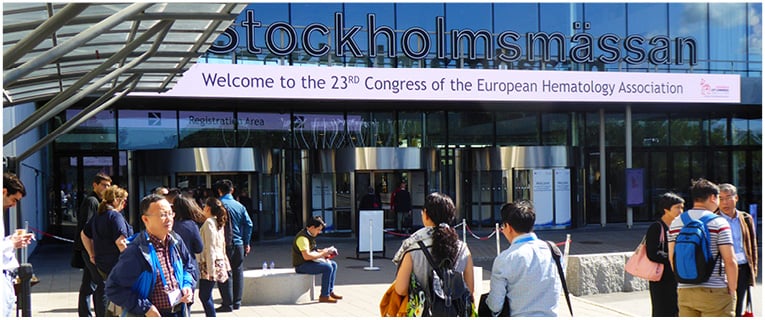
A warm welcome to the EMJ Hematology review of the landmark 23rd annual congress of the European Hematology Association (EHA).
Moving north from the 22nd EHA Congress host city, Madrid, Spain, the 23rd annual EHA Congress arrived this year in the ‘Venice of the North’ and ‘City of Islands’, Stockholm, Sweden, for the first time in 5 years. Home to the Vasa Museum, the Royal Palace, and the world-famous ABBA museum, this June, Stockholm was host to >11,000 haematologists who were hotly anticipating the cornucopia of haematological updates, debates, and discussions that Europe’s flagship haematology congress is renowned for.
The anticipation in the main hall at the Stockholmsmässan Centre was palpable, and that energy was translated into rapturous applause as EHA President Prof Pieter Sonneveld took to the stage. Speaking passionately about the field, Prof Sonneveld praised the work of the organising committee who had produced a scientific programme covering a plethora of haematological disorders, treatments, and hot topics. The programme attracted world-renowned experts to give presentations and lead the interactive plenary sessions, with the aim of combining novel findings and new developments with current care protocols to improve patient care.
The focus of the EHA Congress 2018 was not solely on established haematologists. The YoungEHA committee developed YoungEHA TRACK, a programme specifically for young haematologists to give them the opportunity to get hands-on with the field, meet experts, and attend the Young EHA Research Meeting. The YoungEHA TRACK will surely prove to be a tremendous success, aiding the next generation of field leaders to develop their fledgling careers.
Two new programmes were unveiled during the opening ceremony, the first of which focussing on the rapidly developing field of immunotherapy, which, despite all its impressive potential, must still be scrutinised to ensure patient safety and best practice. The second programme is based on haemoglobinopathies, a broad spectrum of disorders that affect approximately 7% of the global population, with 300,000–400,000 babies born each year with sickle cell anaemia. The goal of the programme is ultimately to improve the curative therapies for these disorders. With the focus of improving research in mind, another new addition to the annual EHA Congress was the Topic-in-Focus session, the aim of which Prof Sonneveld described as: “To raise awareness, provide education, stimulate research, and build a network of experts together with us to improve the care of patients.” A clear theme of this year’s congress was not only the celebration of the field’s achievements and the promotion of new research but also the improvement of patient care and therapies. Prof Sonneveld concluded his speech by stating: “By being here with so many colleagues, ready to share knowledge and ready to work in a sustainable manner, I am convinced that our journey together will lead to a cure for many blood disorders.”
For those of you who were not able to attend this year’s fantastic celebration of haematology, this Congress Review captures the highlights from the event, including the latest updates from a Phase III trial of a new single agent that could change the face of acute myeloid leukaemia (AML) therapeutics. Furthermore, novel results are discussed that show a new, off-the-shelf T cell immunotherapeutic with beneficial effects on post-transplantation lymphomas induced by Epstein–Barr virus. The EMJ reporting team take the history book down from the shelf and provide you with an update on two of the key themes of the congress, immunotherapy and haemoglobinopathies, and the winner does indeed take it all as the prestigious EHA Abstract Awards are celebrated below.
Preparations for the 24th EHA annual congress are already well underway, with the event due to be held from the 13th–16th June 2019 in Amsterdam, Netherlands. The EHA organising committee will be aiming to replicate and build upon their success from this year’s event by attracting more haematologists than ever before. With an exciting year of haematological research and updates ahead of us, the EMJ team is looking forward to what the next 12 months will hold and cannot wait for next year’s congress to celebrate the successes and put haematology back under the microscope.

New Hope for Epstein–Barr Virus-Associated Post-Transplant Lymphoproliferative Disorder Patients
HOPE is in sight for those patients with Epstein–Barr virus (EBV)-associated post-transplant lymphomas, as new results demonstrate a promising safety profile and durable remissions using the new T cell immunotherapy tab-cel™ (Atara Biotherapeutics, Inc., San Francisco, California, USA). Presented in a poster presentation at the 23rd EHA Congress and described in an Atara Biotherapeutics press release dated 15th June 2018, the results of two Phase II studies using tab-cel, also called tabelecleucel, were revealed.
It has long been established that EBV can cause the development of multiple lymphoproliferative disorders. The virus is present in human populations all around the world and asymptomatic infection can persist throughout a host’s lifespan. However, when EBV is present in an immunocompromised host, such as patients receiving solid organ (SOT) or allogeneic haematopoietic cell transplants (HCT), the infection can quickly become life-threatening. This is known as an EBV-associated post-transplant lymphoproliferative disorder (EBV+PTLD).
On average, patients who develop EBV+PTLD following an HCT, who have failed rituximab-based first-line therapy, have a median survival of 16–56 days. In those patients following SOT, the average overall survival for those who have failed on rituximab at 1 and 2 years is 36% and 0%, respectively. Tab-cel offers a new alternative for patients who have failed first-line therapy, both for those with EBV+PTLD as well as other EBV-associated haematological and solid malignancies, such as nasopharyngeal carcinoma.
In the two Phase II studies, it was reported that no patient with EBV+PTLD who responded to tab-cel died as a result of their infection. The 1 and 3-year overall survival in EBV+PTLD patients treated with tab-cel who had failed rituximab treatment following HCT were 68% and 55%, respectively (n=35). In those following SOT, 1 and 3-year overall survival was 64% and 43%, respectively (n=14). Of all the patients who responded to tab-cel treatment, overall survival at 2 years was 83% in HCT patients (n=24) and 86% in SOT (n=7) patients.
These results are significant improvements on the previous overall survival statistics of patients following HCT or SOT. Phase III clinical trials of tab-cel are beginning to confirm the results from these two Phase II trials, but already this new therapy is looking hopeful for patients at risk of this life-threatening infection.
Ruxolitinib Associated with Better Outcomes for Rare Blood Cancer Patients
A PLETHORA of studies have been reported in a Novartis press release dated 15th June 2018, which suggest that ruxolitinib could lead to better outcomes for patients with polycythemia vera (PV) and myelofibrosis (MF) compared to the current best available therapy. With PV affecting up to 3 out of 100,000 people across the world annually1 and this population being vulnerable to serious complications and bleeding,2 these results were much anticipated.
Dr Alberto Alvarez-Larran, Hematology Department, Hospital Clinic, Barcelona, Spain, was the lead author of a comparison study assessing patients in the Phase III RESPONSE trial and the real-world Spanish GEMFINI patient registry, which demonstrated PV patients treated with ruxolitinib who were hydroxyurea-resistant or intolerant had a significantly reduced risk of thrombosis and death compared to those treated with the best available therapy.3 He commented: “When you can complement clinical trial data with real-world experiences, it can provide valuable insight into how treatments affect patients in their day-to-day lives.” He also explained how the results of these trials demonstrate the benefits of prescribing ruxolitinib for PV patients who are unable to tolerate hydroxyurea.
The data were presented at this year’s EHA Congress alongside efficacy and safety analyses of the JUMP trial, which assessed MF patients treated with ruxolitinib. Efficacy analysis demonstrated that patients with lower-risk MF achieved reductions in spleen size following treatment; 82.1% of patients achieved ≥50% reduction at any time.4,5 Additional analysis found that earlier treatment with ruxolitinib, and treatment with a higher dose, could improve spleen response in MF patients.2
Dr Samit Hirawat, Head of Novartis Oncology Global Drug Development, explained: “With limited treatment options, patients with myeloproliferative neoplasms often struggle to keep their disease under control.” He added that these results for both PV and MF are vital for clarifying how ruxolitinib can improve the burden of the disease for patients.
References
- Leukemia & Lymphoma Society. Polycythemia Vera facts. 2015. Available here. Last accessed: 20 June 2018.
- Vannuchi A et al. Results from 48-week follow-up of the EXPAND study: A phase 1b, open-label, dose-finding study of ruxolitinib in patients with myelofibrosis and low platelet counts (50-99 × 109/L) at baseline. Abstract PF611. European Hematology Association Congress, 14-17 June, 2018.
- Alvarez-Larran A et al. Comparison of ruxolitinib real-world best available therapy in terms of overall survival and thrombosis in patients with polycythemia vera who are resistant or intolerant to hydroxyurea. Abstract PF628. European Hematology Association Congress, 14-17 June, 2018.
- Guglielmelli P et al. Safety and efficacy of ruxolitinib (RUX) in patients (PTS) with DIPSS low-risk myelofibrosis (MF) in the Phase 3b expanded-access jump study. Abstract PF623. European Hematology Association Congress, 14-17 June, 2018.
- Gupta V et al. Predictors of response to ruxolitinib (RUX) in patients (PTS) with myelofibrosis (MF) in the Phase 3b expanded-access jump study. Abstract PF616. European Hematology Association Congress, 14-17 June, 2018.
QuANTUM-R Study Results: A New Hope for Acute Myeloid Leukaemia
ACUTE MYELOID LEUKAEMIA (AML) causes approximately 32% of all adult leukaemia cases, and AML patients have the lowest 5-year survival rate of all leukaemia patients, with only around 26% surviving for 5 years post diagnosis.1,2 Mutations in FLT3, the gene that encodes the signal transducing fms-related tyrosine kinase 3, are commonly seen in AML patients. The FLT3-1TD mutation is the most common, affecting 1 in 4 patients; these patients have an increased chance of death and a higher risk of relapse compared with other AML patients. New results from the QuANTUM-R study, however, reported in a Daiichi Sankyo Co. Ltd. press release dated 16th June 2018, could provide a new hope for AML patients.
The aim of the Phase III, open-label, randomised QuANTUM-R trial was to identify whether quizartinib treatment resulted in longer overall survival compared to standard salvage chemotherapy. A total of 367 refractory or relapsed AML patients who were refractory to standard first-line therapy with or without haemopoietic stem cell transplantation or who had relapsed after ≤6 months, who expressed the FLT3-1TD mutation, were enrolled and divided in a 2:1 ratio to receive either the 60 mg (with a 30 mg lead-in) quizartinib treatment or salvage chemotherapy.
The results of the study showed that the patients receiving quizartinib had a 24% lower risk of death when compared with the patients receiving salvage chemotherapy therapy (hazard ratio: 0.76; p=0.0177; 95% confidence interval: 0.58–0.98). Furthermore, the median overall survival for the quizartinib group was higher than the salvage chemotherapy therapy patients, totalling 6.2 months versus 4.7 months, respectively. Extrapolation of these data provided researchers with the estimated survival probability at 1 year of 27% for the quizartinib patients, while the salvage chemotherapy patients had an estimated survival probability of 20%. “In relapsed/refractory AML with FLT3-1TD mutations, these findings represent the first reported clinical data demonstrating that a single agent can significantly improve overall survival, suggesting that quizartinib could potentially help these patients live longer”, summarised Dr Jorge Cortes, Anderson Cancer Center, University of Texas, Houston, Texas, USA.
The median treatment duration in the two arms of the trial was four cycles of 28 days for quizartinib patients and one cycle of salvage chemotherapy for the control group. The occurrence of adverse events in both arms was comparable, with thrombocytopenia, anaemia, and neutropenia being the most common Grade ≥3 disorders. The results of the trial show great promise for the future use of the drug, which will soon be submitted to health authorities for review.
References
- Cancer.net. Leukemia – Acute Myeloid – AML: Statistics. 2018. Available at: https://www.cancer.net/cancer-types/leukemia-acute-myeloid-aml/statistics. Last accessed: 25 June 2018.
- Leukemia & Lymphoma Socitey. Facts 2016–2017. 2018. Available at: https://www.lls.org/sites/default/files/file_assets/PS80_Facts_2016-2017_FINAL.pdf. Last accessed: 25 June 2018.
Better Management in Line for Immune Thrombocytopenia Patients
PATIENTS with immune thrombocytopenia (ITP) may soon experience better management of their disease and symptoms thanks to a new tool developed to improve quality of life in this patient group. According to results presented at the EHA Congress 2018 and reported in a Novartis press release dated 15th June 2018, it is not just the bleeding symptoms of this disease that concern these individuals. The tool, named the ITP Life Quality Index (ILQI), consists of 10 questions that aim to quantify and monitor the quality of life of patients with ITP.
ITP is a rare blood disorder that results in the impaired production and increased destruction of platelets. Patients with the condition often present with bruising, red or purple dots on the skin, bleeding from the gums, nosebleeds, and general bleeding that is difficult to stop. The main treatment goal for ITP patients is to maintain a safe platelet count that results in a minimal risk of bleeding; however, results from the ILQI survey show that patients are experiencing other symptoms that severely affect their quality of life, and that they would like to be treated.
The survey, which is still ongoing, is a cross-sectional online survey that began in January 2018 and has so far included 1,400 patients with ITP and 480 healthcare professionals who treat the disorder across 14 different countries, which were the UK, Spain, Japan, Italy, France, Colombia, Canada, China, Egypt, Germany, India, Norway, Turkey, and the USA. At the time that these results were presented, there were responses from >1,300 patients from 13 countries. There are plans for additional survey results to be released later this year.
The ILQI survey results revealed that for many patients, the factors of the disease that affected them the most were emotional wellbeing (36%) and symptoms that prevented them from working (28%). Another factor was fatigue, with 71% of patients revealing that this was their most severe symptom at diagnosis, and 64% saying this was still the case once they had completed the survey. Dr Nichola Cooper, Hammersmith Hospital, Imperial College London, London, UK, commented on the results: “Severe fatigue, in particular, was reported by many patients as the most difficult to manage symptom of ITP.” She remarked: “This is an important message for healthcare providers treating patients with this rare disease; ITP is about more than bruising and risk of bleeding.”
“Some patients only realise their fatigue has become such an issue in their daily lives after it is corrected by treatment,” Dr Cooper said. She added: “The ILQI tool will help measure this correction more accurately and could also play a crucial role in monitoring disease impact on quality of life beyond just relying on the platelet count alone.” These results will help to improve the standard of care for ITP patients, taking their specific needs into account, while also helping clinicians to better understand their patient’s requirements and provide them with a more personalised style of treatment.

A Brief History of Immunotherapy
Immunotherapy has seen a meteoric rise to prominence across a wide range of medical disciplines for its exciting potential to fight cancer, as well as a myriad of other applications. As a result, it came as no surprise that this therapy featured prominently at the EHA Congress 2018, comprising one of the event’s two main therapeutic focusses, alongside haemoglobinopathies.
This focus was made clear to delegates from the outset of the event, with a very special walkway just beyond the registration area. Taking the form of a tunnel with interactive screens on either side, the walkway’s colourful floor display chronicled immunotherapy’s development through the ages, allowing visitors to literally walk through the history of this exciting field.
Late 19th Century: The Journey Begins…
It is hard to pinpoint an exact date for the inception of immunotherapy; some consider this key event to be rooted in 1867, when German physician Wilhelm Busch noted that a patient’s malignant tumour had disappeared following the contraction of erysipelas. The potential of the immune system to fight malignant cancers was slowly realised from this point on, helped a great deal by Emil von Behring’s Nobel Prize- winning discovery of antibodies in 1890. One year later, in 1891, William Coley was building on the work of his predecessors, injecting heat-inactivated bacteria (so-called Coley’s toxins) into patients with inoperable cancer, demonstrating a reduction in tumour size.
Turn of the Century: Adaptive Immunity is Conceptualised
The next major breakthrough came at the turn of the century (1897–1901), when Paul Ehrlich developed the theory of antibody specificity, for which he would receive a Nobel Prize. The concept of adaptive immunity was born. This idea would prove a significant lodestone in the development of immunotherapies, but it was not until the late 1950s that the field again began to advance at a blistering pace. Immune surveillance of tumours was postulated by Thomas and Burnet in 1959, a concept that would gradually evolve into the ideation of tumour immunoediting.
1960s–80s: Rapid Development and the Rise of Monoclonal Antibodies
The 1960s saw a flurry of immunotherapeutic activity: in 1965, the first allogenic bone marrow transplant was completed in a patient with acute lymphoblastic leukaemia; 1966 saw the discovery of B and T cells; and, in 1969, Wallace Clarke coined the term tumour-infiltrating lymphocytes, suggesting they comprise part of an immune response to melanoma.
Further discoveries blessed the 1970s, including the identification of dendritic cells, natural killer cells, and TNF, to name but a few. However, 1975 proved the real jewel in this decade’s crown when Köhler, Milstein, and Jerne were awarded the Nobel Prize for their method of producing monoclonal antibodies. The next milestone noted the effectiveness of the Bacillus Calmette–Guérin vaccine for the treatment of bladder cancer and, in 1982, the T cell receptor was discovered.
1990s–2000s: First Cancer Treatments Approved
IL-2 was famously the first form of immunotherapy approved for cancer patients in 1992, and 5 years later, rituximab received approval from the U.S. Food and Drug Administration (FDA), becoming a prototype for a vast array of cancer treatments, many of which are still used today. Many more cancer drugs became available throughout the 2000s, notably thalidomide and lenalidomide.
2010–Present: What Does the Future Hold?
The more recent past holds some incredible breakthroughs of its own, with many seminal treatments developed. In 2010, the first autologous cell-based cancer vaccine for prostate cancer was discovered. This year also saw the first successful use of gene-edited T cells for the treatment of haematological malignancies. This decade has seen cancer more accurately defined, including its quintessential ability to evade immune destruction, as well as the advancement of immune checkpoint inhibitor treatment, with anti-CTLA-4 first approved in 2011. Finally, just last year in 2017, we saw chimeric antigen receptor T cell therapy approved for the treatment of paediatric acute lymphoblastic leukaemia; this is a treatment modality that is of growing importance for haemo-oncology and featured prominently in this year’s EHA programme.
The future of immunotherapy is unquestionably bright, and the next breakthroughs are inevitably just around the corner. What those breakthroughs will be is unknown, but one thing is clear: the EHA Congress will champion their development, push them into the spotlight, and carry them into the future of haematological practice.

Haemoglobinopathies
Forming the second main theme of the EHA 2018 annual congress was the broad spectrum of haemoglobin disorders. In his opening speech, EHA President Prof Sonnerveld highlighted that approximately 7% of the world’s population are carriers of the sickle cell trait, and that with 300,000–400,000 babies born worldwide each year with sickle cell anaemia, action is required to combat the growing number of cases of this long-neglected blood disorder. As a result, the EHA organised new Topic-in-Focus sessions, alongside the returning Meet the Expert opportunities that were devoted to an in-depth analysis of various haemoglobinopathies, including both thalassaemia and structural haemoglobin disorders.
There are a number of different diseases that are associated with the amino acid sequences of haemoglobin subunits (4α and 2β), including haemoglobin E, caused by a Glu26Lys mutation; haemoglobin C, caused by a Glu6Lys mutation; and, arguably the most famous, sickle cell anaemia. Thalassaemia can arise from partial or full deletions of the haemoglobin peptide chains, which gives rise to anaemia as well as bone and spleen disorders.
Sickle Cell Anaemia
First identified in 1900, sickle cell anaemia was primarily identified in Asian and African populations. However, since the dawn of the 20th century, the world has become a much smaller place and migration is commonplace; as such, sickle cell anaemia is becoming increasingly more common in northern and western European populations. Germany, in particular, has seen a growth in the number of sickle cell anaemia cases.
Initially described as peculiar, elongated sickle-shaped erythrocytes, it was not until the pioneering work of Dr Linus Pauling in 1949 that it was established that this disease is caused by abnormally shaped haemoglobin protein. Sickle cell anaemia was one of the first disorders to be understood at a biochemical level, but it was not until much later, in the 1970s, that disease therapeutics began to advance more rapidly. One such treatment was the prophylactic administration of penicillin.
A learning session during the EHA Congress was dedicated to furthering the medical community’s current knowledge of anaemic disorders, with the aim of pushing the boundaries of medicine. A special focus was placed on genetics as Prof Douglas Higgs, Weatherall Institute of Molecular Medicine, University of Oxford, Oxford, UK, discussed gene expression regulations and highlighted how genome editing of haematopoietic stems cells can improve treatment. Prof Brigitte Ranque, Hôpital Européen Georges-Pompidou, Paris, France, looked at regional treatment options with a particular focus on sickle cell anaemia progress in sub-Saharan Africa. Dr Miguel Abboud, Department of Pediatrics and Adolescent Medicine, American University of Beirut Medical Center, Beirut, Lebanon, provided his take on the most recent advances detailing the results from the latest clinical trials. In an excellent Meet the Expert session, Dr Karina Yazdanbakhsh, Lindsley F. Kimball Research Institute, New York Blood Center, New York City, New York, USA, detailed her experiences with blood transfusion in patients with sickle cell disease.
Thalassaemia
Dr Thomas Cooley and Dr Pearl Lee, two American paediatricians, first identified Mediterranean anaemia in Italian children in 1925, 25 years after the discovery of sickle cell anaemia. Mediterranean anaemia was linked to an enlargement of internal organs, poor growth, and childhood death. Similar to its sickle counterpart, it was not until the 1940s that understanding of what we now call thalassaemia advanced. In 1943, Dr Ezio Silvestroni and Dr Ida Bianco, two Italian haematologists, identified a disorder they termed microcitaemia. Following the laws of Mendelian genetics and investigating the inheritance of the disorders, it was identified that children developed Mediterranean anaemia, or thalassaemia, if both their parents passed on their microcitaemia genes.
Thalassaemia arises from partial or complete deletions of the α or β haemoglobin chains, causing the body to destroy the red blood cells, resulting in anaemia. A knock-on effect of this response is the production of more red blood cells, inducing a positive feedback loop resulting in bone abnormalities and spleen enlargement.
In the 1960s, doctors first used monthly blood transfusions to ease the symptoms of thalassaemia and increase survival, and since then even more therapeutics have developed, such as folic acid supplementation and iron chelation therapy. With a view to the future, the EHA organised several thalassaemia presentations at this year’s congress, including a panel discussion on clinical decision-making for patients with transfusion-dependent β-thalassaemia and the role of haematopoietic stem cell transplantation for these patients.
The focus of the EHA Congress 2018 was to further drive forward and improve the therapeutic options available to physicians, with the ultimate goal of improving patient outcomes. There were a number of sessions and poster presentations dedicated to the best practice of currently available therapeutic strategies, with a focus on the identification of the next therapeutic breakthrough that could improve patient outcomes many times over. With the ever-growing number of haemoglobinopathy cases, it is clear from presentations given at the EHA Congress that the medical community feels that there is plenty more to be done to combat this broad spectrum of disorders.

Abstract Awards
This year the EHA honoured researchers, physicians, and scientists at all levels for their outstanding contributions to the field of haematology with a range of awards and grants. In addition, the EHA proudly announced for promising young researchers in order to foster the next generation of haematologists. Herein, we summarise the most prestigious awards that were received at this year’s congress and congratulates all the winners for their achievements.
José Carreras Award
The José Carreras Award recognises the very frontrunners of haematological research and is awarded to an investigator who is not only active and well-established in their research but has also made an important contribution to the field. This year, the winner was Prof Francesco Lo Coco, University Tor Vergata Rome, Rome, Italy, who was a driving force in the implementation of arsenic trioxide combined with retinoic acid as treatment of acute promyelocytic leukaemia. Prof Lo Coco joins a select group of researchers to have been recognised with this award since 1999.
David Grimwade Award
The David Grimwade Award is a brand-new award for 2018 and celebrates the outstanding work of basic and translational researchers in haematology. This year, the recipient was Dr Peter Campbell, The Wellcome Trust Sanger Institute, Hinxton, UK, for his work in the field of haematological cancer genetics. As a result of his dedication to this topic, a number of disease-specific driver genes in myeloid cancer, including SF3B1 mutations in myelodysplastic syndrome with ringed sideroblasts, have been discovered, and the way in which tumours develop has been elucidated for the whole medical community. Dr Campbell received his award in the opening ceremony of the congress, where he also gave the David Grimwade honorary lecture.
Jean Bernard Lifetime Achievement Award
This year’s Jean Bernard Lifetime Achievement Award, which was established in 2008 and honours an outstanding lifetime contribution to the advancement of haematology, was awarded to Prof Charlotte Niemeyer, University Medical Center of Freiburg, Freiburg, Germany. Prof Niemeyer is a paediatrician, oncologist, and haematologist and has dedicated her professional career to the study of paediatric myelodysplasia, bone marrow failure, and juvenile myelomonocytic leukaemia. Her translational research works have assisted in the elucidation of the biology and genetic origin of juvenile myelomonocytic leukaemia and have demonstrated the pivotal role of the RAS pathway, which has helped to improve the treatment options for this childhood disease.
Education and Mentoring Awards
The EHA is proud to have become well known for providing high-quality medical education to haematologists the world over. In order to recognise the people who make this education possible through their work contributing to and leading programmes and supporting committees, the EHA this year introduced another brand new award: EHA Education and Mentoring Awards. The first recipients of these exciting new awards were Prof Robin Foá, Sapienza University, Rome, Italy, and Prof Barbara Bain, Imperial College London, London, UK, for their outstanding contributions to the educational programmes of the EHA, as well as to the education of haematologists more broadly.
YoungEHA Best Abstract Award
Young clinicians and researchers were also recognised by the EHA in the YoungEHA Best Abstract Award series. These prizes were awarded to abstract authors in four different categories: clinicians or medical students training for a PhD, PhD research students, postdoctoral fellows, and clinical haematologists. The awards were given at the opening ceremony and the EHA expressed their delight that such esteemed young researchers were presenting their work at the congress. The winners were as follows:
Clinical Trainee Award: R. Shouval, Israel
MD-PHD Award: L. Hinze, Germany
PHD Research Student Award: F. Ribezzo, Germany
Postdoctoral Research Trainee Award: A. Nai, Italy