Abstract
Advancements in novel combination immunotherapies as well as innovative downstream management courses offer great optimism for the applicability of emerging cancer immunotherapy to prospective treatment of cold tumours. This review comprehensively analyses and discusses notable current research directions in the field and underscores future directions for continued scientific progress alongside relevant clinical applications. Vitiligo is an autoimmune disorder characterised by white depigmented cutaneous macules. Although vitiligo may generally be considered a cosmetic disease, literature has associated broader systemic comorbidities, including a higher risk for atherosclerotic events, dyslipidaemia, and cardiovascular risk. To the authors’ knowledge, this is the first systematic review that assesses the association between vitiligo and cardiovascular disease (CVD)/CVD-associated factors. Utilising the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, the authors searched PubMed and Scopus databases to identify studies available as of 30th June 2022, examining CVD and CVD-associated risk factors in patients with vitiligo. Of 2,553 articles, seven studies (four cross-sectional and three case-control), totalling 611 patients diagnosed with vitiligo (56.3% female), met the inclusion criteria for the authors’ review. Six studies suggested a significant association between patients with vitiligo and an increased risk for CVD via increased atherosclerotic events, constraint-induced movement therapy, plaque presence, dyslipidaemia, high-sensitivity C-reactive protein, oxidative stress, as well as decreased levels of vitamin D, calcium, zinc, and antioxidants. However, one study found that patients with vitiligo presented with fewer cardiovascular risk factors and increased levels of high-density lipoprotein. Although few studies indicated an increase in atherosclerotic risk due to elevated low-density lipoprotein-cholesterol and total cholesterol, contradictory high-density lipoprotein and total cholesterol levels in additional studies indicate the need for further investigation. Lastly, the association between vitiligo severity and CVD risk also indicated conflicting results. The authors’ small sample size restrained their ability to compare populations and incorporate racial and ethnic diversity to generalise their conclusions. Additional studies are required to comprehensively understand the association between vitiligo and the risk of CVD.
Key Points
1. Despite being primarily seen as a cosmetic condition, vitiligo has systemic implications which are frequently overlooked. The existing research regarding vitiligo’s association with cardiovascular disease (CVD) reveals contradictory results. It is important for dermatologists to understand vitiligo’s associated risk factors to provide comprehensive care, improve risk assessment, and guide treatment approaches for patients with vitiligo.
2. This review provides a summary of the current understanding regarding the association between vitiligo and CVD, including CVD-related risk factors. In total, seven case-control and cross-sectional studies were included in the analysis, and the results are presented.
3. This review highlights a reported emerging link between vitiligo and CVD risk factors. However, few studies also reported contradicting support when analysing vitiligo’s association with hypertension and lipid profiles, two known CVD-related risk factors. Therefore, more randomised controlled studies and future research is warranted to further examine this relationship.
INTRODUCTION
Vitiligo is an autoimmune disorder characterised by the loss of melanocytes, resulting in white, depigmented cutaneous macules. This disorder affects approximately 0.76–1.11% of adults in the USA, and has an estimated prevalence of 0.5–2.0% of the population worldwide.1,2 Although understanding the pathogenesis is still under debate, many hypotheses suggest metabolic abnormalities, oxidative stress, generation of inflammatory mediators, cell detachment, and autoimmune responses.3 Although vitiligo may generally be considered a cosmetic disease, literature has associated broader systemic comorbidities. A variety of comorbidities have been associated with vitiligo, including thyroid disease, alopecia areata, diabetes, systemic lupus erythematosus, rheumatoid arthritis, psoriasis, and atopic dermatitis.4 Additionally, patients with vitiligo demonstrated a higher risk for developing atherosclerotic events, dyslipidaemia, and cardiovascular risk.5
Cardiovascular disease (CVD) is a leading cause of death globally, and is a significant contributor to healthcare expenditure. In 2019, 32% of all deaths worldwide were attributed to CVD, totalling an estimated 18.6 million people.6,7 Although factors such as high-density lipoprotein (HDL) cholesterol, diabetes, and smoking have been used extensively in calculating risk for cardiovascular events, recent work has identified additional factors associated with CVD. Specifically, dermatologic conditions, such as psoriasis and hidradenitis suppurativa, have been linked to increased cardiovascular risk.5 Other conditions, including vitiligo, have received attention as they may share similar pathophysiologic mechanisms to CVD, and also may be linked to traditional CVD risk factors.5
To the best of the authors’ knowledge, this is the first systematic review that assesses the association between vitiligo and CVD. Previous research suggests that patients with vitiligo are at a higher risk of developing dyslipidaemia, atherosclerosis, and a potential increase in cardiovascular risk.5 Further, a case-control study suggests that vitiligo is significantly correlated with a family history of CVD.8 A recent systematic review and meta-analysis demonstrated an association between vitiligo and metabolic disorders such as diabetes mellitus, hypertension, and obesity via metabolic syndrome.9 However, other studies indicate contradictory results, where patients with vitiligo displayed lower cardiovascular risk than controls.10-12 Therefore, the authors conducted a systematic review of available case-control and cross-sectional studies to synthesise the evidence regarding the association between vitiligo and CVD and CVD-associated risk factors. Understanding this association is important due to the potential systemic impact of vitiligo beyond its cosmetic manifestations. The authors hope that this review can help clinicians direct screening strategies, risk assessment tools, and tailored interventions for patients with vitiligo to mitigate the risk of CVD in this population.
MATERIALS AND METHODS
Study Identification
The authors conducted a systematic literature search using PubMed and Scopus databases to identify studies available as of 30th June 2022. The search consisted of the following medical subject heading terms: “vitiligo” OR “non-segmental vitiligo” OR “segmental vitiligo” AND “cardiovascular disease” OR “cardiovascular risk” OR “CVD” OR “CVR” OR “atherosclerosis” OR “hypertension”. Additionally, the authors searched the reference lists of selected studies. This search was conducted adhering to the updated 2020 standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.13
Eligibility Criteria
Two reviewers independently selected studies that met the following inclusion criteria: observational studies, including prospective cohort, retrospective cohort, cross-sectional, and case-control; studies that examined the association of vitiligo with CVD or risk; and studies reported in English. Studies were excluded if all participants had metabolic syndrome. Any disagreement was reviewed by a third reviewer, and the final decision was made unanimously between the three authors.
Data Extraction
A total of 2,553 studies were screened, and seven were included. Information was collected regarding study design, location, data year range, cohort groups, number of subjects, average mean or range, sex, and risk for outcome metrics. All included studies and data collection information is presented in Table 1.
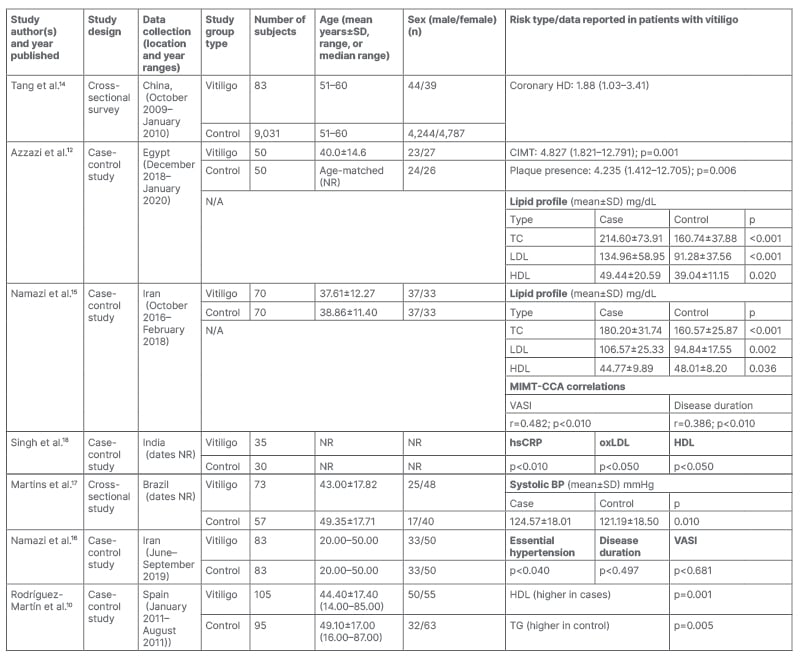
Table 1: Characteristics of included studies.
BP: blood pressure; CI: confidence interval; CIMT: carotid intima media thickness; CVD: cardiovascular disease; HD: heart disease; HDL: high-density lipoprotein; hsCRP: high-sensitivity C-reactive protein; LDL: low-density lipoprotein; MIMT-CCCA: mean intima media thickness of the common carotid artery; N/A: not applicable; NR: not reported; OR: odds ratio; oxLDL: oxidised low-density lipoprotein; TC: total cholesterol; TG: triglycerides; SD: standard deviation; VASI: Vitiligo Area Scoring Index.
RESULTS
The authors’ search strategy is illustrated by the flowchart in Figure 1. Their initial search resulted in 2,553 studies, and ultimately seven studies that met all three inclusion criteria were used for data collection and analysis (Table 1). Overall, four cross-sectional studies with a level of evidence of four, and three case-control studies with a level of evidence of three were included. Of the 611 patients with a confirmed diagnosis of vitiligo, the ages ranged from 8–85 years, with 56.3% females and 43.7% males. Dates for incorporated studies ranged from 2011–2022.
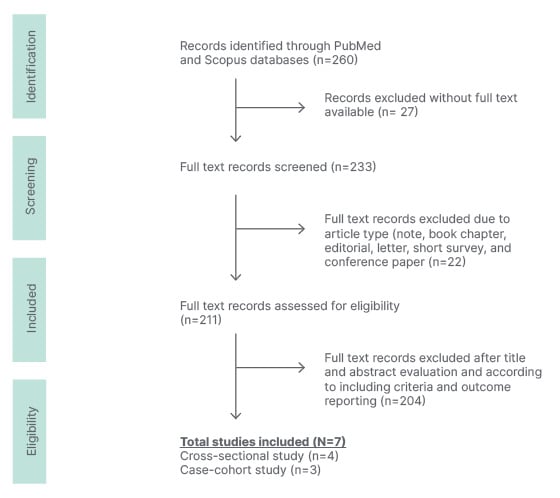
Figure 1: Flowchart for the selection of eligible studies included.
Six out of the seven studies directly support the positive association between vitiligo and CVD or CVD-associated risk factors. Tang et al.’s14 cross-sectional survey examined 83 non-segmental and segmental vitiligo patients for 3 months, and found that patients with vitiligo had an increased risk of coronary heart disease (adjusted odds ratio [OR]: 1.88; 95% confidence interval [CI]: 1.03–3.41.)14 In subgroup analyses, the increased risk was observed in participants ≥60 years (adjusted OR: 2.25; 95% CI: 1.13–4.47), and in overweight (BMI: ≥24 kg/m2) participants (adjusted OR: 2.45; 95% CI: 1.02, 5.88). In addition to CVD risk, Azzazi et al.’s12 recent case-control study utilised ultrasonography to demonstrate that patients with vitiligo had an increased carotid intima media thickness (CIMT; case: 0.6180±0.1900 mm versus control: 0.5250±0.2000 mm) and an increased presence of atherosclerotic plaques when compared to controls (p=0.001 and 0.006, respectively). Further, Namazi et al.15 measured a similar variable, mean intima media thickness of the common carotid artery (MIMT-CCA), and found that patients with vitiligo had a greater MIMT-CCA than healthy controls; however, this was not statistically significant.15 They also found no atherosclerotic plaques in any subjects, although significantly more patients with vitiligo displayed subclinical atherosclerosis (p=0.006).15
Further, four out of the seven included studies examined the association between hypertension, a CVD-associated risk factor, and vitiligo. Namazi et al.’s16 case-control study found that patients with vitiligo were diagnosed with hypertension more often than the normal population (p=0.040). In contrast, Tang et al.’s14 cross-sectional study found that the adjusted OR for hypertension in patients with vitiligo compared with healthy controls was 1.00 (95% CI: 0.61, 1.65).14 Similarly, Namazi et al.15 found no significant difference between systolic and diastolic blood pressures between patients with vitiligo and healthy controls (p value: 0.247 and 0.957, respectively). Although Martins et al.’s17 cross-sectional study showed no significant difference in hypertension between vitiligo and control patients, they did find significantly increased systolic blood pressures in patients with vitiligo (p=0.01).
Lastly, four out of the seven included studies examined the association between dyslipidaemia and vitiligo. Azzazi et al.’s12 case-control study found that patients with vitiligo had significantly higher low-density lipoprotein-cholesterol (LDL-C), high-density lipoprotein-cholesterol, and total cholesterol when compared with controls (p=<0.001, 0.020, and <0.001, respectively).12 Namazi et al.’s15 study also showed that LDL-C and total cholesterol levels were elevated in patients with vitiligo compared with controls (p=0.002 and p<0.001, respectively). Singh et al.’s18 case-control study found that patients with vitiligo had significantly increased levels of serum high-sensitivity C-reactive protein and serum oxidised LDL levels compared with healthy controls (3.9±2.3 mg/L versus 2.3±1.4 mg/L; p<0.01; 313.5±157.3 pg/dL versus 172.1±103.8 pg/dL; <0.05, respectively).18 Interestingly, only Singh et al.18 found elevated triglycerides levels in patients with vitiligo when compared to controls. Of note, both Namazi et al.16 and Singh et al.’s18 studies found that patients with vitiligo had significantly decreased levels of HDL compared with controls (p=0.036 and p<0.05, respectively),15 which is contrary to Azzazi et al.’s12 findings. Furthermore, another study by Rodríguez-Martín et al.10 indicated that patients with vitiligo had higher levels of HDL, lower levels of triglycerides, and no significant difference in LDL levels compared to healthy controls.10
DISCUSSION
Only Tang et al.14 directly supported the association between vitiligo with CVD risk, specifically among older and overweight individuals. The remaining six studies instead identified associations between vitiligo and CVD-associated risk factors, indicating that additional studies are needed to fully characterise the relationship between vitiligo and CVD.
Azzazi et al.’s12 study demonstrated an increased presence of atherosclerotic plaques compared with controls, concluding that patients with vitiligo displayed increased CIMT and a higher risk of developing clinical atherosclerosis, which is one of the predominant pathologic events predisposing patients to CVD. CIMT and an increased plaque presence are independent predictors of cardiovascular events,12,15 with studies demonstrating that an absolute increase of 0.1 mm in CIMT increases the future risk of myocardial infarction (MI) by 10–15%.19 Additionally, the presence of carotid plaques has been associated with an increased risk of coronary heart disease and CVD.20 Although Namazi et al.15 did not find a similar statistically significant result, they did demonstrate that patients with vitiligo displayed increased rates of subclinical atherosclerosis. Further studies with increased sample sizes and greater longitudinal data are required to draw conclusions regarding carotid intima thickness and its association with CVD outcomes in patients with vitiligo.
With postulations that vitiligo is a systemic disease, it is vital to assess whether there is a relationship between vitiligo severity and its systemic effects on CVD. Such a relationship could help providers optimise screenings for patients with vitiligo to minimise the risk for CVD. Although both Azzazi et al.12 and Namazi et al.15 found an increase in thickness of the carotid arteries in patients with vitiligo, they found contradictory results regarding the relationship between disease severity and CVD. Azzazi et al.12 did not find a significant correlation between CIMT and Vitiligo Extent Score (VES), Vitiligo Area Scoring Index (VASI), or vitiligo activity. However, Namazi et al.15 found that the MIMT-CCA correlated significantly with both the VASI score and disease duration in patients with vitiligo, suggesting that increased disease severity was associated with an increased risk for CVD (r=0.482; p<0.010, and r=0.386; p<0.01, respectively). Further studies that analyse the relationship between disease severity and duration are required to understand the severity of the systemic effects of vitiligo on CVD risk.
Additionally, Azzazi et al.’s12 study demonstrated significantly increased levels of oxidative stress, and decreased levels of total antioxidant capacity in patients with vitiligo compared with healthy controls. Since oxidative stress is deemed the common mechanism supporting atherosclerosis, the increased levels of reactive oxidative stress in patients with vitiligo may explain the increased risk of atherosclerosis.12,21 Further, vitiligo inflammatory markers including homocysteine, TNF-α, and IL-6 are mediators in atherosclerosis development, suggesting that vitiligo as a systemic disease could promote CVD risk.21
Patients with low levels of vitamin D and zinc have also been shown to be at an increased risk for CVD, including MI.22 Additionally, low ionised serum calcium levels can prolong the ST segment, a common manifestation of early MI. Rahman et al.22 found significantly decreased levels of vitamin D, zinc, and calcium levels in patients with vitiligo compared with healthy controls. Concurrently, levels of serum calcium showed a significant positive correlation with vitamin D levels, increasing the risk of MI in patients with vitiligo. Since these decreased levels of vitamin D, zinc, and calcium may make patients with vitiligo more prone to MI, it may be a valuable tool for providers to screen and manage patients with vitiligo to minimise their risk for MI.22 However, this would require further investigation to demonstrate its clinical utility in the management of patients with vitiligo.
Hypertension is a major contributor to the high prevalence of CVD.23 Four out of the seven included studies examined the association between hypertension and vitiligo. Of these studies, only Namazi et al.16 found a positive association, demonstrating that patients with vitiligo were diagnosed with hypertension more often than the normal population. As increased efflux of catecholamines has been proposed as a mechanism for vitiligo and hypertension, the authors suggested that the increase in plasma catecholamines in patients with vitiligo could lead to a higher predisposition to hypertension.16 However, they found no association between characteristics of vitiligo and hypertension, which may have been due to the presence of confounding factors. For example, the authors note that they did not examine factors such as nutrition and stress level in the study. Although Tang et al.,14 Namazi et al.,15 and Martins et al.’s17 studies showed found no significant association between hypertension and vitiligo, Martins et al.17 identified a significantly increased systolic blood pressure in patients with vitiligo. This trend was also demonstrated in an additional study.24 These conflicting results indicate the need for further studies to understand the complete impact vitiligo has on hypertension and ultimately CVD.
Dyslipidaemia is an established risk factor known to promote atherosclerosis and CVD. In patients with vitiligo, Singh et al.’s18 study found increased levels of oxidised LDL and high-sensitivity C-reactive protein, while Azzazi et al.12 and Namazi et al.15 found elevated LDL-C and total cholesterol levels compared with healthy controls. Elevated levels of LDL-C are oxidised into atherogenic particles that, when accumulated, initiate an inflammatory response leading to potential atherosclerotic lesions.25 High levels of high-sensitivity C-reactive protein are shown to be indicators of increased cardiovascular risk, and have been associated with an increased risk of hypertension development.26 Additionally, elevated levels of total cholesterol are associated with increased CVD risk reinforcing the increased atherosclerotic risk in patients with vitiligo.27 Three of the reported studies indicated conflicting results regarding HDL levels. In patients with vitiligo, Azzazi et al.’s12 study showed significantly increased levels of HDL while both Namazi et al.15 and Singh et al.’s18 studies demonstrated significantly decreased levels of HDL compared with controls.15 HDL levels have been shown to be inversely correlated with atherosclerotic events.28 Contrary to the antagonistic role of HDL against atherosclerotic events, many patients who experience cardiovascular events have also shown normal to high levels of HDL cholesterol.28 On the contrary, Rodríguez-Martín et al.’s10 study indicated that patients with vitiligo had higher levels of HDL, lower levels of triglycerides, and no significant difference in LDL levels compared with healthy controls.10 This study ultimately concluded that patients with vitiligo present fewer cardiovascular risks. Further studies measuring lipid profiles in patients with vitiligo are required to confirm the association between patients with vitiligo and lipid profiles, and its ultimate impact on cardiovascular risk.
Ways to Decrease Cardiovascular Disease Risk in Patients with Vitiligo
Bae et al.29 compared the effects of long-term narrowband ultraviolet B phototherapy on cardiovascular (ischaemic heart disease and MI) and cerebrovascular events (cerebrovascular infarction and haemorrhage) in patients with vitiligo.29 They found that the risk for both cardiovascular [hazard ratio: 0.682; 95% CI: 0.495–0.940] and cerebrovascular events (hazard ratio: 0.601; 95% CI: 0.470–0.769) was significantly lower in those who received long-term narrowband ultraviolet B. These findings were consistent with those from clinical trials and in vitro studies that suggest beneficial effects of phototherapy on the cardiovascular system, although the mechanism of action is still unclear. Importantly, this study demonstrated a potential added benefit to phototherapy for vitiligo patients. Future studies may investigate whether such a benefit is present in patients with varying vitiligo severity, and if fewer phototherapy sessions can produce a similar effect.
The authors’ study was limited by a small sample size, which posed challenges in comparing studies due to varying data parameters collected. This led to a focus on a systematic review rather than a meta-analysis, further limiting their study. Additionally, given the genetic and racial differences in vitiligo, the limited racial and ethnic diversity of included studies impacts the study’s generalisability. These highlight the need for additional research in this area. Nevertheless, the authors’ review offers valuable insight into the elevated risk of CVD and cardiovascular events among patients with vitiligo.
CONCLUSIONS
This systematic review provides a comprehensive summary of the association between vitiligo and CVD risk. Through a review of seven case-control and cross-sectional studies, positive associations were observed in CVD risk factors, such as atherosclerosis, dyslipidaemia, oxidative stress, and altered vitamin D, calcium, and zinc levels. While most studies support the association between vitiligo and risk for CVD, conflicting findings were noted when comparing vitiligo’s association with hypertension and lipid profiles. Overall, although this review highlights the emerging link between vitiligo and CVD, future comprehensive research is required to elucidate this intricate relationship.






