Meeting Summary
The Kite, a Gilead company, symposium “Beyond Clinical Trials in B-Cell Malignancies: What Real-World Experience Tells Us” took place as part of the 24th European Hematology Association (EHA) Congress and focussed on using real-world evidence (RWE) to complement clinical trial data for B-cell malignancies. Prof New began the symposium by discussing the importance of real-world data, as well as ways in which the data can be collected and used. Prof New continued with the example of the Salford Lung Study, a pragmatic Phase III real-world effectiveness trial that collected large quantities of data from hospital and primary care electronic medical records. This allowed for considerably more data to be collected compared with regular clinical trials. These data were used to provide quick responses to inquiries by regulatory authorities. The symposium was continued by Dr Hoechstetter and Prof Ysebaert, who presented idelalisib clinical outcomes and safety results obtained from both clinical trials and real-world studies. In general, real-world studies of Zydelig (idelalisib) showed similar results to data obtained from clinical trials. Prof Lin presented clinical trial results and real-world data for treatment with YESCARTA▼ (axicabtagene ciloleucel) in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and concluded that data from observational studies support clinical trial data and showed effectiveness and acceptable safety in patient populations who were excluded from clinical trials. Mr McGrath continued the symposium by presenting the European Society for Bone Marrow Transplantation (EBMT) and its involvement in patient registries for haematological malignancies. Mr McGrath showed how EBMT registries formed an integral part of recent approvals of haematologic therapies and how their registries are involved in long-term collection of safety data mandated by regulatory agencies. Finally, Prof New presented the current treatment pathway for new drug development and how this pathway can be improved by using adaptive approaches. Prof New also showed the involvement of adaptive approaches in the recent approvals of chimeric antigen receptor (CAR) T-cell therapies and how these methods led to quicker access of these therapies for patients. He explained that using data already collected during routine clinical care could supplement the data collected by EBMT to provide enhanced safety and effectiveness data for patients, clinicians, and payers.
Defining Real-World Experience
Professor John P. New
Clinical efficacy data are insufficient in today’s treatment landscape, and the multitude of different stakeholders requires supplementary evidence, including a favourable risk-benefit profile, value for the money spent on treatment, as well as effectiveness in larger real-world populations once clinical trials are completed. All these requirements make the development pathway for different regulatory medicines more difficult.
Both the USA1 and European Union (EU)2 regulatory authorities now accept the need for real-world data that can then be processed into RWE. Drugs are tested in small numbers of select patients in clinical trials before receiving marketing authorisation. Upon marketing authorisation, new drugs are used in large numbers of patients, and information can be captured using large datasets with real-world data. These data can be obtained from several sources that include routinely collected hospital data, such as case report forms; admissions data and billing information; data from claims/prescribing databases and disease registry data; and data collected from wearable technologies.1,2
Adherence to medications is very different in randomised clinical trials compared with the real world, with a substantial proportion of patients with cancer being nonadherent to their oncology medications. For example, 26.4% of patients with chronic myeloid leukaemia who were receiving long-term imatinib treatment were not adherent at a median 5 years after diagnosis,3 with similar proportions of nonadherence seen in patients receiving imatinib for gastrointestinal tumours, which is in stark contrast to physician-perceived adherence rates of up to 97.0%.4
The Salford Lung Study was a randomised, pragmatic, Phase III, real-world effectiveness trial in patients with chronic obstructive pulmonary disease. A total of 4,232 patients were randomised to either fluticasone furoate/vilanterol once daily or the standard therapy.5,6 One of the main inclusion criteria was patient consent for the investigators to use all their clinical records, including general practitioner data for the previous 3 years. Compared with randomised controlled trials for which the data footprint spans from the first subject first visit to the last subject last visit, the Salford Lung Study could collect all data from general practitioners and hospitals involved in the study. This was particularly useful for the sponsor when regulatory agents asked for supplementary data regarding events of pneumonia for regulatory approval in asthma. Although this information was not part of a prespecified endpoint, data were available and could be analysed and provided to the regulators within 3 months of the request.
RWE has been pivotal in recent regulatory submissions and is particularly important in rare diseases for which the number of patients is insufficient or where patients have an extremely poor prognosis. Recent drugs in the haematology field for which RWE data have been extremely important in initial regulatory decisions, post-marketing extension of indications, and post-marketing commitments include Yescarta®▼ (the efficacy results were benchmarked against historical control data sets such as SCHOLAR-1, and post-authorisation safety study [PASS] will be set up), Kymriah®▼ (efficacy results were compared against three external data sets [SCHOLAR1, the CORAL extension study, and PIX301], and PASS and efficacy study will be implemented), Zalmoxis®* (EBMT registry was used as a control group, and a PASS is ongoing), Strimvelis®▼ (PASS), or Soliris® (where upon the results of a global paroxysmal nocturnal haemoglobinuria registry a modification in the label was attained to extend the indication regardless of transfusion history).2
However, the use of real-world data also faces challenges such as data access, protection, sharing, and completion; inconsistent use of terminology; as well as potential biases and confounders that are not always captured, although possible solutions exist to all these problems.2
In summary, real-world data are playing an increasing role in healthcare decisions and can complement data from clinical trials to help inform patient care,2 and regulatory agencies use real-world data for regulatory decisions and post-marketing safety monitoring. With appropriate consent, this RWE can provide additional insight into the safety and effectiveness of new treatments. Such information should be collected in classification and regression tree algorithms to demonstrate their longer-term safety and effectiveness. Real-world data can be used for clinical trial design development and observational studies, with electronic health records facilitating simultaneous data collection and safety monitoring without direct patient contact for large populations.5,7
Real-World Experience with Phosphoinositide 3’-Kinase δ Inhibitor Therapy in Follicular Lymphoma and Chronic Lymphocytic Leukaemia
Doctor Manuela Hoechstetter and Professor Loïc Ysebaert
The presentation was started by Dr Hoechstetter by describing the efficacy of idelalisib, which is a first-in-class, selective, oral, phosphoinositide 3’-kinase δ (PI3Kδ) inhibitor that acts by decreasing downstream signalling of the B-cell receptor and cytokine receptors (CXCR4, CXCR5, CXCL12), critical components of signalling pathways in B-cell malignancies.8 Idelalisib is approved in Europe for chronic lymphocytic leukaemia (CLL), in combination with rituximab or ofatumumab for adult patients with ≥1 prior therapy or as first-line therapy in the presence of del(17p)/TP53 mutations in patients not eligible for any other therapies.9 Idelalisib is also approved as monotherapy for follicular lymphoma (FL) in adult patients refractory to ≥2 treatment lines.9 European Society for Medical Oncology (ESMO) guidelines currently place idelalisib plus rituximab as a treatment option for patients with relapsed CLL10 and idelalisib monotherapy for double-refractory FL.11
Study 116 was a randomised, controlled, Phase III trial of idelalisib plus rituximab versus rituximab alone (N=220) in patients with early relapsed CLL, medical comorbidities, and limited treatment options.12 Patients enrolled in Study 116 could continue to receive idelalisib in the extension Study 117. In these trials, the median progression-free survival with idelalisib plus rituximab was 19.4 months versus 6.5 months for rituximab alone, whereas the median overall survival (OS) was 40.6 months for patients who received idelalisib plus rituximab and 34.7 months for patients who received rituximab.13 An analysis of patients stratified by del(17p)/TP53 mutation status showed no impact on idelalisib plus rituximab clinical outcomes (p=0.9012).13 In the separate Study 101-09, idelalisib monotherapy also showed clinical benefit in patients with heavily pretreated FL, with an 11.0-month progression-free survival compared with 5.1 months with the prior regimen.14
Real-world data showed similar results compared with trial data. Retrospective data from the Polish Adult Leukemia Group in patients with relapsed/refractory CLL (N=34) showed similar OS results to Study 116/117 data,15 whereas retrospective data from the UK and Republic of Ireland showed similar clinical benefit to trial data both in patients with CLL16 and FL.17 A prospective real-world data study to assess the use of idelalisib in routine clinical practice was conducted in Germany. After a median observation time of 11.5 months in the CLL cohort (N=84), the median OS was not reached, whereas the 12-month survival rates for patients with and without TP53 aberrations were 81.0% and 83.0%, respectively. Furthermore, the PASS study also showed that prophylactic treatment for Pneumocystis jirovecii pneumonia (PJP) improved survival, with 12-month OS rates of 84.0% versus 76.0% in patients with and without prophylaxis, respectively.18
The presentation was continued by Prof Ysebaert, who summarised safety data of idelalisib collected both in clinical trials and real-world studies. In clinical trials, treatment discontinuation due to adverse events occurred in 25–29% of patients.13,14 The most common adverse events occurring both in patients with FL and CLL were diarrhoea/colitis, increased liver transaminases, neutropenia, and infections.13,14 Pooled data from multiple idelalisib trials showed that prophylactic treatment for PJP infection is required.19 Currently, the European Medicines Agency (EMA) recommends prophylaxis to be used in all patients throughout idelalisib treatment, and for a period of 2–6 months after discontinuation.9 Other common adverse events leading to discontinuation can be occasionally managed by re-challenge with a lower dose. Based on clinical trial data, 41% of patients with interruptions due to Grade 3 diarrhoea/colitis and 83% of patients with Grade 3 transaminase elevations were successfully re-challenged and continued treatment.13
Published real-world data generally support safety findings from clinical trials. Retrospective data from the UK and Republic of Ireland that included patients with a performance status ≥2 revealed the same pattern of adverse events as in the clinical trials, but at lower rates.17,18 Furthermore, a French retrospective, multicentre survey study of idelalisib patient management showed similar adverse event profiles in patients with FL (n=145) and CLL (n=384) compared with clinical trial data, but with larger discontinuation rates due to adverse events.20 In this French retrospective study, multivariate analyses showed that good performance status and anti-PJP prophylaxis were associated with longer treatment duration.20 Furthermore, patients who had at least one nurse follow-up tended to have a longer treatment duration both in FL and CLL, demonstrating the importance of nurse follow-up on patient persistence in voluntarily taking the treatment.
In summary, the efficacy and safety of idelalisib were established in clinical trials. Consistent with trial data, several years of RWE showed similar clinical outcomes with no new safety signals. Finally, anti-PJP prophylaxis should be administered to all patients receiving idelalisib, neutrophil count and CMV surveillance is recommended, and nurse consultations may help with increasing patient adherence to treatment.
Real-World Experience with Chimeric Antigen Receptor T cells in Aggressive Non-Hodgkin’s Lymphoma
Professor Yi Lin
The SCHOLAR-1 retrospective study used pooled data from clinical trials and observational studies in relapsed/refractory DLBCL, and showed a median OS of 6.3 months, a 2-year OS of 20%, and a complete response (CR) rate of 7%,21 demonstrating a high unmet need in these patients. However, recent developments in CAR T-cell therapies have brought a new viable option for these patients.
The pivotal multinational ZUMA-1 trial enrolled patients with refractory DLBCL, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, or transformed FL. Patients enrolled in the study underwent leukapheresis for manufacturing of CAR T cell and received lymphodepleting chemotherapy followed by treatment with axicabtagene ciloleucel (2×106 anti-CD19 CAR T cells/kg body weight). A total of 111 patients were enrolled and underwent leukapheresis. The manufacturing success rate of the treatment was 99%, and 91% of patients received treatment.22 After a median follow-up of 27.1 months, the overall response rate (ORR) and CR per independent central review committee among treated patients were 74% and 54%, respectively, and the median OS was not reached.23 The most common adverse events included cytokine release syndrome (93%; 11% Grade ≥3) and neurological events (67%; 32% Grade ≥3).23 The majority of these common adverse events were reversible and can be managed with established protocols and informed management.24
Retrospective studies of real-world practice have reported that patients who did not meet the eligibility criteria from the pivotal ZUMA-1 trial have been treated with axicabtagene ciloleucel, including patients with an Eastern Cooperative Oncology Group (ECOG) performance status >1, thrombocytopenia (<50,000/µL), reduced kidney function (serum creatinine >1.5 mg/dL), liver abnormalities (serum alanine transaminase/aspartate transaminase ≤2.5 ULN; total bilirubin ≤1.5 mg/dL), or a history of central nervous system lymphoma. In all patients evaluable after 30 days of treatment (n=112), the ORR and CR per investigator assessment were 79% and 50%, respectively, whereas in patients evaluable after 100 days (n=39), the ongoing response and CR were 59% and 49%, respectively. Grade ≥3 cytokine release syndrome occurred in 7% and neurological events in 31% of evaluable patients (n=163). Despite the inclusion of patients with clinical characteristics outside of pivotal trial eligibility, the safety and efficacy results were similar compared with ZUMA-1 results.25 Another USA retrospective cohort analysis showed that axicabtagene ciloleucel-treated patients (N=73) had a best ORR and CRR of 64% and 41%, respectively, at a median follow-up of 4 months, with Grade ≥3 cytokine release syndrome and neurological events observed in 17% and 38% of patients, respectively.26 Finally, another retrospective analysis performed at a single USA centre showed similar response rates with the same adverse event profile for patients younger and older than age 65, indicating that an age >65 did not preclude treatment with axicabtagene ciloleucel.27
Navigating the logistics of upfront insurance approval, pre-treatment evaluation, and leukapheresis can impact access to axicabtagene ciloleucel. In the USA, a single-centre study looking at the experience with 13 patients showed that the median time from patient referral to autologous anti-CD19 CAR T-cell infusion was 37 days (range: 31–80) days, which included a median 12 days for insurance approval, showing that opportunities still exist to decrease the pre-treatment timelines for these patients, which can also be variable across different health systems.28 Furthermore, a survey conducted at 26 certified centres to prescribe CAR T-cell therapies showed that product logistics (including manufacturing time) influenced prescribing practices in 84% of centres, whereas the single most important reason informing treatment decisions was the adverse event profile (32% of centres).29 This survey also showed a considerable heterogeneity in the use of the different toxicity grading systems and management.
In conclusion, anti-CD19 CAR T-cell therapy is an effective treatment option in patients with relapsed/refractory DLBCL. ZUMA-1 showed high rates of durable responses with axicabtagene ciloleucel, and early real-world studies supported the results of the trial and showed promising safety and efficacy results in a broader patient population.
Harnessing the Power of Patient Registries
Mr Eoin McGrath
The EBMT is a Dutch-registered, non-profit organisation that includes 583 centre members located in 63 different countries, comprising a total 2,898 physicians, 826 nurses, and 645 data managers.30 The EBMT was established in 1974 and currently contains data for over 666,000 haematopoietic stem cell transplants, with information on more than 40,000 haematopoietic stem cell transplants included in 2018 alone.30
The interests of the registry users include science and education, quality control of clinical care, and safety surveillance, which is of importance to clinicians, regulators, and corporate sponsors (Table 1). The benefits of patient registries include case identification for prospective and retrospective studies, real-world assessment (therapy effectiveness), risk factor insights, improved patient management, healthcare services assessment, patient subgroup evaluation, and institutional benchmarking.31
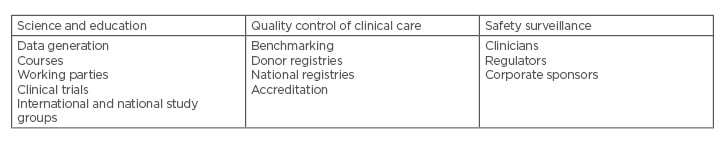
Table 1: Interests of registry users.
As more and more patients are becoming survivors of cancer, long-term follow-up is needed, which is often not performed as part of clinical trials. As an example, several large cohort studies have shown an increase in secondary malignancies and cardiovascular disease following radiotherapy and chemotherapy, which were not captured as part of clinical trial monitoring.32 Furthermore, registries can also offer a ‘neutral ecosystem’ for monitoring the impact of novel drugs on treatment choices. Patient registries also come with several challenges, including quality management, data analysis (that can introduce bias), data security including General Data Protection Regulation (GDPR) compliance, validity of results, long-term retention, and patient follow-up, as well as in the assessment of adverse events.33
Registry data have been useful to provide control patients for EMA assessment of a single-arm pivotal trial. Zalmoxis* treatment was assessed in a pivotal single-arm Phase I/II trial; because no control arm was included, retrospective match-pair analyses comparing trial patients with patients receiving standard of care and included in the EBMT registry were essential for marketing approval of Zalmoxis*.34 Furthermore, data from the pivotal single-arm ZUMA-1 trial of axicabtagene ciloleucel was also compared with historical controls based on pooled analyses in patients with refractory non-Hodgkin’s lymphoma included in the SCHOLAR-1 analysis, leading to marketing approval.35
Registries can be well placed to collect data for cell therapies, with manufacturers, payers, regulators, and clinicians all benefiting from these data. In the case of CAR T cell therapy approval by EMA, post-authorisation systems and risk mitigation strategies were specific requirements.35 A similar registry from the Center for International Blood and Marrow Transplant Research (CIBMTR) is being implemented in the USA.36 Based on EMA requirements, data from CAR T patients could be centralised in one registry to permit one point of reporting and data access for EU clinicians, and for supporting specific studies.36
In summary, the use of patient registries for CAR T-cell therapies may change the lifecycle paradigm for future advanced therapy medicinal products. These patient registries were built by clinicians for clinicians to allow centralised data collection that can inform clinical decisions and serve to enhance patient care. A CAR T-cell therapy registry is needed for collecting data and performing pharmaco-epidemiological studies. Collaboration between the registry and all stakeholders, including clinicians, regulators, payers, and sponsors, is the key to future success.
Using Real-World Experience in Future Drug Development
Professor John P. New
The current EU trial pathway can be slow and costly. Preclinical testing followed by clinical trials can take between 9 and 13 years, which is followed by regulatory and payer approval of the new therapy, which can take another 2–5 years, for an approximate total cost of medicine development of $2–4 billion. Patients can only have access to the new therapy once the process is complete.37 Timely access to a promising treatment is relevant for any serious disease, regardless of its time course. In case of certain diseases, such as hypercholesterolaemia or dyslipidaemia, a long development timespan might not have a high impact for patients because the evolution of the disease towards major cardiovascular events is slow. This is not the case for patients with diseases like cancer for which quick access to new therapies is essential due to the high disease mortality.38
External influences are pushing for a transition towards new drug development pathways that can lead to improved and quicker medicines for patients. First of all, patients demand timely access with an emphasis on diseases with an unmet need; second, emerging scientific research has led to a fragmentation of treatment populations based on genotypic biomarkers and early disease interception; third, the high costs of new therapies has led to a rise in payer influence; and finally, all these factors have placed pharmaceutical sponsors under pressure affecting the sustainability of drug development.38
The adaptive pathways approach to the drug development lifecycle may provide patients with timely access to beneficial medicines, by identifying patients most likely to benefit from new therapies and to adequately determine the evolving information on the risk-benefit ratio.38,39
Furthermore, the adaptive pathways approach can also involve a transition in the way the research and development roadmaps are set up. The traditional development strategy starts with a large population, aiming to obtain an approval licence as broad as possible, followed by later assessment of patient subgroups that can derive the highest benefit from treatment; the adaptive pathway strategy would have an initial goal of showing a positive benefit-risk ratio in subpopulations with a high unmet need, and further studies would follow to support broader coverage and other indications.38
Axicabtagene ciloleucel and tisagenlecleucel were the first therapies to be supported through the EMA PRIority MEdicines (PRIME) scheme to receive marketing authorisation based on small, single-arm studies with small patient populations with a high unmet need. Key risk management steps were advocated as part of the authorisation, including the mandatory utilisation of a patient registry to monitor long-term clinical benefit and safety, and a post-authorisation safety surveillance programme will report data until 2038.35,40 The use of electronic medical record data to demonstrate longer-term safety and efficiency of new treatments will provide essential information in the adoptive licensing process.
In conclusion, the current EU trial pathway can be costly and slow, but regulators are looking into new ways to balance the needs of patients, needs for safety, and the needs of the corporate trial sponsors. Adaptive approaches to drug development using RWE to determine the safety profile will ultimately help patients with a high unmet need receive new treatments in a timely manner.







