Abstract
Objective: To determine the impact of surgical treatment on quality of life (QoL) of patients with early-stage cervical cancer at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya, and Kenyatta National Hospital (KNH), Nairobi, Kenya.
Methods: A cohort study conducted among 71 patients undergoing surgery for surgically amenable cervical cancer stage. Consecutive sampling of females was used to recruit participants. Participants were followed up for 3 months post-operatively. Descriptive statistics was used to describe the study participants. Bivariate analysis was used to assess the relationship between dependent and independent variables, and p value ≤0.05 was considered to be statistically significant.
Results: Nearly two-thirds (63.5%) of the females had a parity of four or more, 69 (97.2%) did not have a family history of cervical cancer, and 57 (80.3%) were negative on HIV test. Most females (47.9%) had Stage IB2 cervical cancer, followed by those with Stage IB1, seen in 28 (39.4%) of the females enrolled. There were statistically significant differences in pain/discomfort (p=0.028) and anxiety/depression (p=0.028). Patients aged 20–35 years had a two-fold increased likelihood (adjusted odds ratio: 2.44; 95% confidence interval: 1.30–3.10; p=0.011) of reporting better QoL scores compared to older females. The lower the cervical cancer stage (Stage IA2), the higher the likelihood for improved QoL following surgical management of cervical cancer (adjusted odds ratio: 5.69; 95% confidence interval: 3.55–6.89; p=0.001).
Conclusion: This study reports that being aged 20–35 years old and having a lower stage cervical cancer increased the likelihood of a good QoL outcome following surgical management of cervical cancer.
Key Points
1. Because of the high disease burden associated with cervical cancer, there is a need to determine whether the current early intervention of radical hysterectomy improves the patient’s quality of life (QoL).
2. The QoL among patients with early-stage cervical cancer after surgery was generally good, indicating an overall improvement of QoL, especially with regard to pain/discomfort and anxiety/depression.
3. There should be more attention and clinical focus in the tertiary facilities of low and middle income countries, offered to patients with cervical cancer who are >35 years, and with Stage IB and above, to improve their QoL by focusing more on addressing their pain/discomfort and anxiety/depression, through a multidisciplinary approach in these patients’ care.
BACKGROUND
Cervical cancer is established as a major cause of morbidity and mortality among females globally.1 In Kenya, and other countries with developing economies within sub-Saharan Africa, it is the second most prevalent cancer after breast cancer among females.2 Because of this huge disease burden, the majority of the females affected are still in their reproductive age, and this raises concerns about their resultant quality of life (QoL). The great disease burden is further compounded by the high prevalence of HIV infections in these countries. Because of the many early detection programmes, such as the see and treat strategy introduced in Kenya and other sub-Saharan African countries, females with cervical cancer are now identified early, and prescribed radical hysterectomy for their surgically amenable cervical cancer.2 However, this procedure is associated with the complete resection of the uterus, parametrium (round, broad, cardinal, and uterosacral ligaments), cervix, upper one-third to one-half of the vagina, and bilateral pelvic lymph nodes.3 The removal of the ovaries and fallopian tube is an integral part of the radical hysterectomy. The ovaries will be removed in post-menopausal females and trans- positioned in pre-menopausal females who may require radiotherapy later on. This may interfere with their perception of wellbeing, especially in the aspect of fertility and childbearing ability, and psychosexual health and wellbeing.4
Complications, such as longer operation time, pain, and side effects of lymph node dissection, like lymphoedema, which reduces the QOL of females who have undergone radical hysterectomy, could influence both the physical (pain, discomfort, low energy and fatigue, sleep disturbance, and medication dependency) and psychological (anxiety and depression) domains.5 Most of the studies conducted in many developing countries have focused on the prevalence and disease burden of cervical cancer, with a few focusing on early screening and interventions for the disease. However, very few published studies have focused on the resultant QoL among females who undergo radical hysterectomy as an intervention for surgically amenable early-stage cervical cancer. This study therefore aims to determine the QoL of these females by assessing both the physical and psychological domains at two national referral and teaching hospitals in Kenya. Because of this huge disease burden, major concerns on the QoL, resulting from both the disease itself and treatment modalities, have been raised.
Most studies done in other populations on the impact of treatment for cancer of the cervix on QoL, evaluated females in all stages of the disease, and included all treatment modalities. This study, therefore, set out to determine the major indicators of QoL among patients with surgically amenable cervical cancer, who had undergone radical hysterectomy at two major national hospitals in Kenya.
The objective of this study was to determine the impact of surgical treatment on QoL of patients with early-stage cervical cancer at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya, and Kenyatta National Hospital (KNH), Nairobi, Kenya.
METHODS
Study Design
This was a prospective cohort study conducted among females with a surgically amenable stage of cervical cancer, and scheduled for radical hysterectomy.
Study Area
The study was carried out at two national hospitals in Kenya, MTRH in Eldoret and KNH in Nairobi. This study was carried out for a period of 17 months from October 2019–February 2021, with each participant followed for 12 weeks after radical hysterectomy to assess the person’s perception of their QoL.
Study Procedure
Females who presented with a histologically confirmed diagnosis of cervical cancer at the gynae-oncology units of both KNH and MTRH were recruited into the study. Appropriate laboratory and radiological investigations, such as a complete blood count, abdominopelvic CT scan, chest X-ray, and renal function test, were done.
Based on their medical history and clinical signs, the International Federation of Gynecology and Obstetrics (FIGO) criteria were used to stage the patients with newly diagnosed cervical cancer. Those who met the criteria of Stage IB2 and below were recruited into the study. After consenting, an interviewer administered a questionnaire that included the EQ-5D-5L to collect participants’ clinical and reproductive characteristics, as well as assessing their QoL prior to surgery. After radical hysterectomy, the participants were followed up after 3 months to determine their post-surgical QoL.
Data Management and Analysis
Data were collected using a structured questionnaire where both participants’ information and QoL score (pre- and post-hysterectomy) were documented. The questionnaire was administered by medically trained research assistants to single out patients before and after surgery.
Descriptive results were computed, and presented in the form of tables for the participants’ sociodemographic characteristics, cervical cancer stage, treatment factors (surgery), and impact of treatment on QoL.
Inferential statistical analysis using bivariate analysis with the Pearson’s χ2 test was adopted to compare the difference in participants’ sociodemographic characteristics and QoL indicators, where a p value of ≤0.05 was considered to be statistically significant.
Ethical Considerations
The MTRH Institutional Research and Ethics Committee and KNH Institutional Research Board reviewed and approved the conduct of this study, and no data collection took place prior to approval.
RESULTS
Sociodemographic Characteristics of Study Participants
A total of 71 participants were recruited into the study. The mean age of the participants was 47.94 years, and most of the participants were aged between 40–50 years old. The youngest was 26 years old, and the eldest 68 years old.
The majority of the participants were married (87.3%), while 7.0% were either single or divorced. A total of 39 (54.9%) had no education or primary education, with 22.5% having secondary education, and the same percentage (22.5%) having tertiary education. Most of the interviewed participants (52.1%) were unemployed, 16.9% were in formal employment, and the remaining 31.0% were running their own businesses or participating in other economic activities, such as farming. Thirty-nine (54.9%) had health insurance. Most of the patients (56.4%) were from the KNH study site. There were no patients lost to follow-up or death during the 12-month study period.
The sociodemographic characteristics are presented in Table 1
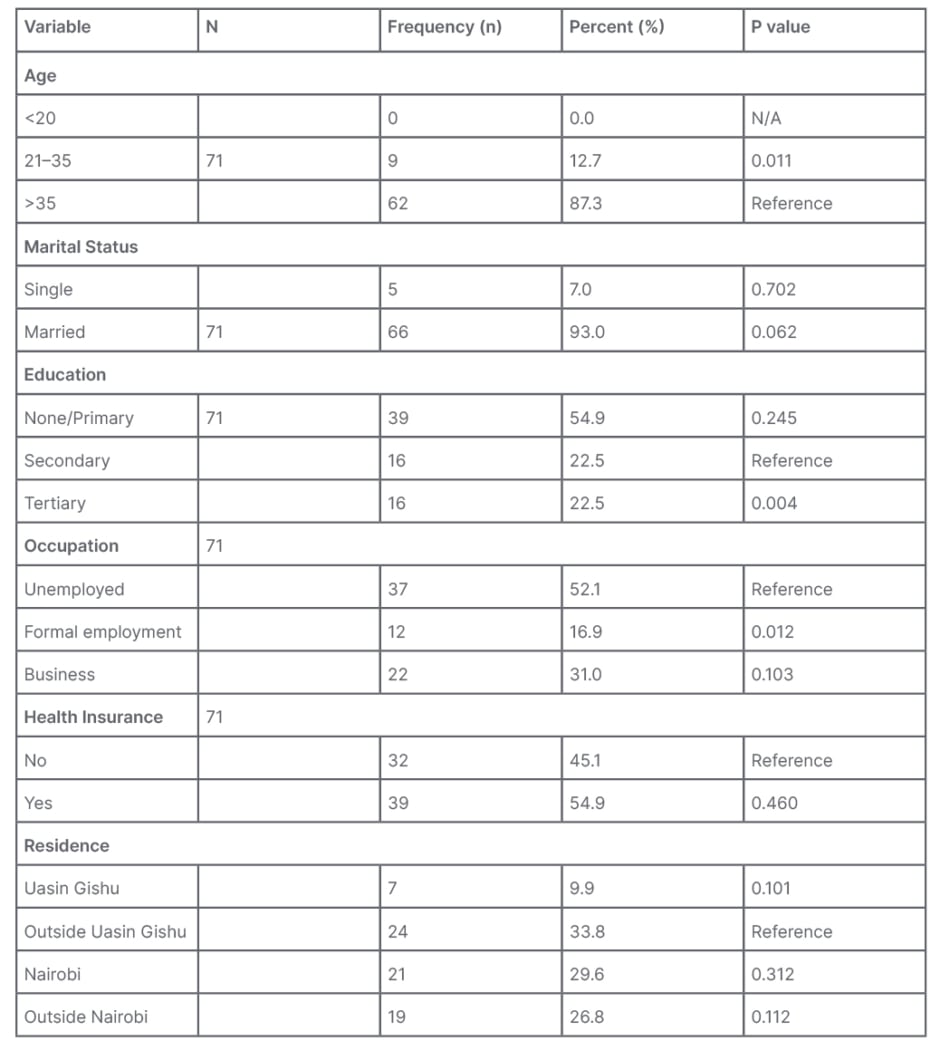
Table 1: Participants’ sociodemographic characteristics (N=71).
N/A: not applicable.
The study conducted a bivariate comparison between participants’ sociodemographic characteristics and QoL improvement. Females aged 21–35 years were significantly (p=0.011) more likely to improve, compared to the older counterparts aged 35 years or higher. Females with a tertiary level of education significantly (p=0.004) reported an improvement in their QoL, compared to those with a secondary and primary level of education. Similarly, formally employed females were significantly (p=0.012) more likely to report an improvement in their QoL, compared to those who were either unemployed or in self-employment.
Clinical Characteristics of the Study Participants
The clinical characteristics of the study participants are shown in Table 2.
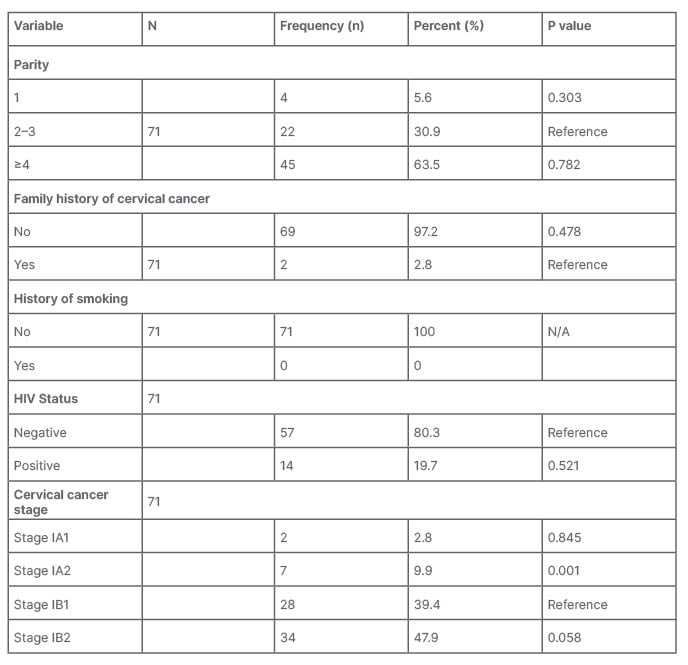
Table 2: Clinical characteristics of patients with early-stage cervical cancer.
N/A: not applicable.
The study further compared whether there was any statistically significant association between the participants’ clinical characteristics and QoL improvement. Females with Stage IA2 were more likely to report a significant (p=0.001) improvement in their QoL, compared to those presenting with all the other early clinical stages of cervical cancer.
Quality of Life of Patients Diagnosed with Cancer of Cervix Pre- and Post-surgical Treatment
A descriptive analysis using the EQ-5D-5L dimensions showed a positive improvement in the QoL score before and after radical hysterectomy on all five dimensions. This was further stratified into five levels: Level 1 (no problems), Level 2 (slight problems), Level 3 (moderate problems), Level 4 (severe problems), and Level 5 (unable to do anything).
The mobility level of patients significantly improved after surgery, as depicted in Table 3. A total of 65 out of 71 of the patients were at Level 1 (91.5%) after surgery, which was a good indicator, as opposed to only 45.1% before, meaning more than half of the participants at a percentage of 54.9% had a poor score (Levels 2–5) prior to surgery.
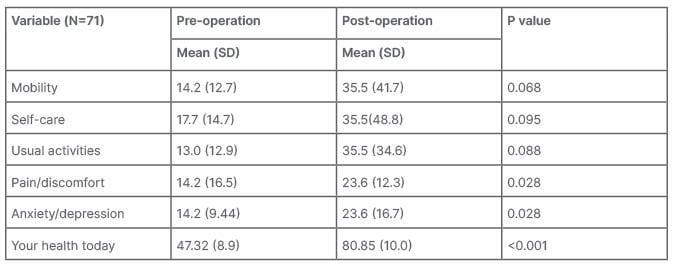
Table 3: Bivariate association of EQ-5D-5L scores pre- and post-radical hysterectomy.
SD: standard deviation.
Descriptive Comparison of Number of Patients in EQ-5D-5L Before and After Surgery in Aspect of Self-Care
In the aspect of self-care, a total of 70 (98.6%) participants were able to take care of themselves without any assistance, as opposed to only 38 participants prior to surgery (53.5%). Therefore, 46.5% of participants had problems with taking care of themselves; however, this percentage comes down to only 1.4% post-operatively, representing improvement.
Descriptive Comparison of Number of Patients in EQ-5D-5L Before and After Surgery in Aspect of Usual Activities
In total, 84.0% of participants had no problems conducting their usual activities after surgery; however, only 22.5% of participants were at the same level pre-operatively. This indicates that 81.5% of participants had problems conducting their usual activities prior to surgery, while that percentage significantly reduced to 15.5% post-operatively.
Descriptive Comparison of Number of Patients in EQ-5D-5L Before and After Surgery in Aspect of Pain/Discomfort
In the domain of pain/discomfort, only 4.2% of participants had no problems with pain or discomfort, meaning that 95.8% of participants had problems, or complained of pain or discomfort, prior to operation. However, post-operatively, 47.9% of participants had no problems with pain or discomfort, while 52.1% still reported or complained of pain or discomfort 12 weeks post-operatively.
Descriptive Comparison of Number of Patients in EQ-5D-5L Before and After Surgery in Aspect of Anxiety/Depression
In the domain of anxiety or depression prior to surgery, 15.5% of participants did not report pain or anxiety, while 84.5% of the participants had problems, or complained of anxiety or depression. Post-operatively, only 60.6% had no problems, or reported no anxiety or depression, meaning that 39.4% of participants still had problems with anxiety and depression.
Therefore, a descriptive analysis of the authors’ results using the EQ-5D-5L dimensions showed a positive improvement between the two time periods. The health state and QoL of the interviewed patients was better after surgery with regard to mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.
The statistically significant sociodemographic and clinical characteristics of the study participants were then fitted into a logistic regression model, where females aged 21–35 years had a two-fold (adjusted odds ratio [AOR]: 2.44; 95% confidence interval [CI]: 1.30–3.10) increased likelihood of reporting an improvement in their QoL compared to their compatriots older than 35 years. Similarly, females with Stage IA2 reported a nearly six-fold (AOR: 5.69; 95% CI: 3.55–6.89) improvement in their QoL outcomes across all five domains assessed, compared to their colleagues with other early stages of cervical cancer. However, after adjusting for the confounders, level of education and being formally employed did not significantly increase the likelihood of better QoL scores (Table 3).
DISCUSSION
Sociodemographic and Clinical Characteristics of Patients Who Underwent Surgery for Early-Stage Cervical Cancer
This study evaluated the QoL among patients with cervical cancer, and its relationship to sociodemographic and clinical variables. Findings from the study established that age, level of education, and occupation influenced the QoL of patients with cervical cancer in the studied settings. The study also established a significant association between the stages of cervical cancer and QoL scores.
Having completed secondary education or higher positively influenced QoL of the patients. Therefore, patients who had primary or no education were the more likely to have a low QoL score, and thus seemed to require more attention and focus from caregivers.
This was consistent with findings of Twahir et al.,2 which reported that patients with higher levels of education were more likely to achieve a better QoL than their counterparts with a lower level of education. The authors’ findings were also supported in a study done in Ethiopia on the QoL in patients with gynaecological cancer who had undergone surgery, which also found an AOR of 4.33 of better QoL in patients with post-secondary education; patients with post-secondary education had a four times better chance of having a good QoL score than their counterparts with primary or no education.
However, these results contrasted with findings from a study that reported higher physical and overall QoL scores among patients with lower levels of education.6,7 This difference could be due to the different coping methods and social support they obtained from family and friends.
Patients who had completed secondary and tertiary levels of education had higher total QoL scores compared to those with lower levels of education. Low levels of education have been associated with decreased awareness of the disease. This often contributes to a large number of females being less likely to be screened early for their cancers, which makes them increasingly present to health facilities in the late stages of their cancers, leading to poor prognosis, hence low QoL scores. These findings are consistent with those by Araya et al.8 reporting higher QoL scores with higher levels of education, while lower levels of education were associated with lower QoL scores in two other studies.
The patients’ occupation was significantly associated with QoL. The formally employed had higher QoL scores compared to their unemployed counterparts. Formal employment is associated with adequate social support based on high income earnings. This finding was consistent with that of Araya et al.8 among patients with cancer, where those with higher levels of employment had higher QoL.
The patients who were formally or self-employed had higher QoL scores compared to those who had no source of income. This finding was consistent with other studies that have reported a significant association between income and overall QoL.
Patients aged 21–35 years had higher QoL scores compared to the older patients. This was consistent with the findings of Chan et al.,9 but contrasted findings from a study by Goker et al.,7 who reported higher physical and overall QoL scores among older Turkish patients with gynaecological cancer.
Patients with Stage IA2 had better QoL scores than those with Stage IB1 and above. This finding was consistent with that of another study,7 where patients who had early-stage cancer had better health status, role function, and social wellbeing than those with advanced cancers. The observed difference could be attributed to good prognosis following early diagnosis and pathogenesis. Normally, females with early-stage ovarian cancer tended to have good prognosis following surgical treatment.
From the regression analysis, age and cervical cancer stage were found to be independent predictors of QoL among patients with cervical cancer in this study. This finding was consistent with those of other studies,7 which identified age, cancer stage, and level of education as predictors of QoL among patients with cancer.
Quality of Life of Patients Diagnosed with Cervical Cancer Pre- and Post-surgical Treatment of Surgically Amenable Stage
This study determined that the majority of the study participants improved in all the five indicators on their QoL. Specifically, nearly all participants were able to move (91.5%), take care of themselves (98.6%), and perform usual activities (84.5%) without any difficulty. However, less than half (47.9%) of the females enrolled did not experience any pain or discomfort, and 60.6% did not report anxiety or depression symptoms.
Previous studies have indicated variability in the participants’ perception to mobility, self-care, and ability to perform usual activities, and this is often affected by the place a participant resides, their occupation, and number of individuals living in their household.10 For instance, participants living in a bungalow or ground-floor of a multistorey building will report less mobility challenges, compared to those living in mansions or higher floors within a multistorey building. The findings of this study match those reported in Indonesia,11 where 77.0% of females enrolled did not experience any difficulties with mobility, 83.9% were able to perform self-care activities without any problem, and two-thirds (66.7%) performed their usual activities with ease. More than half of the participants enrolled in the Indonesian study11 experienced moderate-to-severe problems in their assessment of pain or discomfort, as well as anxiety or depression. It is easier for participants to express pain or discomfort, as well as anxiety, compared to other QoL indicators, such as self-care and usual activities; these are easily confounded by the nature of self-care and usual activity a participant is involved in. Furthermore, the assessment of the first three QoL indicators (mobility, self-care, and usual activities) is not significantly affected by the assessment tool (whether it is EQ‑5D‑3L or EQ‑5D‑5L), as was demonstrated in a Polish general population, and a sample of patients with cancer in Korea.12
The mean values for pre- and post-radical hysterectomy QoL indicators have also been demonstrated to differ based on the assessment tools. In a Dutch retrospective study,13 the mean total EQ-5D utility post-radical hysterectomy score of 81.4 (±24.4) was nearly half that reported in the current study. This could be attributed to the differences in the study designs adopted by these two studies, one being retrospective and the other prospective; differences in the study duration; and QoL assessment questionnaire. It may also be due to sociocultural differences, as this has previously been shown to affect the efficacy of questionnaires. This creates the need for the massive adoption of a universal QoL assessment tool for patients with cervical cancer undergoing radical hysterectomy.
CONCLUSION
The QoL among patients with early-stage cervical cancer after surgery was generally good, indicative of overall improvement of QoL. Specifically, with regard to pain/discomfort and anxiety/depression, there appears to be an improvement in QOL scores post-surgery for early cancer.







