Interview Summary
The intricate relationship between climate change and air pollution is having a significant impact on public health. Increases in global temperatures are leading to extreme weather events, changes in plant growth patterns, and higher levels of aeroallergens and air pollution; all of which can exacerbate pre-existing respiratory conditions and increase the risk of developing respiratory and other diseases. In this article, four world leaders in the field of respiratory health outline the evidence linking climate change and air pollution to poor respiratory health outcomes. They highlight that people living with lung conditions, such as asthma and chronic obstructive pulmonary disease (COPD), as well as pregnant people, children, older people, and those living in low- and middle-income countries (LMIC), are the most at risk. They emphasise the need for greater awareness among the public and healthcare professionals alike, talk about the role of healthcare teams in helping people to recognise and mitigate the risks, and share practical ways people can help to minimise the health impacts of climate change and pollution.INTRODUCTION
Climate change is happening, with the evidence clearly demonstrating an increase in global temperatures; extreme weather events; and levels of air pollution, aeroallergens, and airborne pathogens.1,2 The complex interplay between these various factors is changing the quality and composition of the air we breathe, directly aggravating pre-existing respiratory diseases and increasing everyone’s exposure to their risk factors.3 “This is happening and we need to prepare for it,” said Fan Chung, Professor of Respiratory Medicine and Head of Experimental Studies Medicine at the National Heart and Lung Institute, Imperial College London, UK; and Consultant Physician at the Royal Brompton and Harefield NHS Trust, London, UK.
It is now widely accepted the Earth’s climate is changing, due to the burning of fossil fuels resulting in the generation of greenhouse gases (GHG).4 The global atmospheric CO2 concentration, for example, has increased from pre-industrial levels (1850–1900) of approximately 280 parts per million, to 415 parts per million in 2021.2 Such GHGs become trapped in the planet’s atmosphere, and create a warming effect. Chung said: “There is already evidence that this is happening. The World Meteorological Organization (WMO) has said that 2023 was another record year for temperatures.”5 Higher global temperatures mean more extreme weather events, such as flooding, drought, and wildfires, as well as changes to how plants grow.3 Professor of Paediatrics at the Chinese University of Hong Kong, Shatin, Hong Kong, Gary Wong, explained: “When we burn large amounts of fossil fuels, it releases GHGs that change the atmospheric composition and leads to gradual increases in the overall temperature. This has subtle trickle-down effects on plant growth: they have longer growing seasons and they generate more pollen.3 Taken together, it means we have more pollutants and more pollen in the atmosphere.” The changing composition of air also influences the way airborne pathogens, such as viruses and bacteria, behave in the air and access human bodies.
CLIMATE CHANGE AND HEALTH
The complex interplay between increasing global temperatures and air pollution is having an important impact on public health. The Intergovernmental Panel on Climate Change has projected a significant increase in climate-related ill health and premature deaths in the coming years, estimating excess deaths of 250,000 a year by 2050.2 However, there is clear evidence to show that decreasing air quality and climate change are already impacting the world’s respiratory health.1 Christopher Carlsten, Director of the Centre for Lung Health and Legacy for Airway Health (LAH), Vancouver, Canada; and Professor of Respiratory Medicine at the University of British Columbia, Vancouver, Canada, said there was no one way to quantify the impact of climate change on health. Though imperfect, he said that the easiest way is to “break it up into its parts,” by looking at the “effects of particulate matter (PM), toxic gases such as ozone, temperature, and allergens, to name but a few.” Each of these generally increase as the climate warms, and their interaction can have compounding effects.
Pollution and Particulate Matter
Sundeep Salvi, Director of the Pulmocare Research and Education (PURE) Foundation in Pune, India, and winner of the 2024 American Thoracic Society (ATS) World Lung Health Award, explained that climate change and air quality were “very intricately connected.” “A human being breathes 10,000 litres of air a day,”6 he said. “The air we breathe comes into close contact with a very large surface area in the lung, around the size of a tennis court, where the gas exchange takes place,” he said. “The gas exchange portion of the lung surface is very sensitive and very thin, so if polluted air, hot air, or cold air reaches that, it is going to have an adverse effect.”
An estimated 50% of all childhood pneumonia deaths, for example, are connected to air pollution, with the highest concentrations of mortality being found in LMIC.7 In addition, air pollution has been found to be the most important driver of COPD in India, being responsible for more burden than smoking.8 While asthma is largely recognised to be a genetic disease, the environment has a “very important and perhaps equal contribution,” Salvi said.9 “If you live in a polluted environment, you’re at risk of developing these conditions.9 If you have underlying asthma or COPD and live in a polluted environment, you’re going to get repeated exacerbations,” he added.9
With the burning of fossil fuels producing both GHGs and pollutants, climate change and air pollution are intrinsically linked.1 PM refers to everything in the air that is not gas, and consists of a wide variety of chemical compounds, organic matter, and other materials.10 Scientists tend to classify these particles according to their size.10 PM10, for example, are particles of less than 10 µm in diameter, PM2.5 are particles of less than 2.5 µm, and PM1 are particles of less than 1 µm.10 Chung said: “The size is important because the small ones can travel deep into the lungs.” Particles >5 μm reach and are deposited mainly in the proximal large airways, and then removed via mucociliary clearance; whereas, those <5 μm will reach, and are deposited, in the small airways and alveoli.11 Studies have suggested that 83% of PM2.5 are deposited in the lung, compared to just 31% of PM with a diameter of less than 11.5 μm.11 “PM can contain various carbon-like substances, metals, organic material, and plastic nanoparticles, and many can have a toxic-type effect,” Chung explained. In 2019, PM2.5 was responsible for an estimated 6.7 million deaths worldwide, including 373,000 in Europe.1
PM has many known effects across the respiratory system. “You can visualise it going from the nose to the bottom of the lungs: from the nasal passages at the beginning of the upper airway, through the pharynx, the larynx, through the bronchial tree, and all the way down to the alveoli,” Carlsten said. “Every known respiratory condition or disorder along that pathway has been demonstrated, in one way or another, to be affected by PM.” 7,8,9,12-14 (see Table 1)
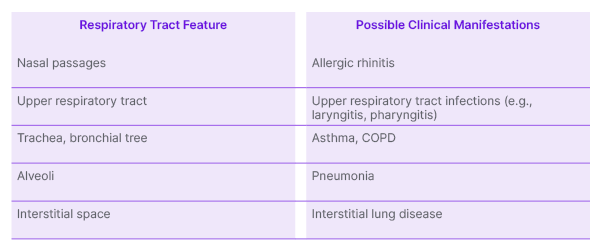
Table 1: Potential health impact of particulate matter by respiratory tract feature.7,8,9,12-14
COPD: chronic obstructive pulmonary disease.
It does not stop, however, with the respiratory system, Salvi explained. “A lot of the pollutants that enter the lungs go on to enter the circulation, and get transported to all the organs of the body.15 They get deposited in the brain, in the kidney, the bowel, and so on,” he said, highlighting his recent study that teenagers living in the polluted city of Delhi, India, had a high prevalence of not only asthma and respiratory symptoms, but also allergic rhinitis, eczema, and high BMI.16 This, he went on, was a new and important finding that warrants further investigation.
As well as PM, air pollution can also contain gases, including nitrogen oxides (NOx), carbon monoxide, sulphur dioxide, and ground-level ozone, an irritant that is promoted by sunlight exposure and higher temperatures.1,17 “All of these tend to irritate the airways,” Wong said. “Without underlying disease, it can result in respiratory symptoms, such as cough and phlegm.3 But for those living with, for example, asthma or COPD, it can irritate the airway so much that it makes the pre-existing inflammation worse. That’s why, when the level of pollutants rise, we see exacerbations.”18
Where Does Particulate Matter Come From?
Various factors are associated with higher levels of PM. Carlsten explained that diesel exhaust particles (DEP) have typically been the most common contributor to ultrafine particles (<0.05–0.10 μm), at least in urban environments. DEP contains a complex mixture of particles and gases including carbon monoxide, NOx, sulphur dioxide, hydrocarbons, formaldehyde, transition metals, and carbon particles.11 It is the size of PM found in DEP, however, that scientists believe accounts for its systemic effects, which include increased carcinogenicity, the potentiation of autoimmune disorders, alterations in blood coagulability, and increased cardiovascular disorders.11 “In some ways, DEP are the most concerning of the particles because of how deep they get into the lungs,” Carlsten said, but extreme weather events, such as wildfires and sandstorms, also generate high levels of dangerous PM that can travel thousands of kilometres from their source over days or even weeks.1,19,20
Indoor pollution is another important area for consideration, particularly in areas of the world that use coal or biomass fuel. Worldwide, more than three billion people use traditional cookstoves that burn wood, animal dung, or crop residues to cook food or heat water.21 Wong said: “When you are biomass fuel in an enclosed area, all the pollutants are trapped inside the home environment. It is very common in India, Africa, and Latin America.” In addition, many people in tropical parts of the world routinely use products such as mosquito coils and agarbatti incense, Salvi said. “Our research has shown that burning one mosquito coil for 6 or 7 hours exposes people to the same amount of pollution as smoking 100 cigarettes,” he said.22
In high-income countries, much indoor pollution, Chung said, was “leakage” of outdoor pollution into the home, while the rest was the result of cooking and cleaning products.17 “We might not necessarily think of this as a climate-related phenomenon, but it’s more related than one might imagine,” Carlsten said. “The higher the outdoor air pollution, the higher the indoor air pollution because homes are far from being a complete barrier. The challenge of indoor air pollution becomes linked to climate change by virtue of the connection between the outdoor and the indoor worlds.”17
Temperatures
Increasing temperatures also have an adverse impact on mortality and morbidity.23 “The impact of temperature on health has been less extensively studied than that of PM,” Carlsten said, “but heat has been associated with increased mortality.” A recent study in England found that the risk of COPD hospitalisation increased by 1.5% per 1 °C increase in temperature, and attributed 1,851 events per year to temperatures above 23 °C.24 According to France’s public health body, Santé Publique France, the country recorded almost 33,000 heat-related deaths between 2014–2022, 28% of which occurred during heatwaves.25
While the mechanisms of this connection are still under investigation, the doctors said it was likely related to the impact of impaired thermoregulation.23 Wong explained: “We are warm-blooded animals and we need to keep our body temperature in a very narrow range. When we get too hot, we reduce our body temperature by breathing faster and drinking more water. If someone already has borderline lung function, this will likely stress the respiratory and cardiovascular systems.”
Aeroallergens and Allergies
Climate change has also been associated with an increase in allergic manifestations, including allergic rhinitis and asthma.2 Higher temperatures mean longer pollen and fungal spore seasons, and, when combined with increasing CO2 concentrations, higher levels of airborne allergens and higher pollen allergenicity.2 The interactions between aeroallergens and air pollutants, including PM, also play a role with some pollutants being able to alter the immunogenicity of allergenic proteins.2 “Climate change means longer summers, so high pollen levels for longer, and there is evidence to suggest the allergenicity of pollen may increase,”2 Chung said. “It means there is a possibility that more people will develop a pollen allergy, because more people will be exposed to it.” Studies have also suggested that diesel exhaust contributes to an increasing prevalence of allergies, with DEPs being shown to act as adjuvants that increase the sensitisation response in some experimental models.11
“Allergens have a huge impact on quality of life, through rhinitis and other allergic conditions,” Carlsten said. “We often think of exacerbations of allergic disease as things that are inconvenient, but not deadly, like a runny nose, but they’re also a risk factor for mortality.” Thunderstorm asthma, or asthma exacerbations linked to high winds drawing higher levels of and pollution particles into the air, is one example of how climate change can have a potentially devastating impact.26 “Pollen particles are usually quite big, so they can’t get into the body, but thunderstorms break them down to the PM2.5 size, enabling them to get deep into the lungs,” Chung said.27 Thunderstorm asthma, Wong went on, is particularly dangerous because it can affect people who do not have asthma, with one study finding 65% of people with seasonal allergic rhinitis experienced it.28 They have never learnt to recognise the symptoms, meaning they do not necessarily understand how to manage the symptoms with an inhaler, or when to seek help,” he explained. In 2016, a thunderstorm asthma event in Victoria, Australia, led to 3,365 people presenting to an emergency department with acute respiratory symptoms.29 From these presentations, 476 asthma-related hospital admissions occurred, equating to a 992% increase in typical asthma-related hospital admissions.29 Thirty-five people were admitted to an intensive care unit and 10 died.29
Climate Change and Infections
In addition, climate change can enhance the spread of vector-borne diseases. Rising temperatures and higher precipitation can directly affect the life cycles of pathogens, and change their habitats and environments. While the climate change-related increase in infectious diseases has not yet been quantified, studies have shown, for example, that the incidence of water and vector-borne diseases such as malaria and dengue fever are very much influenced by changes in the climate and environment.30
As temperatures and rain levels continue to rise, this could pose a challenge worldwide. Wong said: “Singapore is a tropical country, with the same temperature, humidity, and so on throughout the year. In that atmosphere, there are various bacteria and fungi that we know could cause trouble if inhaled into the lungs. If we are moving towards a climate that is more like Singapore’s in London, for example, we might move towards that same kind of ecology.” The consequences, he went on, could be felt by people with pre-existing respiratory disease, as well as the general population.
CLIMATE CHANGE AND SUSCEPTIBLE POPULATIONS
Taken all together, then, climate change is changing the air that we breathe. Chung said that increased humidity, higher temperatures, and increased ozone is affecting the way PM, pollen, and organisms behave in the air, and how they access and act in our bodies. “Anything that travels with the PM2.5, including micro-organisms, can ‘piggyback’ on the particles and get deep into the lungs,” he explained.31
Everyone’s health, at least to some extent, is at risk from the health impact of climate change, but those with pre-existing respiratory issues are in the greatest danger.1
“By definition, those with pre-existing COPD, asthma, and interstitial lung disease, etc., are the ones at greatest risk of exacerbations. That is obvious,” Carlsten said. “But who is at risk for new disease? That is a much more complicated question than most people appreciate.”
Air pollution causes 8.34 million excess deaths every year.32 “What characterises these people who are at risk of dying from pollution, and makes them different to the other 30 or 40 billion people in the world who do not die from pollution?” Chung asked. The answer, he said, is likely to be linked to personal factors. His team has just completed a study in which people wore sensors to measure their own personal levels of exposure to PM10, PM2.5, and PM1. “We found that it really depended on lifestyle, and the level of exposure varied from person to person. Even two people living at the same address can have very different exposure levels because of the different ways they travel, their workplace, the places they go to, etc.,” he said (unpublished data; Chung, F).
In general, however, the current literature shows that, aside from those with pre-existing medical conditions including cardiorespiratory disease, it is pregnant people, children, and older people who are most at risk. Socioeconomic factors can also play a role.1
Pregnant People
Prenatal exposure to air pollution has been linked to infant and child lung function impairment, an increase in respiratory symptoms, and the development of childhood asthma.33 It may also be indirectly linked to early birth, low birth weight, and impaired development of the immune system.34 “It is important to appreciate that the health effects of air pollution start even before you are born,” Salvi said. “The quality of air the mother breathes is going to decide the quality of nutrients the baby receives in the womb.”
Children
Children are at both acute and chronic risk of the effects of air pollution, due to their behaviour, their physiology, and their environment. Their lungs and immune systems are still developing, they tend to spend more time being physically active outside, and they breathe two to three times faster than adults; meaning they can inhale more polluted, hot, or aeroallergen-containing air, Salvi explained.1 There are data to suggest, for example, that children exposed to higher levels of PM2.5 are more likely to develop asthma and persistent wheezing than children who are not.34 Such asthma exacerbations can be extremely dangerous. In December 2020, the UK became the first country to list air pollution exposure as a cause of death after a 9-year-old girl who lived on a busy road in London, UK, died following an asthma attack. An inquest heard she had experienced a lifetime of exposure to excessively high levels of a traffic-derived mix of nitrogen dioxide and PM10, including non-exhaust sources of PM such as tyre and brake wear.35
Air pollution can also negatively impact the normal growth of lung function, and this can leave children vulnerable to respiratory disease later in life.36 Wong pointed to a study that showed that children who lived in more polluted areas of California, USA, had more impaired lung function, compared to those who lived in less polluted areas.36 “A small percentage reduction in lung function may not cause a big problem in terms of daily activity, but our lung function improves as we get older, and then starts to decline,” he said. “If you start with a lower peak, you are going to start feeling symptoms easier. Impaired lung growth reduces the maximum lung capacity of a healthy individual,”36 Salvi agreed. “There is a stunting of the lung growth that happens because of air pollution. Not only does that give rise to asthma or upper and lower respiratory tract infections, but it also makes children more vulnerable to developing COPD when they become adults.”
Older People
Older people are at increased risk from climate change in several ways. They are, for example, more likely to be trapped after extreme events such as flooding or drought, due to a lack of mobility, disability, or frailty.37 Their propensity for dehydration puts them at increased risk of heat-related illnesses, such as cardiac events, and they are particularly vulnerable to the pollutants and pathogens in the air.38 Salvi said: “As the immune system ages, the defences wear off, and the air pollutants they inhale will have a bigger impact.” Wong agreed, adding: “Older people with pre-existing lung disease or cardiovascular disease are much more prone to the effects of pollution, global warming, and climate change.”
Female Sex
There is also some evidence to suggest female sex plays a role in risk. A 2017 literature search, for example, suggested that females over the age of 65 years were more likely to suffer heat-related mortality than their male counterparts.39
Carlsten said the relationship between female sex and risk in the context of climate change “has not been adequately studied.” Increased risk among females, he went on, was likely to be related at least in part to their smaller respiratory tree, as compared to males, which could affect the deposition of pollution, he added.
Low- and Middle-Income Countries
People living in LMICs will “bear the brunt” of climate change and its health impact, Chung said. “A lot of people cannot pay for medical care, and they often live in places more affected by climate change; they experience more flooding, more forest fires, and so on,” he said. According the 2023 World Air Quality Report, Bangladesh, Pakistan, and India have the highest concentrations of PM2.5 of all 134 countries that collect data.40 Of his native country, India, Salvi said: “There is rapid urbanisation and industrialisation, and the number of motor vehicles has shot up.” In developed parts of the world, he went on, systems and policies are being put in place to combat climate change. “But in developing parts of the world, there is no way we can halt it because a country’s economic growth depends on how much they can manufacture.” In addition, females in LMICs are thought to be at high risk from the adverse respiratory effects of indoor pollution, as they tend to be the homemakers and therefore have high exposure to pollution generated by the burning of biomass fuel.41
PROTECTION AND MITIGATION
The evidence base is still evolving, and much more research is needed on the intricate interplay between climate change, pollution, and respiratory health, as well as the possible mitigation and resilience-building strategies. “There is a lack of research in the field of practical solutions: on things like wearing a mask, using nasal filters, saline nasal washes, and the use of antioxidants and dietary supplements,” Salvi said. “There are papers that seem to suggest they are effective, but we need more evidence to support that. The space is not mature.”21
However, all four doctors agreed that we understand enough to know that urgent action is needed. Chung said: “The problem is not in the distant future, the problem is here, now, on our doorstep, and it is just getting worse.” Greater awareness and education among the public, healthcare professionals (HCP), policymakers, and researchers alike is the “first and the most important intervention,” Salvi said. “Once that knowledge base is established, it’s a matter of disseminating and using it to offer advice to patients.” Raising awareness of the issues among hospital and healthcare systems is another important task, Carlsten added. “Broadly, healthcare systems tend to focus on the traditional challenges of capacity. Everything gravitates to the immediate crisis of the day. Yet, over time, these issues will impact those systems on a very obvious level, costing more money, and contributing to the busyness of emergency departments,” he said.
THE ROLE OF HEALTHCARE PROVIDERS
Asked if HCPs had a responsibility to help patients mitigate the risks of climate change, global warming, and pollution, Carlsten said it would be better described as an opportunity. “Healthcare professionals are supposed to do everything they reasonably can to promote health. They are also considered high on the spectrum of trust, so there’s reason to believe that their patients, and the community in general, will respect and listen to what they say,” he went on. Due to the “intuitive relationship between the air we breathe and the lungs,” respiratory specialists have been at the forefront of educating patients so far, but with pollution and climate change affecting every system in the body, there is an opportunity for all HCPs to become involved.
HCPs are already aware of, and have contact with, those people who are at greater risk from climate change and pollution. They are “at the forefront of the health battle,” Chung said. “I think it’s something that needs to be raised at each visit, particularly for those people suffering from chronic conditions. Pregnant people, children, older people, and so on, need to be informed of the risks.” While it is not the job of physicians to tackle climate change, Wong said that they were in the perfect position to identify at-risk individuals, and provide them with the information they need to mitigate the effects of climate change and pollution.
Healthcare providers can:
- identify at-risk populations;
- educate patients on the risks climate change poses to their health;
- educate patients on the mitigation strategies people can follow to protect their health from climate change; and
- support patients to implement the necessary changes.
Offering Solutions
While we wait for the evidence base to mature, there are certain “working solutions” that HCPs can recommend, Salvi said. In 2020, he, along with Carlsten, Wong, and Chung, published ‘Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public’.21 The paper reviewed the literature on a number of personal strategies aimed at reducing exposure to outdoor or indoor air pollution, and made recommendations based on the strength of the evidence (Table 2).
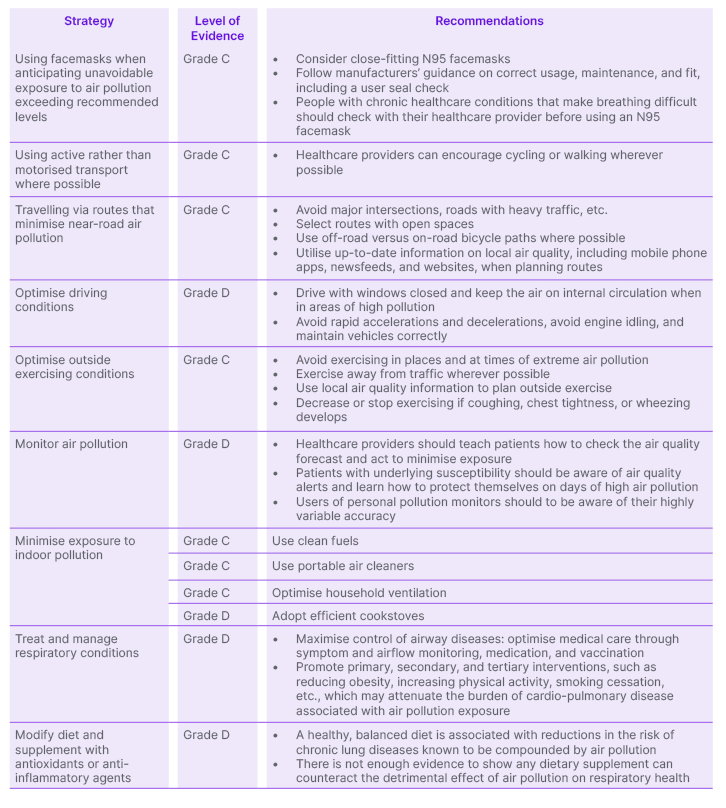
Table 2: Personal strategies to mitigate the impact of air pollution on respiratory health.21
Grade A: Rich body of evidence based on randomised controlled trials and/or meta-analyses; Grade B: Limited body of evidence based on randomised controlled trials and meta-analyses; Grade C: Body of evidence based only on non-randomised trials or observational studies; Grade D: Panel consensus judgement only.
It also argued that HCPs need to receive the most up-to-date evidence and information.21 “HCPs need to be aware of the depth of knowledge on air pollution, climate change, and human health. Next, they need to give potential simple, practical, affordable, sustainable, and effective solutions to the patients they see in the clinic,” Salvi said. Wearing a mask on polluted days and using saline nasal washes to clear pollutants that become trapped in the nose, for example, may be of some benefit.21
Preparedness was an important theme, and the doctors recommended HCPs advise patients to learn how to access local air pollution information. They can then use these data to plan where and when they exercise, or plot alternative, less polluted routes when commuting or travelling. Ensuring all patients have an up-to-date action plan that considers the impact of air pollution, and explains what to do when they experience an exacerbation, is important. Likewise, in areas at high risk of extreme weather events, whether that’s wildfires, flooding, or heatwaves, HCPs can work with patients to ensure they are prepared. Carlsten’s team, principally Emily Brigham, University of British Columbia, Vancouver, Canada, has developed an action plan checklist for wildfire smoke and extreme heat event readiness.42 Designed to be completed during clinic, it ensures people know how to check their local air quality, how to recognise potentially dangerous levels of heat and pollutant exposure, when to act, and how to minimise the risks.42,43
At the same time, however, HCPs need to be careful not to add to anxiety, the doctors said. “We don’t want everything to be doom and gloom, and for people to feel like they have to lock themselves up during any kind of pollution event. We have to balance the very real evidence about the serious health effects with the need to exercise, be outside, socialise, and be connected to nature,” Carlsten said. The next phase of research, he went on, will be to understand how to build resilience to the changes that are already happening. “Scientifically, we’ve got the methodologies and resources to do the analyses and publish the papers on all the bad things that are happening, but there’s a lot less work going on looking at how we can manage these, and not be so anxious about it all the time. Part of what I am trying to focus on is what we can do together to build the strength and capacity we will need to withstand this threat.”
TIME TO ACT
The doctors concluded that the complex interplay between climate change, air pollution, and respiratory health presents a significant challenge, and that urgent action is needed to address the impact of these factors, particularly on vulnerable populations. While the evidence base is still evolving, there are practical solutions and mitigation strategies that HCPs can recommend to minimise exposure to outdoor and indoor air pollution, as well as extreme-weather-related ill health. Greater awareness, education, and preparedness are essential, they agreed.
“It is absolutely crucial” to take action, Salvi concluded. “I am worried the next generation is going to be more vulnerable, so we need to be very, very serious about this.”







