood loss during surgery was 1.11±0.16 L, and mean packed red blood cells transfused was 2.00±0.38 units (Table 2). The mean pre-operative haemoglobin was 11.36±0.42 g/dL, and mean postoperative haemoglobin was 11.18±0.69 g/dL. There were no neonatal deaths, and mean birth weight was 2.28±0.21 kg. In total, 57.89% of neonates required neonatal intensive care unit admission for low birth weight and preterm care. There were no maternal deaths, and none of these cases required intensive care management or massive blood transfusion. Only 21% of cases required more than two blood transfusions. The mean duration of postoperative stay was 11.94±2.79 days, as patients stayed until sutures were removed. All specimens were sent for histopathological examination, and increta was confirmed. A summary of cases is included in Table 3.
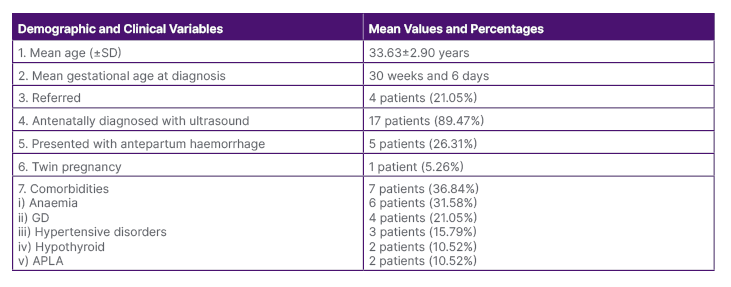
Table 1: Patient demographic and clinical variables.
APLA: anti-phospholipid antibody; GD: gestational diabetes; SD: standard deviation.
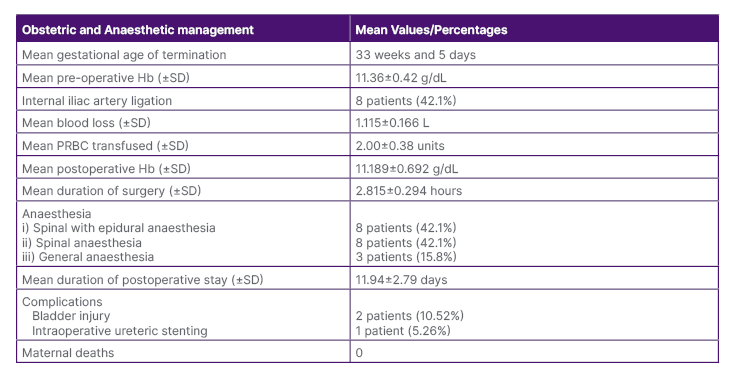
Table 2: Patient obstetric and anaesthetic management.
Hb: haemoglobin; PRBC: packed red blood cells; SD: standard deviation.
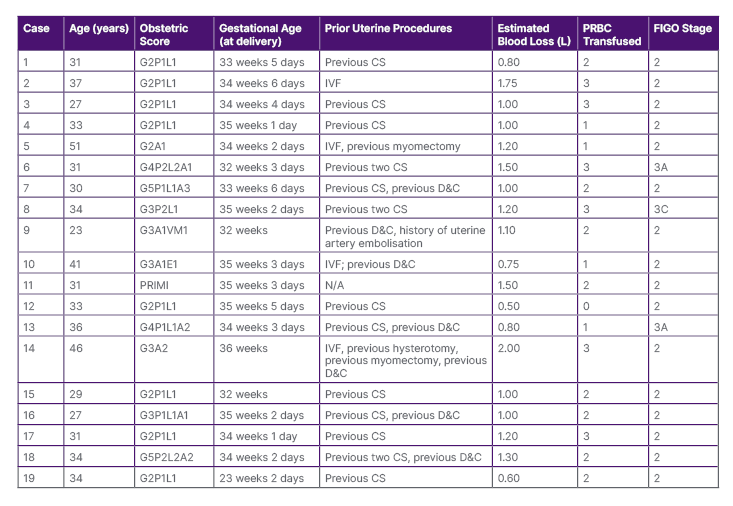
Table 3: Summary of patient cases.
CS: caesarean section; D&C: dilation and curettage; FIGO: International Federation of Gynaecology and Obstetrics; G,P,L,A,VM: gravida, parity, live, abortion, vesicular mole; IVF: in vitro fertilisation; N/A: not applicable; PRBC: packed red blood cells; PRIMI: primigravida.
DISCUSSION
Over the 10-year study period, there were 19 cases of PAS disorders, for which CH was performed. The mean age group in this study was 33.63 years, which was comparable to the mean age of 32.70 years reported by Dandolu et al.6 There is an increase in the risk of PAS with advanced maternal age.2 The mean gestational age in the study by Ansar et al.7 was 33.84 weeks, comparable to the mean gestational age of 33 weeks and 6 days in this study.
The most common risk factor in the study by Dandolu et al.6 was previous Caesarean (47.37%), followed by prior history of curettage (15.80%). The authors’ study identified multiple risk factors, and the most common was previous Caesarean section (68.42%). The risk factors for each case are mentioned in Table 3. In this study, one female had no risk factors. She was a primigravida, and hysterectomy specimen histopathology found placenta increta. In this study, 13 cases were FIGO Grade 2 (84.2%), followed by FIGO Grade 3 (15.8%). Blood loss and requirement for blood transfusion were lower in this study compared to the study by Ansar et al.7 Mean blood loss and mean packed red blood cells transfused in this study were 1.11±0.16 L and 2.00±0.38 units, respectively, compared to 2.60 L and 7.76 L in the study by Ansar et al.,7 which are much higher. In the study by Paily et al.,8 aortic clamp was used, and the mean blood loss was 1,000±1,500 mL. The correct surgical technique involves a right plane of bladder separation, without touching the placenta; this is a core step to reduce haemorrhage and associated complications. Bladder dissection should be initially performed, so that hysterectomy at the lower portion, where the placenta is situated, can be accomplished more quickly to reduce haemorrhage.
Methods to control haemorrhage include internal iliac artery ligation, aortic balloon, embolisation, and aortic clamp.2,4 In the authors’ study, internal iliac artery ligation was performed in eight cases (42.11%).
The mean birth weight in this study was 2.289±0.217 kg, which was comparable to the mean birth weight of 2.40±0.95 kg in the study by Ansar et al.7 In this study, 57.89% of newborns required neonatal intensive care unit admission, which was for pre-term and low birth weight care. None required ventilator support.
Panaitescu et al.9 stated that, in the case of conservative management of PAS, one in three patients will still require hysterectomy after expectant management. Expectant management requires long term follow-up, carries risk of complications, and at any time can become an emergency, with patients requiring lengthy hospital stays.
There were no maternal or neonatal deaths in the authors’ study, none required intensive care monitoring, and there were no postoperative complications. Early diagnosis and management of PAS disorders in a planned multidisciplinary setup, and hysterectomy by an experienced obstetrician, will reduce maternal morbidity and mortality.
CONCLUSION
CH is the standard approach for PAS disorders. The most common risk factor for PAS is previous Caesarean section. Proper pre-operative diagnosis and management in a multidisciplinary setup by a senior skilled obstetrician reduces morbidity and mortality. Early bladder dissection before proceeding to hysterectomy will reduce blood loss, and hence allow faster completion of hysterectomy.







