INTRODUCTION
Local excision using transanal endoscopic microsurgery (TEM) for rectal cancer may be considered for selected patients. Management demands assessment of risk of local (LR) and distant (DR) recurrence.
METHODS
In this retrospective study, patients who underwent full-thickness TEM for rectal cancer in western Sweden in a period from 2000 to 2012 were identified through the Scandinavian TEM registry. For reference, Swedish patients who had undergone primary resection of early rectal cancer during the same time period were identified through the Swedish Colorectal Cancer Registry, including non-irradiated patients staged as tumour stage 1 (T1) with any lymph node (N) involvement with tumour height exceeding up to 13 cm from the anus.
RESULTS
A total of 113 patients in western Sweden underwent TEM for rectal cancer (Figure 1); 24 patients underwent completion salvage resection, four patients died post-operatively, and four patients were lost to follow up. Eighty-one patients were followed after TEM-only, with additional radiotherapy in two patients with T2 tumours. Specimens were staged as T1, T2, and T3 in 52, 24, and five patients respectively. Median follow-up was 76 (9–195) months. LR was detected in 19 (23.5%) patients, and DR in 11 (13.6%). Nine patients had both LR and DR.
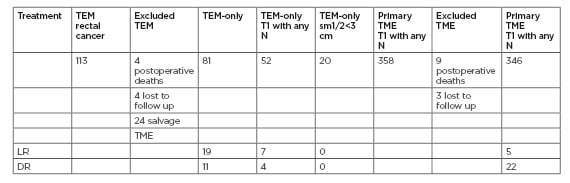
Figure 1: Transanal endoscopic microsurgical outcomes in Scandinavian rectal cancer patients.
DR: distant recurrence; LR: local recurrence; N: nodal involvement; T1: tumour stage 1; TEM: transanal endoscopic microsurgery.
Median time to LR was 13.5 (5–47) months. LR was detected in seven of 52 (13.5%) patients with T1, in five of 22 (22.7%) patients with T1>30 mm, in two of 30 (6.7%) patients with T1<30 mm, in four of 15 (26.7%) patients with T1 submucosal depth of invasion 1/2 (T1sm1/2), in none of 20 (0.0%) patients with T1sm1/2<30 mm, in three of 12 (25.0%) patients with T1sm1>30 mm, and in none of 12 (0.0%) patients with T1sm1<30 mm. In total, 346 patients who had undergone primary resection were selected for reference as described. Median follow-up was 80 (6–196) months. LR was diagnosed in five of 346 (1.4%) patients and DR in 22 of 346 (6.4%) patients.
CONCLUSIONS
TEM resulted in a high LR rate compared to primary resection for early rectal cancer. Recurrence rates differed considerably according to stage and size. T1sm1/2 tumours smaller than 3 cm seem to have a favourable outcome.








