Abstract
Retrorectal neoplasms is a rare, heterogeneous group of neoplasms developing in the retrorectal space. Its rarity makes its management a challenge to the unaware. Here, the authors present a case of 37-year-old female patient presenting with anal pain, diagnosed with retrorectal teratoma, which was managed surgically by posterior approach, the Kraske procedure.
Key Points
1. Retrorectal neoplasms are a rare group of heterogeneous neoplasms that presents a challenge to unaware healthcare professionals, especially as there is limited literature on the condition.
2. The authors detailed the importance of a digital rectal examination on patients with a retrorectal teratoma, highlighting how it allowed physicians to study the mass during surgical planning.
3. Full excision is the aim when surgically removing retrorectal teratomas, with a 0% chance of reoccurance to be expected if a benign tumour is completely excised.
INTRODUCTION
Retrorectal neoplasms is a rare, heterogeneous group of neoplasms that develops in a potential space known as the presacral or retrorectal space. Anatomically, this potential space is enclosed posteriorly by the sacrum, anteriorly by the rectum, superiorly by the peritoneal reflection, and inferiorly by the rectosacral fascia. Although the supralevators and the deep postanal space is not included in this space, lesions occurring within these areas are still generally considered as retrorectal or presacral neoplasms. The estimated incidence of admissions diagnosed by retrorectal tumours is 1 out of 40,000 admissions.1,2 Due to the rarity, management of retrorectal neoplasms poses a challenge to the unaware, manifested by difficulty to diagnose by physicians, difficulty to characterise by radiologists, and a challenge to manage by surgeons. Here, the authors present a case of 37-year-old female patient presenting with pelvic heaviness and dull anal pain, diagnosed with retrorectal neoplas that was resected by posterior approach, with histologic studies showing a mature teratoma.
CASE PRESENTATION
The authors present a case of 37-year-old female patient, previously healthy with no past medical or surgical history, presenting with the complaint of pelvic heaviness and continuous dull anal pain. The patient reported that pain worsened with prolonged standing and towards the end of the day. They denied any anal discharge, blood per rectum, painful defecation, and feeling of incomplete rectal emptiness. There was no family history of malignancy. On physical exam, their vital signs were within normal limits, blood pressure of 120/80 mmHg, and heart rate of 73 beats/min. Neurologic exam was normal, and digital rectal exam revealed a smooth rectal mucosa with a posterior bulge felt displacing the posterior rectal wall anteriorly.
The mass was palpable, starting 1 cm from the anal verge, with its distal end at around 6 cm from the anal verge. Furthermore, a rigid sigmoisdoscopy was completed, showing a bulge in the posterior rectal wall with intact mucosa. Consequently, the patient was scheduled for pelvic CT scan, with intravenous contrast showing a multilobulated cystic mass with several locules and rim enhancement measuring 6 cm in craniocaudal dimension and 3.5 cm in axial diameter (Figure 1). This mass displaced the rectal wall anteriorly and was located below the level of S3 vertebra. Consequently, the patient was scheduled for the excision of retrorectal tumour by posterior approach, the Kraske procedure. In the operating theatre, the patient was put in prone jackknife position, where a paramedian incision was made; coccygectomy was done for better exposure. Dissection continued until the tumour was reached (Figure 2). During dissection, repetitive digital rectal examinations were done, which aids in better surgical exposure and avoids injury to the rectum. Complete excision of the tumour was carried out (Figure 3). The patient had an uneventful hospital stay, and was discharged on Day 1 after surgery. The final histopathology showed mature teratoma with stratified squamous epithelium and regular pseudostratified ciliated respiratory-type epithelium.

Figure 1: Pelvic CT scan with intravenous contrast showing a multilobulated cystic mass with several locules and rim enhancement.
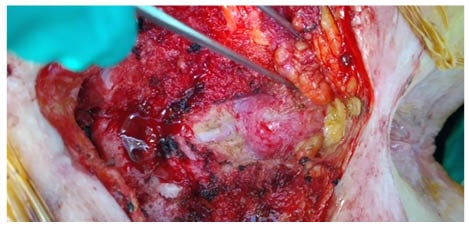
Figure 2: Retrorectal tumour intraoperative.

Figure 3: Complete excision of the tumour.
DISCUSSION
Teratomas have been reported to occur in different anatomical locations, such as the head and neck region, mediastinum, intraperitoneal or retroperitoneal, and in the retrorectal or presacral space. In fact, 11% of retroperitoneal tumours are teratomas and tend to occur in the paediatric age group.3,4
Due to the rarity, retrorectal teratomas present a challenge to the unaware, with the medical literature being limited to case reports and only a scarce large case series. Review of the medical literature revealed a total of 88 reported cases.5-7 Teratomas are considered a true neoplasm, and they include the three germ layers: epithelium of the gastrointestinal tract, respiratory tract, and nervous system. Teratomas can be solid, cystic, and frequently contain both components. Furthermore, teratomas have the potential to undergo malignant transformation to squamous cell carcinoma or rhabdomyosarcoma.8 In fact, the risk of malignant degeneration in an adult population reaches 40–50%, and even higher with incomplete surgical resection.9,10 Furthermore, the tendency of these lesion to adhere to the coccyx mandates at some instances an en bloc coccygectomy.8
Retrorectal teratomas are characterised by their slowly progressive nature. They are frequently incidentally detected during a pelvic or rectal exam from one side or by imaging while investigating another complaint from the other side. Symptoms attributed to retrorectal teratomas are due to the mass effect posed by the tumour. This mass effect is manifested by compression or consequent invasion to adjacent structures, including the pelvic viscera and nerves.8,11
Having said this, patients present with a wide range of symptoms depending on the location of the tumour from one side and the invasion of nearby structures from the other side. These symptoms include low back pain, pelvic heaviness, anal pain, and constipation. Furthermore, if invasion of pelvic nerves happen, rectal incontinence, urinary incontinence, and sexual dysfunction may occur. Moreover, patients may present with urinary tract obstruction.12 On the other end, patients may present with septic complications, including chemical peritonitis due to tumour rupture or abscess formation.13-15 Patients also may present with chemical peritonitis related to dermoid rupture.4,8 Chronic infection of dermoid cysts is a known complication with associated local abscess and fistulous tract formation to adjacent structures, including the skin.12,15
From here, a detailed physical exam, including a neurologic exam to assess for neurologic deficiency, and a digital rectal examination is vital and usually demonstrates an intact rectal mucosa with a posterior extra rectal bulge displacing the posterior rectal wall anteriorly.11 The importance of digital rectal examination is evident for surgical planning. For instance, a digital rectal exam allows the physician to study the extent of fixation of the mass by palpation and its relation to nearby structures. Furthermore, it allows the examiner to realise the proximal and distal level of the tumour, which aids in choosing the best surgical approach. Physical exam in such patients is accompanied by a rigid or flexible sigmoidoscopy, which can be performed to ensure the integrity of the rectal mucosa and the absence of anterior trans mural invasion by the tumour. On the other hand, it is believed that the best imaging modalities to diagnose, characterise, and aid in planning for surgical resection are the CT scan and MRI. These modalities allow the study of the anatomical location of the tumour, and hence determine the surgical approach in conjunction with physical exam. Having said this, the final diagnosis cannot be achieved unless surgical resection is done.3,16
From here, the cornerstone in treatment of retrorectal teratomas is complete surgical resection. The best surgical approach is directly related to the anatomical location of the tumour, the nature, and the size, as well as the invasion of adjacent structures such as the sacrum, the pelvic sidewalls, the rectum, and the anal canal.17 The three most commonly described surgical approaches for resection of retrorectal tumours in medical literature are the anterior approach, either open or laparoscopic, the combined abdominoperineal approach, and the perineal or posterior approach. The main determinant of the surgical approach utilised, along with surgeon preference, is the relation of the tumour to the S3 vertebra. In general, tumours located above the level of S3 will necessitate an anterior or combined approach, whereas lesions located below the level of S3 are excised utilising the posterior approach. Irrespective of the surgical approach utilised for resection, complete excision is the aim. In fact studies have demonstrated a recurrence rate ranging between 0–15% of cases.18,19 However, a recurrence rate of 0% is expected with a complete excision of a benign tumour. this is reinforced by a study published by Glasgow et al.20 demonstrating that the recurrence rate in 22-month follow-up was 0% in completely excised tumours, with a 5-year survival rate of 100%.21 In the authors’ case, the tumour was located inferior to the S3 level, hence a posterior approach was chosen.
CONCLUSION
In conclusion, retrorectal or presacral teratomas are a rare condition with a wide and nonspecific clinical presentation. Such lesions are a challenge to the unaware and are often diagnosed late. Radiologic assessment is a key component in surgical planning that is the cornerstone in treatment of these neoplasms. Treatment should be planned in collaboration between radiologists and surgeons with expertise in pelvic and cancer surgery in order to obtain the best possible outcomes with the lowest recurrence rate, as well as the lowest morbidity and mortality.







